Abstract
Aims: Optimal ostial seating and adequate back-up of guide catheters are required for challenging percutaneous coronary interventions (PCI). The GuideLiner™ (GL) (Vascular Solutions Inc., Minneapolis, MN, USA) is a guide catheter extension system that provides active back-up support by deep coronary intubation. We aimed to assess feasibility and safety of GL-use in routine clinical practice.
Methods and results: We prospectively recorded patient and procedural details, technical success, and in-hospital outcome of 65 consecutive patients undergoing “5-in-6” Fr GL-facilitated PCI of 70 target vessels. The GL was mainly used for PCI of complex coronary lesions: 97% (68/70) had American Heart Association/American College of Cardiology (AHA/ACC) lesion types B2/C; 53% (37/70) were distally located; and 23% (17/70) were heavily calcified. Indications were to increase back-up of the guide and facilitate stent delivery (59%; 41/70), achievement of coaxial alignment of the guide catheter (29%; 20/70), and selective contrast injections (13%; 9/70). Device success rate was 93% (65/70). There were no major complications and two minor complications managed without clinical sequelae: one air embolism and one stent dislodgement.
Conclusions: GL-use resulted in increased back-up and guide catheter alignment for stent delivery in unfavourable tortuous coronary anatomies and complex, heavily calcified, and often distally located lesions, which otherwise may have been considered unsuitable for PCI. Procedural success rate was high and there were no major complications.
Abbreviations
ACS: acute coronary syndrome
CK: creatine kinase
CTO: chronic total occlusion
DES: drug-eluting stents
GEA: gastroepiploic artery
GL: GuideLiner
LAD: left anterior descending coronary artery
LCX: left circumflex coronary artery
LM: left main
NSTEMI: non-ST-elevation myocardial infarction
PCI: percutaneous coronary intervention
STEMI: ST-elevation myocardial infarction
RCA: right coronary artery
UAP: unstable angina pectoris
Introduction
Despite the advancements made in percutaneous coronary interventions, the interventional cardiologist nowadays has to deal with an increasing complexity of procedures. A good back-up of the guide catheter is essential to advance guidewires and balloons, and to deliver stents. Support of the guide can be increased by use of extra back-up guides and larger guide dimensions. In addition, the stability of the guide can be improved by advancing a buddy wire, and use of stiffer guidewires or anchoring balloons1,2. Another way to increase back-up support is deep intubation of the guide3,4. There is, however, a considerable risk of dissecting the vessel. Introduction of guide catheter extension systems, in which a long guide catheter with a flexible tip is advanced through the mother guide, has further refined this concept5-7. Besides the improvement in back-up support, the use of guide catheter extensions provides selective visualisation of the target vessel, improves the stability of the guide and allows coaxial alignment of the guide.
There are three systems available: the Heartrail® II catheter (Terumo Corp., Tokyo, Japan), the Proxis™ device (St Jude Medical, St Paul, MN, USA) and the GuideLiner™ catheter (Vascular Solutions Inc., Minneapolis, MN, USA). The Heartrail® II catheter and Proxis™ device are 120 cm catheters that are introduced into the mother guide by removing the Y-connector6-9. The GuideLiner (GL) catheter (Figure 1) is a novel rapid exchange guide catheter extension system that provides active guide support by its 20 cm-long flexible tubular end, which can be deeply advanced into target vessels10-18. Its handling is particularly easy, as it is does not require disconnection of the haemostatic valve at the proximal end of the guide catheter and is compatible with standard 180 cm-long guidewires. Its soft distal tip promises a low risk of dissecting vessels compared to the deep-seating of regular guide catheters.
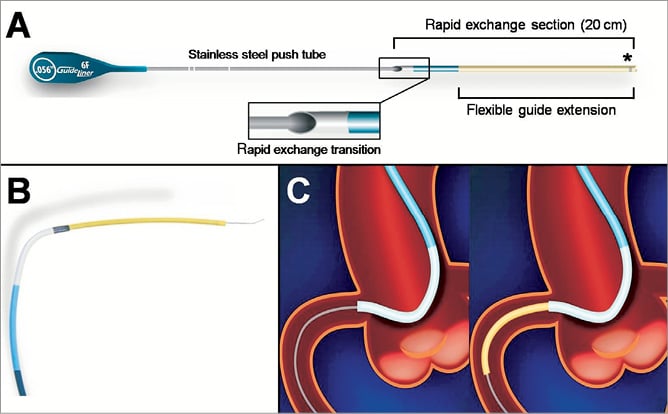
Figure 1. Schematic presentation of the GuideLiner catheter.
So far, only a limited number of reports and case series have been published on the GL guide catheter extension10-18. Mamas et al reported a case series of 13 complex coronary interventions, performed via the radial artery with the “5-in-6” Fr GL system10. Although their success rate was high, the main limitation encountered was stent damage upon advancement of the stent across the metallic collar of the GL (two out of 32 stents)10. Recently, Luna et al published their experience with the GL catheter in a series of 21 patients15. In their study, a transfemoral approach and 7 Fr guide catheters were used in the majority of the cases with a procedural success rate of 90%. Pressure dampening was seen in 57% of their patients, contributing to three out of four unsuccessful cases. There was one major complication in the series reported by Luna et al, which was a flow-limiting dissection in the proximal left anterior descending coronary artery (LAD) but they noted no case of stent damage15. The purpose of the present Twente GuideLiner registry was to assess feasibility and safety of use of the “5-in-6” Fr GL guide catheter extension system during routine, clinical PCI procedures as performed at Thoraxcentrum Twente, a high-volume PCI centre located in Enschede, The Netherlands.
Methods
STUDY POPULATION
Between November 2010 and July 2011, we prospectively collected data from a consecutive series of 65 patients, in whom the GL was applied to facilitate routine PCI. The patients had a background of stable or unstable angina pectoris, or presented with an acute myocardial infarction.
INTERVENTIONAL PROCEDURES
A team of five interventional cardiologists performed the PCI procedures; each of them had performed PCI for more than five years (250-500 PCI procedures per operator annually; total PCI experience of 4,000 or more per operator). PCI procedures were performed according to standard clinical protocols via the femoral or radial routes, using 6 Fr guide catheters as a standard. All patients received a bolus of unfractionated heparin (5,000 IE or 70-100 IE/kg). Prior to PCI, all patients received adequate loading doses of acetylsalicylic acid (300 mg) and clopidogrel (300-600 mg), if not pretreated. During the procedure, an intracoronary bolus of nitrates was administered. The choice of interventional approaches, devices, and techniques was left at the operators’ discretion, considering current clinical protocols and guidelines. Following PCI, clopidogrel was prescribed for one year (75 mg once daily [o.d.] in addition to life-long treatment with acetylsalicylic acid [at least 100 mg o.d.]).
THE GUIDELINER CATHETER AND ITS USE
The GL (Vascular Solutions, Minneapolis, MN, USA) consists of a flexible, 20 cm, straight, flexible, soft-tipped extension tube that is connected via a metal collar to a thin 115 cm-long stainless steel shaft (Figure 1A and Figure 1B). The extension tube has a silicon coating for lubricity. The procedure starts by positioning the mother guide and advancing the guidewire across the target lesion. Then the GL is advanced over the guidewire through the haemostatic valve of the Y-adapter (handling comparable to regular balloons) to intubate the target coronary artery or bypass graft (Figure 1C). The GL reduces the inner diameter of the mother guide by approximately 1 Fr, but it does not lengthen the guide outside the patient. When the GL is in place, balloons and stents can be delivered over the same initial guidewire. The GL is available in sizes of 6 Fr, 7 Fr, and 8 Fr. In this study, only 6 Fr GL were used (also called the “5-in-6” Fr system), which has an internal diameter of 0.056” (1.422 mm). Notably, the use in vessels <2.5 mm is discouraged by the manufacturer. Bifurcation lesions in our study were treated as follows: two wires were advanced through the guide. Then, the GL was advanced over both wires simultaneously. Provisional stenting was the strategy of choice. In cases where a kissing balloon technique was demanded, a wire exchange was performed followed by balloon dilation of the side branch through the stent struts. Before the final kissing balloon inflation could be performed, the GL had to be removed.
STUDY PARAMETERS AND DATA ACQUISITION
To assess the usefulness (feasibility and safety) of the GL in clinical practice, we prospectively recorded various procedural data and clinical details on the in-hospital outcome of a consecutive series of 65 patients, who underwent PCI with the use of the GL. Patient demographics, indication for GL use, angiographic and procedural details including technical success, and all complications were recorded. Quantitative coronary angiography (QCA) was used to determine the intubation depth of the GL catheter. Procedural success was defined as the achievement of <20% diameter stenosis with TIMI 3 flow in the target vessel. Routine peri-interventional assessment of cardiac biomarkers was performed to screen for PCI-induced myocardial necrosis up to 24 hours after PCI or until the highest value of creatine kinase (CK) was measured. Peri-PCI myocardial infarction was defined as two times the upper reference limit of CK, confirmed by significant elevation of other specific biomarkers (MB-fraction of CK or troponin).
STATISTICAL ANALYSIS
Values are expressed as mean±SD. Comparison of continuous variables was performed with the Student’s t-test. Categorical variables are presented as numbers or percentages and were tested with the chi-square test or Fisher’s exact test. A p-value <0.05 was considered statistically significant. Statistical analysis was performed with SPSS version 15.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
PATIENT POPULATION AND LESION CHARACTERISTICS
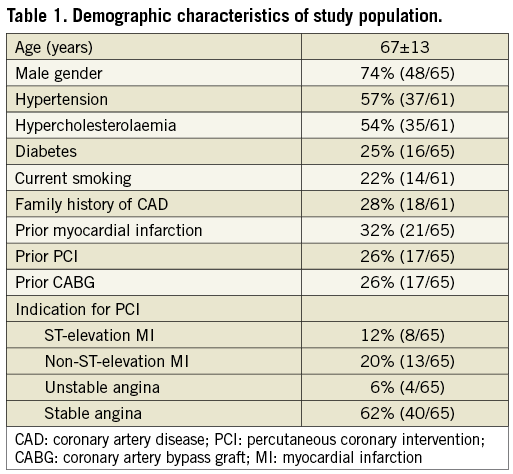
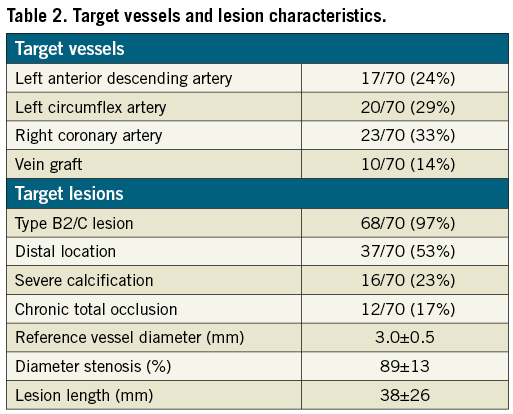
The demographic characteristics of the study population are presented in Table 1. The majority of patients were male (74%), and the mean age was 67±13 years. Target lesions were relatively complex as is shown in Table 2. Most lesions (97%) had American Heart Association/American College of Cardiology (AHA/ACC) lesion types B2 or C, with more than half of them being located in distal vessel segments. A total of 90% of lesions was classified as being calcified: 67% mild to moderately and 23% heavily calcified. Mean lesion length was 38±26 mm, which is indicative of long lesions.
INDICATION FOR GL USE AND PROCEDURAL DETAILS
All procedures were carried out with the “5-in-6” Fr GL device. As shown in Figure 3, the primary indications for GL use were to increase back-up of the guide catheter, in general to facilitate stent delivery (59%), and to improve alignment of the guide catheter (29%) (Table 3). In a few patients (13%), the GL was used for selective contrast injection, predominantly because of dominant left coronary artery (LCA) and/or renal impairment. There were differences between the application in right coronary artery (RCA) and LCA interventions. In the LCA, the GL catheter was used regularly to improve the alignment of the guide or enhance selective contrast injections, whereas its use in RCA interventions was mainly to increase catheter back-up (p=0.024). An example is shown in Figure 2.
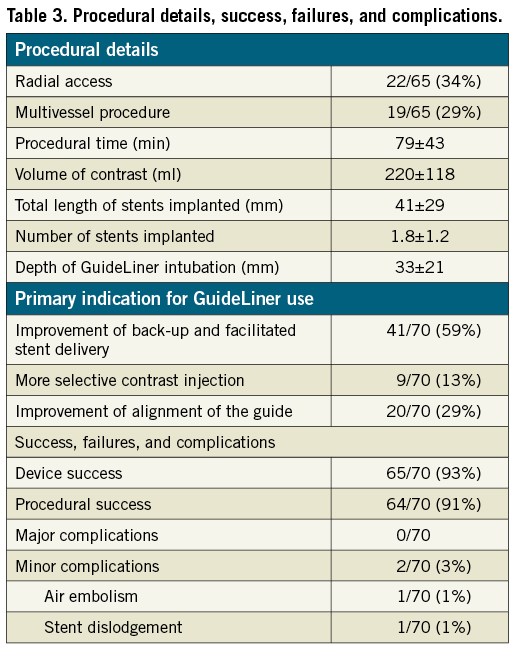
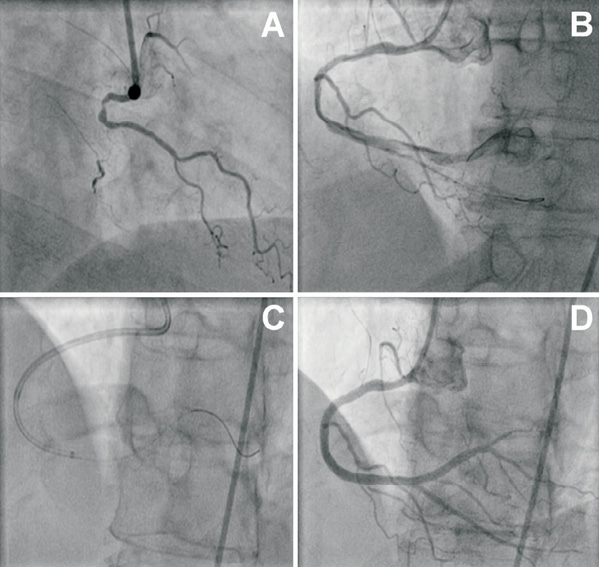
Figure 2. Angiography of a chronically occluded RCA in a 55-year-old female patient (A). Wire crossing was achieved using a pilot 50 wire. After subsequent passage and dilation with low profile balloons, the flow is partially restored and a long dissection can be noted that extends into the postero-lateral branch (B). Passage of a stent was unsuccessful due to marked resistance in the distal segment of the vessel. With the help of an anchoring balloon, the GuideLiner catheter was deeply intubated over the guidewire (C). Then, several drug-eluting stents were successfully delivered and postdilated, with a good final angiographic result (D).
A 6 Fr guide catheter was used in all subjects, while radial access was chosen in one third of cases. Multivessel procedures were performed in almost one third of the patients, and there were 17% of chronic total occlusions. Of all 126 stents implanted, 123 (98%) were third-generation drug-eluting stents (DES). In this registry, we noted a single stent that was damaged upon advancement across the metallic collar of the GL; damage to the (secondary) guidewire tip when passing the metallic collar of the GL occurred slightly more often (4/70; 6%).
DEVICE SUCCESS AND DEVICE FAILURE
The overall success rate of the GL was 93%. The average depth to which the GL was intubated in the proximal target vessels was 33±22 mm (range: 0 to 106 mm), however, these generally deep intubations did not cause any coronary dissections. The rate of procedural success of the transradial and transfemoral access routes was 95.5% and 88.4% (p=0.35), respectively, but the power of the study was insufficient to draw sound conclusions from this comparison. There were five device failures (5/70; 7%), which are illustrated in Figure 3.
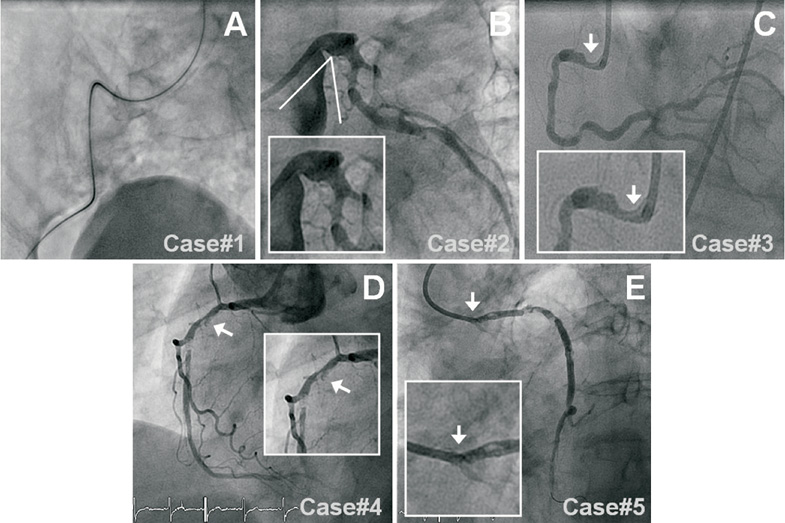
Figure 3. Angiographic overview of the device failures: Case #1) The first case was a 79-year-old male patient with an acute inferior MI. The target lesion was located in a diffusely diseased, heavily calcified RCA. The GL could not be advanced through the guide catheter because of severe iliac tortuosity (A), but procedural success was accomplished by use of a 3DRC guide catheter, two guidewires, and a distal anchoring balloon. Case #2) The second case was a long and calcified proximal LCX lesion, located behind a sharp angle between the LM and LCX that prevented GL intubation (B). Case #3) The third case was a 56-year-old subject who underwent an elective PCI of a diffusely diseased RCA. The GL catheter could not be intubated in the vessel due to a proximal lesion (C). The procedure was finished successfully with an AL1 guide. Case #4) In the fourth patient, the target lesion was a heavily calcified long mid RCA lesion (D). The proximal RCA segment was diffusely diseased, which prevented deep GL intubation (a depth of only 5 mm) and resulted in insufficient support; however, this problem was solved by rotablation of the ostium. Case #5) The fifth case was a vital 87-year-old female with stable angina due to a severely calcified proximal lesion in an 18-year-old saphenous vein graft. An AL2 guide catheter was positioned in the ostium and a flexible guidewire with hydrophilic coating was advanced across the lesion. Use of the GL was attempted to increase back-up support but the GL could not be advanced into the ostium (E), and the PCI procedure was terminated as a second guidewire could not pass the ostium either. We discussed the patient with our thoracic surgeons, who then performed an elective repeat bypass surgery with an uneventful clinical course.
COMPLICATIONS
We noted no major complications or coronary dissections. There were two minor complications, which are outlined below. In the first case, during PCI of a diffusely diseased RCA in a 53-year-old male, the GL was deeply advanced (61 mm intubation depth) to increase back-up support and to pass a balloon catheter across the heavily calcified distal RCA stenosis. During this manoeuvre, some air embolism was noted as a result of insufficient venting of the wedged GL, which caused a brief phase of stasis of coronary flow that was rapidly resolved. The second minor complication occurred during PCI of a long mid lesion in an RCA with “shepherd’s crook” anatomy. After predilatation and stenting of the mid RCA, an attempt to advance a second stent through the first one was made, which turned out to be extremely difficult. To increase support, the GL was advanced over both guidewires and the second stent balloon system (stent still undeployed), which led to dislodgement of the stent from the balloon. Eventually the dislodged stent was crushed behind a third stent and was postdilated with high balloon pressures, leading to a good final angiographic result with an uneventful clinical course until the eight-month follow-up.
Discussion
Good back-up of the guide catheter is crucial for both wiring and equipment delivery. The development of guide catheter extension systems has further expanded the therapeutic arsenal of the interventional cardiologist5-12. Intubation of the guide catheter extension system into the target vessel provides enhancement of equipment delivery in challenging coronary lesions, and facilitates engagement in case of difficult takeoff of the coronary ostium. Takahashi et al demonstrated that a guide catheter extension system provides a substantial improvement in back-up support5. The support was directly related to the depth of intubation. For example, insertion of a 5 Fr guide catheter 15 mm into a 6 Fr catheter doubled the back-up support. The guide catheter extension system may be used as a tool for deeper intubation of the guide, referred to as “rail-roading”, as was described in detail by Farooq et al18. Its use in graft interventions is well recognised as aiding graft cannulation and enhancing the stability of the guide in the graft ostium. Further back-up may be achieved by advancing the extension catheter, thereby allowing the guide to back out and down until it rests on the aortic valve or contralateral aortic wall (Swan-neck manoeuvre)18. And finally, guide catheter extension systems can be used as an aspiration device18.
The Twente GuideLiner registry reports on a consecutive series of GL applications in 65 patients, treating 70 target vessels with implantation of 126 stents (98% being third-generation DES). So far, this is the largest registry on the use of the GL in routine daily practice. Demographics and clinical characteristics of the study population are similar to previous all-comers stent studies and our general PCI population19-25. However, lesion characteristics differed a lot from the general patient population as the majority of target lesions were long and complex: all but two target lesions (97%) were classified as lesion type B2 or C with more than half of them being located distally, and the vast majority being at least moderately calcified.
During the first months, the GL was used as a bailout device in challenging cases, when the “old familiar tricks” (e.g., deep-seating manoeuvres or use of buddy wires) had failed. However, after becoming more familiar with the device, we switched to a more upfront use in difficult anatomical situations. In our present series, the main indication for GL use was to improve guide support to facilitate stent delivery (59%). An illustration is shown in Figure 2. However, in one third of the cases the GL was used to improve coaxial alignment of the guide catheter in anatomical situations with an abnormal takeoff of the target vessel (e.g., shepherd’s crook-shaped proximal RCA) or a vertical takeoff of either RCA or left main stem. In particular, a vertical offspring of the left main stem, as may be seen in young lean patients or patients with pulmonary emphysema, bears an increased risk of dissecting the left main stem with a guide catheter. Gentle intubation of the GL substantially facilitated the intervention in such patients (Figure 4). In a small number of patients, the GL was used to perform selective contrast injections for a better visualisation of the vessel of interest with smaller amounts of contrast; this indication for GL use may be considered in patients with large calibre vessels, such as a dominant left coronary artery, and an impaired renal function, or if an adequate visualisation cannot be achieved by other means26.
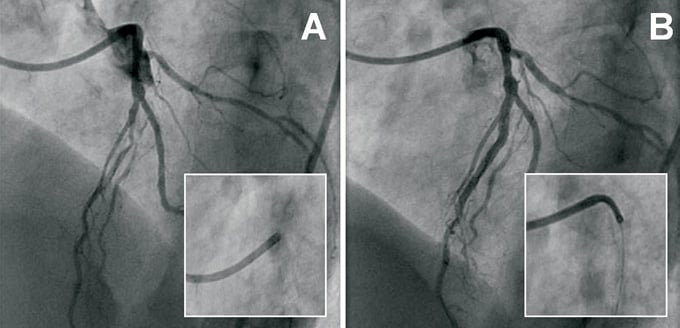
Figure 4. Angiographic overview of a subject with a vertical offspring of the left main (A and B). The GuideLiner catheter was used for coaxial alignment of the guiding catheter, providing gentle intubation in the LM and good support to treat the LAD lesion.
The GL may also be useful to facilitate demanding diagnostic coronary angiographies, which has not been described so far and was beyond the scope of our registry of GL use in PCI patients. Nevertheless, we would not like to withhold the information that our group also used the GL in several demanding cases of diagnostic angiographic visualisation of bypass grafts. Figure 5 shows an example of a gastroepiploic artery (GEA) graft, visualised both with and without use of a GL. It should be emphasised that in case of coronary angiography, the operator should refrain from the use of intracoronary wires and devices as much as possible. However, there are circumstances in which a graft cannot be properly visualised. Instead of accepting a poor visualisation, the use of a guide catheter extension system can be considered in order to achieve conclusive angiographic imaging. It should be used by an interventional cardiologist with great care, and maximum effort should be taken to ensure that such manoeuvres do not give rise to a coronary dissection.
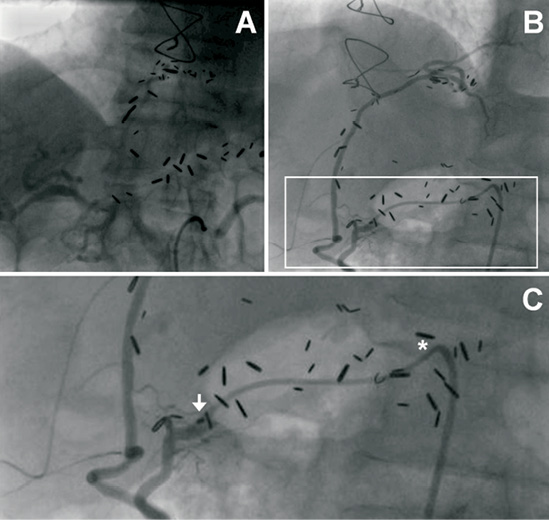
Figure 5. Visualisation of a gastroepiploic artery (GEA) graft in a 66-year-old male patient. Panel A shows vague images of the GEA graft, obtained during routine angiography two years earlier. Panel B illustrates the difference in image quality, obtained recently with the use of the GuideLiner (GL) catheter. The arrow in Panel C is pointed at the tip of the GL catheter.
SUCCESS RATE, SHORTCOMINGS, AND POTENTIAL PROCEDURAL RISK
The success rate of the GL was 93% in our study, which is in agreement with previously reported smaller case series10,15,17,18. Stent damage at the site of the metallic collar of the GL occurred in one out of 126 stents implanted, which was a drug-eluting stent with a nominal diameter of 3.5 mm. Others have reported a higher rate of stent damage (6%) due to the collar of the GL catheter10. Therefore, we discourage the use of stents with a nominal diameter of 4 mm or more through a “5-in-6” Fr GL catheter. Murphy et al recently reported an uncommon case of balloon damage at the site of the metallic collar16. In addition, secondary (buddy) guidewires can be damaged upon advancement when the GL is in place, as reported in our present study. The “5-in-6” Fr GL catheter permits the passage of virtually all regular balloon catheters, contemporary optical coherence tomography (OCT) catheters, and coronary stents up to a nominal diameter of 3.5 mm. However, it does not allow the use of larger devices such as thrombectomy catheters, some intravascular ultrasound (IVUS) probes, and simultaneous kissing balloon inflations.
Although the GL turned out to be generally beneficial with a relatively low rate of device failure, we identified some scenarios, in which the usefulness of the GL may be questionable. Firstly, a difficult access due to iliac tortuosity may impede the advancement of the GL through the mother guide, as was seen in one of our patients. Secondly, the proximal part of the target vessel should be suitable for intubation of the GL catheter; therefore, ostial/very proximal lesions or sharp angles of coronary arteries may lead to device failure, as was noted in the majority of our cases with device failure.
In general, use of the GL turned out to be safe. No major complications were noted, but there were two minor complications with favourable outcomes and an otherwise uneventful clinical course. There was one case of air embolism due to insufficient venting. In the second case, a stent was dislodged from the balloon by the tip of the GL when advancing the GL over a stent balloon system. Both complications could have been avoided, if more care had been taken and the instructions of the manufacturer had been followed. Luna et al15 reported a substantially higher number of cases with pressure dampening (57%) during engagement of the GL catheter; however, dissimilar to our study, they used a “6-in-7” Fr system in the majority of cases.
HOW TO USE THE GUIDELINER AND HOW TO AVOID COMPLICATIONS
Several considerations can be mentioned in order to choose or refrain from the use of a guide catheter extension. If more back-up of the guide catheter is required, the first step can be the use of buddy wires, extra stiff wires, or buddy balloons. However, if these measures fail, a GL catheter may be considered, which allows the mother guide and wires to be left in place. The operator should, however, be convinced that the proximal part of the target vessel is suitable for intubation. If the lesion extends to the proximal segment or if there is sharp angulation, the use of a guide catheter extension system is generally not recommended. Alternatively, the proximal segment may be stented first, followed by gentle intubation of the GL catheter and treatment of the distal segment (so-called proximal-to-distal stenting). However, care should be taken to avoid deformation or longitudinal compression of a proximally implanted stent27,28. If there is a problem with coaxial alignment of the available guide catheters, the operator should estimate the risk of performing the procedure with a suboptimal position of the tip of the guide (in case of a simple proximal lesion one may continue). However, if substantial back-up is required, it appears wise to use a guide catheter extension. This decreases the risk of guide-induced dissections and improves the back-up of the mother guide. If the patient has an impaired renal function and the operator expects to use large amounts of contrast (e.g., in a dominant left coronary artery system), a guide catheter extension system may be considered as a valuable first choice. And finally, if the operator intends to treat a bifurcation lesion, it should be realised that a “5-in-6” Fr system does not allow the simultaneous use of two balloons. Therefore, a choice should be made to use a larger guide catheter extension system (“6-in 7” Fr system or Proxis™ device), remove the guide catheter extension system before the kissing procedure, or refrain from its use and adhere to usual practice.
A WORD OF CAUTION
Intubation of the GL bears the risk of causing a dissection in a proximal coronary artery and should be performed carefully. If resistance is encountered when advancing the device, the GL can be retrieved into the mother guide and then re-advanced over a balloon catheter (to improve alignment) into the target vessel17. After advancing the GL into the vessel, the operator should check the coronary pressure waves and verify the presence of adequate, preserved antegrade coronary flow. Since use of the GL reduces the size of the working lumen, there is an increased risk of air embolism, which can be diminished by slow advancement and withdrawal of the equipment; time should then be taken to carefully vent the system. A limitation of the GL device is the metallic collar located at the entrance of the extension tube. In case of resistance while advancing the stent, the location of the stent in relation to the metallic collar of the GL should be checked and the stent should be inspected for damage. If the collar is located at a bend in the catheter, the GL should be retrieved gently into a straight section of the mother guide in order to allow more coaxial alignment of the collar17. The use of more than one guidewire in combination with a relatively large size of the stent delivery system may sometimes render stent passage through the collar of the GL difficult and occasionally impossible. Factors such as operator awareness, experience, number and type of guidewires, size of the stent, vascular anatomy, the shape of the guide catheter, and indication for GL use may have an effect on the incidence of this problem, which differs between case series17.
LIMITATIONS
The present registry of a consecutive series of PCI patients treated with the use of the “5-in-6” Fr GL provides some “real-life” insight into efficacy, limitations, and the potential risk of this device. Although our patient population is larger than that of all previously reported cases and patient series altogether10-18 the population is still relatively small. In addition, due to well-known limitations inherent to registries, this single centre registry cannot provide the scientific level of insight that might be obtained from a randomised study. During the course of this registry, use of highly deliverable third-generation DES in most patients was our standard of care29, which could have affected our results. We cannot exclude that in cases with upfront use of the GL, a standard guide catheter or other manoeuvres and tricks (e.g., deep intubations or buddy wires) could also have led to procedural success.
CONCLUSIONS
Use of the GuideLiner catheter resulted in an increased back-up support and guide catheter alignment for stent delivery in the presence of unfavourable tortuous coronary anatomies and in complex, heavily calcified, and often distally located lesions, which otherwise may have been considered unsuitable for PCI. The procedural success rate of the GL was high without major complications.
FUNDING
This investigator-initiated study was performed without specific funding. The research department received educational and/or research grants in the past and has participated in clinical studies funded by Abbott Vascular, Biosensors, Biotronik, Boston Scientific, Cordis, and Medtronic.
Conflict of interest statement
C. von Birgelen is a consultant to and has received lecture fees or travel expenses from Abbott, Medtronic, and Boston Scientific and has received a speaker’s honorarium from Merck Sharp & Dohme. All of the other authors have no conflict of interest to declare.

