Abstract
Aims: Challenging coronary anatomies including chronic total occlusions (CTO), extreme vessel tortuosity, diseased bypass grafts, and anomalous coronary arteries pose difficulties in coronary interventions. The GuideLiner is a monorail catheter originally developed to facilitate delivery of stents to target lesions in tortuous vessels. We conducted a study on the feasibility and safety of utilising this catheter in a wider array of complex coronary interventions.
Methods and results: Consecutive patients undergoing coronary or peripheral interventions where a GuideLiner was used were recruited into this study. Patient demographics, lesion and vessel characteristics, procedural details and outcomes were prospectively entered into our database and analysed. From September 2009 to October 2011, 54 consecutive patients underwent coronary intervention in our institution using a GuideLiner; 21 out of 54 coronary applications were motivated by the need to increase support to cross CTOs, predominantly of the RCA. Anomalous or angulated take-off of the treatment vessels (31%), previously deployed proximal stents (15%), heavy proximal calcification (9%) and tortuosity (7%) accounted for the remaining reasons. One patient had successful renal denervation with the aid of a GuideLiner catheter. Procedural success was 98% in our series with no device-related periprocedural complications such as ostial dissection or myocardial necrosis.
Conclusions: The use of a GuideLiner facilitates the approach to complex coronary interventions including chronic total occlusion and saphenous vein graft intervention by providing greater back-up support and easier engagement of coronary ostia.
Introduction
Lower profile balloons and improved stent deliverability have made PCI in the modern era easier as compared to 15-20 years ago. Still, when dealing with challenging coronary anatomies, extreme vessel tortuosity, chronic total occlusions, or calcification, several problems can arise: poor guiding catheter support, failure to cross with a wire or a balloon, and inability to deliver a stent to the target lesion remain common problems. Techniques to improve support can be divided into passive, such as the use of larger calibre guiding catheters or of catheters with shapes gaining support from the aortic sinuses or contralateral aortic wall, and active, including the use of buddy wires, super-stiff wires, proximal and distal anchoring balloons, and deep intubation of the guiding catheter1. The last technique is more commonly used with small 5 or 6 Fr guides and is prone to failure or vessel damage when used in vessels with angulated origins or with proximal disease2,3. The use of a smaller guiding catheter inside another (mother-and-child technique) led to the development of straight flexible and atraumatic catheters such as the Heartrail® II (Terumo Corp., Tokyo, Japan) and the GuideLiner® (Vascular Solutions, Minneapolis, MN, USA)4-8. The latter catheter has an easier delivery because, unlike the 120 cm long Heartrail II, it is compatible with normal length balloons and stents, does not require a second Tuohy-Borst adapter, and does not cause air embolism during insertion or withdrawal.
We describe our consecutive experience of using the GuideLiner catheter to facilitate coronary interventions, focusing on tips and tricks to prevent wire or stent damage during insertion into the proximal end of the GuideLiner and compatibility of the various sizes available with contemporary microcatheters, balloons and stents.
Methods
We prospectively analysed 55 consecutive cases performed in our institution between September 2009 and October 2011 in which the GuideLiner catheter was used during coronary or peripheral interventions. Patient history, indications for procedure, and angiograms were reviewed to determine the factors leading to the use of a GuideLiner. Indications for use were categorised into: i) anomalous or angulated take-off of native coronaries or vein grafts/mammary arteries, ii) proximal vessel tortuosity, iii) extreme lesion/vessel calcification, iv) previously deployed stent in proximal vessel, and v) chronic total occlusion. Target lesion procedural success was defined as successful wire crossing, balloon angioplasty and stent. The GuideLiner is currently available in two sizes: 5-in-6 with an internal diameter of 0.056” and 6-in-7 with an internal diameter of 0.062”. Both are 20 cm long thin-walled hollow tubes coated with silicone for lubricity and connected to a thin flexible steel shaft offering a total working length of 135 cm. The catheter is inserted into the guiding catheter along a normal 0.014” previously positioned coronary guidewire exiting after the first 20 cm as in other monorail catheters.
Statistics
Continuous variables are expressed as means and standard deviations while categorical variables are expressed as counts and percentages. All data were processed with the software Statistical Package for Social Sciences, version 17 (SPSS, Chicago, IL, USA).
Results
A total of 55 consecutive cases (54 coronary cases and one renal denervation) involving use of the GuideLiner were performed by two operators in our institution within the study period. Patient demographic data and indications for treatment are presented in Table 1. The majority (83%) of patients had previous coronary revascularisations including angioplasties, bypass grafting or both. Eighty-seven percent of the patients presented with stable effort angina. In this series, 98% of patients had complex type C lesions and the right coronary artery (RCA) was the most commonly intervened vessel. Procedural details are listed in Table 2. A femoral approach was employed in the majority of patients (39/55, 71%) in order to use 7 or 8 Fr guiding catheters to obtain passive support and to allow the simultaneous insertion of multiple balloons or microcatheters. The indications for employing the GuideLiner (Figure 1) included CTO interventions, accounting for 38%, while anomalous or angulated take-off of vessels (31%), a previously deployed stent in the proximal vessel (15%) (Figure 2), a heavily calcified proximal vessel (9%) and proximal vessel tortuosity (7%) (Figure 3) accounted for the remaining indications. If concomitant multiple indications were present, the key factor leading to the GuideLiner insertion was identified and listed as the primary indication. For instance, in a small proportion of CTO cases, the GuideLiner was only employed to deliver balloons or stents to target lesions across a tortuous or calcified proximal vessel or through previously deployed stents after successful crossing with the guidewire, and therefore CTO intervention per se was not taken as the main reason for utilising the GuideLiner in such cases. Extra-support coronary guidewires and/or buddy wire techniques were used in 89% of cases. Whenever feasible, delivery of a distal anchoring balloon, whether deflated or inflated, was always performed to facilitate intubation of the GuideLiner catheter. Among all 55 patients, procedural success was achieved in 98% of cases. The single case of failure was a CTO of the RCA where the coronary guidewire failed to pass through the occlusion from the antegrade route despite the use of various methods to increase support, including placement of a 6-in-7 GuideLiner in a 7 Fr guiding catheter. There were no immediate periprocedural complications caused by the GuideLiner insertion, such as proximal vessel dissection or malignant arrhythmias due to the flow obstruction, or periprocedural myocardial necrosis as evidenced by raised cardiac biomarkers.
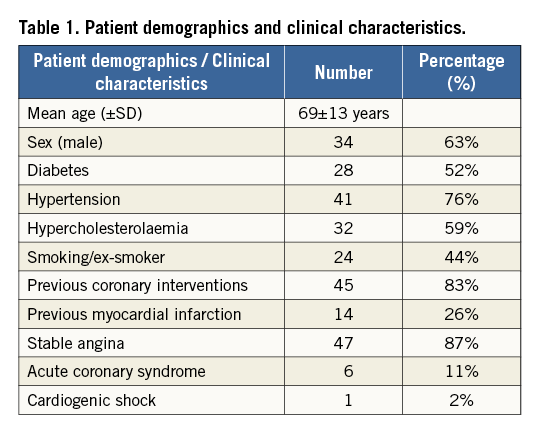
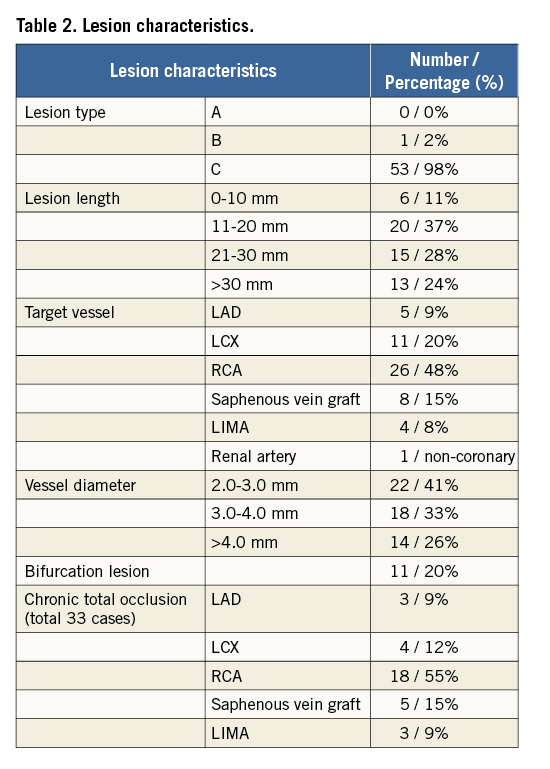
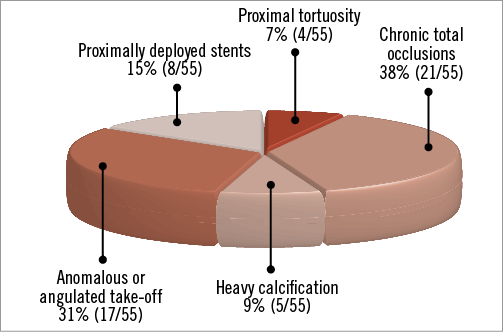
Figure 1. Main reasons for using GuideLiner.
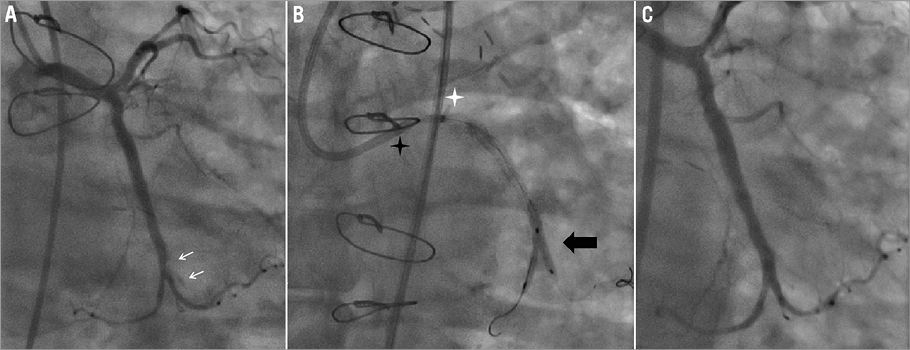
Figure 2. Stent delivery through proximally deployed stents & feasibility of kissing balloons. A 70-year-old man with previous bypass grafts and occluded native LCX presented with class II angina with thallium showing anterolateral ischaemia. Angiography showed occluded SVG-OM. PCI to LCX was performed with long stents but with distal edge dissection. A 6-in-7 GuideLiner assisted in delivering a stent tracking through the deployed stents in the proximal vessel and final kissing balloon was successfully carried out. A) Edge dissection at distal LCX (indicated by arrows). B) Kissing balloons (indicated by black star) delivered in a GuideLiner (tip indicated by white star) using a 7 Fr EBU guiding catheter (tip indicated by black arrow). C) Final angiographic result.
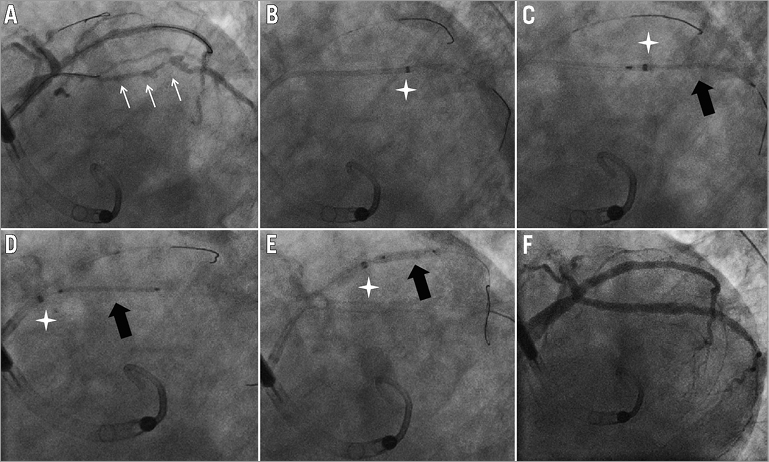
Figure 3. Stent delivery through tortuous and calcified vessels in a cardiogenic shock patient. A 90-year-old man with advanced COPD and chronic renal impairment presented with unstable angina. Echocardiography showed severe LV impairment with anterior wall akinesia. Angiography showed left main, intermediate branch, LCX and LAD disease. PCI was performed to the LCX, intermediate branch and left main coronary artery with haemodynamic support by Impella® (Abiomed Inc., Danvers, MA, USA). The GuideLiner was essential to facilitate delivery of thick high-pressure non-compliant balloons and stents in the extremely calcified LCX and intermediate branch and to achieve a good final angiographic result. A) Diffuse severe disease in LCX (indicated by arrows). B) Tip of GuideLiner at distal LCX (indicated by star). C) Stent delivered to distal LCX (indicated by black arrow). D) Stent delivered to proximal LCX (indicated by black arrow) with tip of GuideLiner withdrawn to LCX ostium (indicated by star). E) Stent delivered to intermediate branch. F) Final angiographic result.
The right coronary artery (RCA) was the artery which most commonly required the use of a GuideLiner, accounting for 48% of cases (Figure 4). The left circumflex artery (LCX) and saphenous vein grafts (SVG) were the second and third most commonly intervened upon arteries, accounting for 20% and 15% of cases, respectively. There were four cases (8%) of intervention to left internal mammary arteries supplying the left anterior descending artery (LIMA-LAD) and five cases (9%) of native LAD intervention. The only peripheral intervention was performed in a patient who underwent renal denervation for uncontrolled essential hypertension despite four antihypertensive medications. A 5-in-6 GuideLiner catheter was used in a short 50 cm long 6 Fr LIMA catheter to engage over a stiff wire into a downward-looking proximal left renal artery and to facilitate advancement of the Symplicity® catheter system (Medtronic Inc., Mountain View, CA, USA). In the majority of the CTO patients 7 or 8 Fr guide catheters were used, with a majority being Extra Back-Up shape for left coronary lesions and Judkins Right for right coronary lesions. Left 0.75, 1.0, 1.5 and 2.0 Amplatz guiding catheters were used for both right and left coronary lesions (Figure 5).
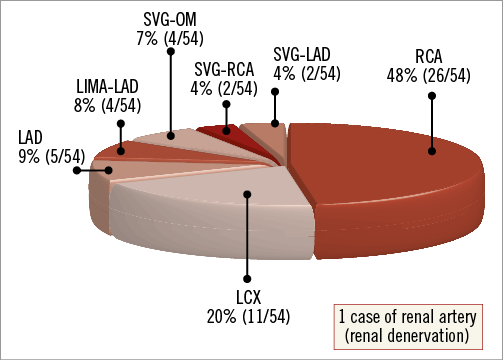
Figure 4. Target vessels including 54 coronary arteries and grafts and one renal artery.
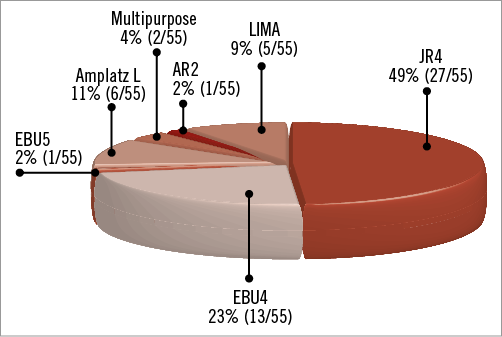
Figure 5. “Mother” guide catheters used in this series.
In view of the unavailability of the 7-in-8 GuideLiner catheter, only 5-in-6 and 6-in-7 systems were used in our series, with the latter accounting for 42% (23/55) of cases. There were 11 patients (20%) in our series who required intervention for bifurcation lesions, and kissing balloon inflation was feasible using the 6-in-7 GuideLiner catheter without undue difficulty in delivering the balloon catheters to the target lesion.
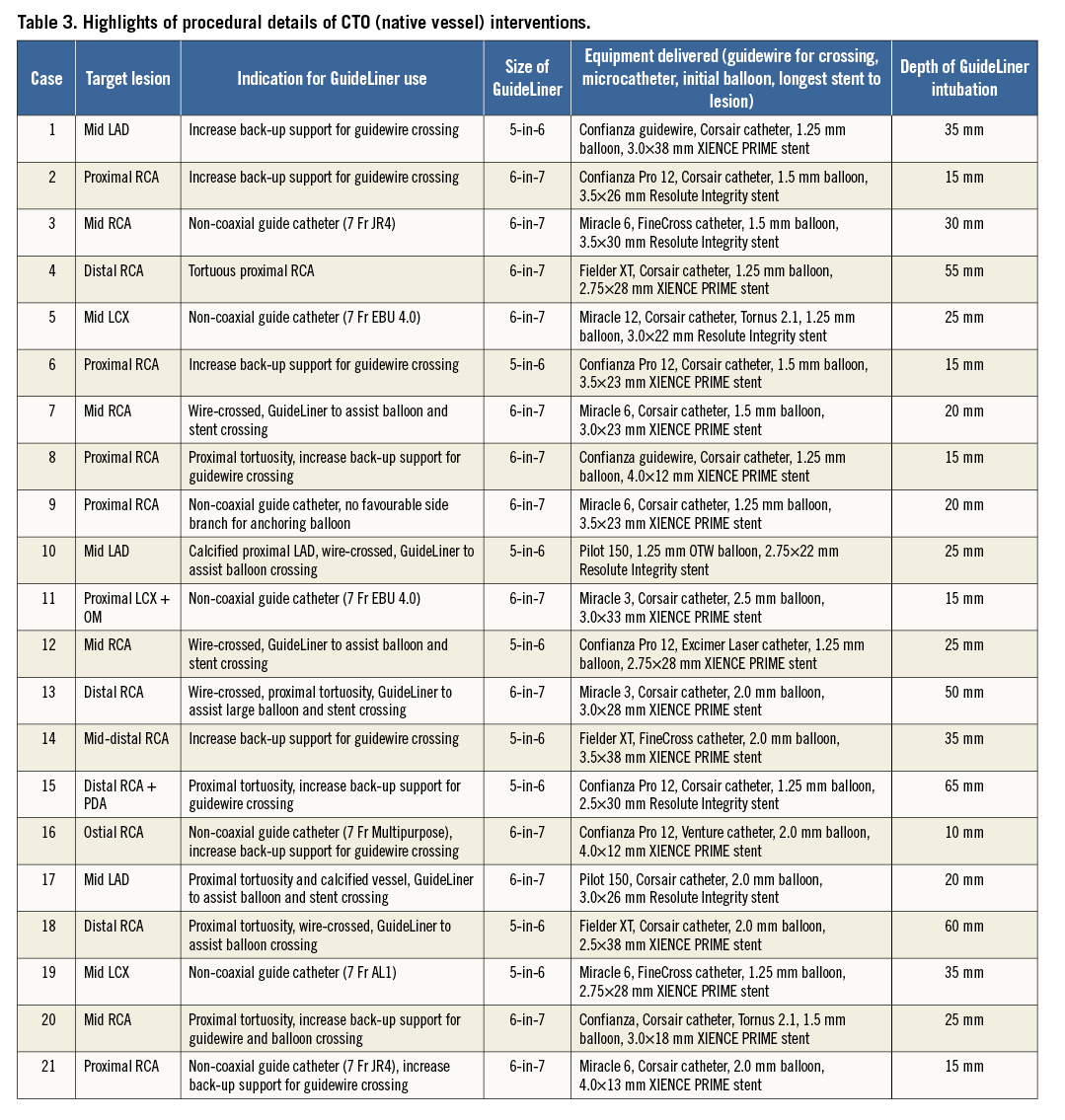
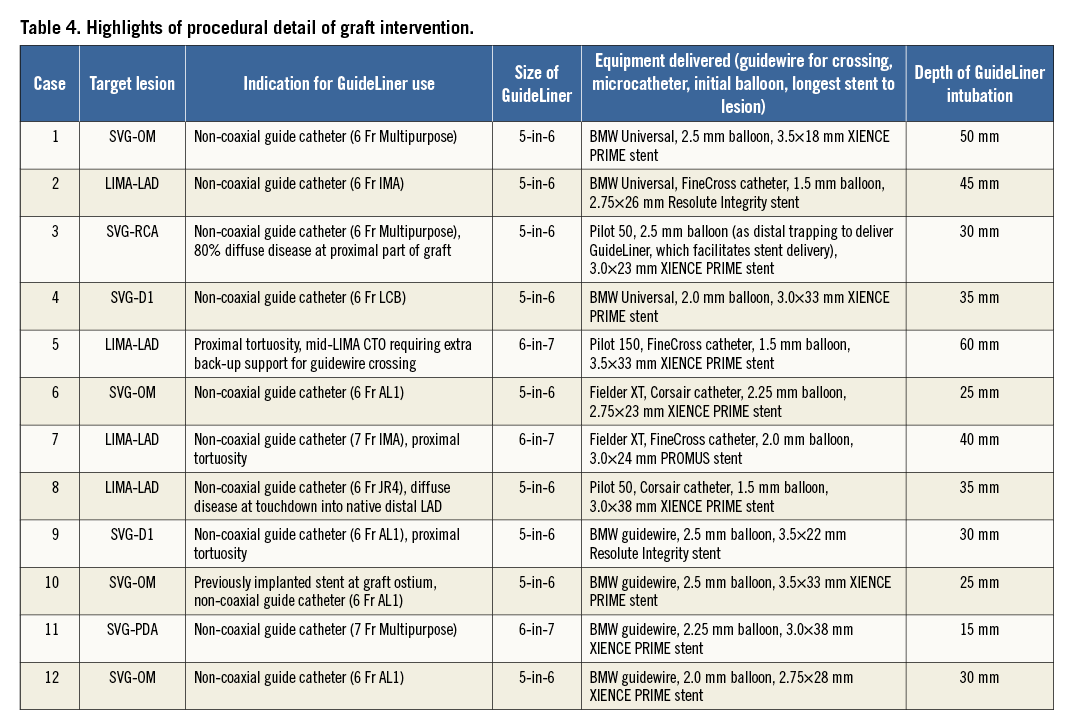
The native CTO and vein graft interventional procedural details in individual patients, including the size of GuideLiner and its depth of intubation, are listed in Table 3 and Table 4.
Discussion
USE OF GUIDELINER IN CTO INTERVENTION
CTO intervention remains one of the main challenges in percutaneous coronary intervention and one of the leading reasons for referral for coronary bypass surgery9,10. In patients where a retrograde attempt is impossible due to the absence of suitable collaterals from the contralateral circulation, an antegrade attempt to open the occlusion is the only feasible option. Both passive support by using a larger size guiding catheter such as 7 Fr or 8 Fr, and active support by using an anchoring balloon are the possible ways to increase the success in these CTO interventions1. However, as commonly encountered in RCA CTO, the absence of suitable side branches for anchoring balloons poses difficulties for active support, and in selected patients non-coaxial ostia preclude proper guiding catheter engagement. The use of a GuideLiner to achieve better support and deeper intubation of target vessels was demonstrated to be of great value in our series which had a large proportion of CTO interventions (Figure 6). In general, 6-in-7 and 7-in-8 GuideLiner catheters are preferable to enable the insertion of multiple intracoronary devices including the large Corsair® microcatheter (ASAHI Intecc, Aichi, Japan). It should be noted that the use of a GuideLiner is not limited to CTO intervention via the antegrade approach. When performing retrograde CTO intervention using the reverse CART technique11,12, the advancement of the GuideLiner from the antegrade guide catheter offers a visible and accessible target for the retrograde wire, shortening the distance between the site of re-entry of the retrograde guidewire and the antegrade guiding catheter.
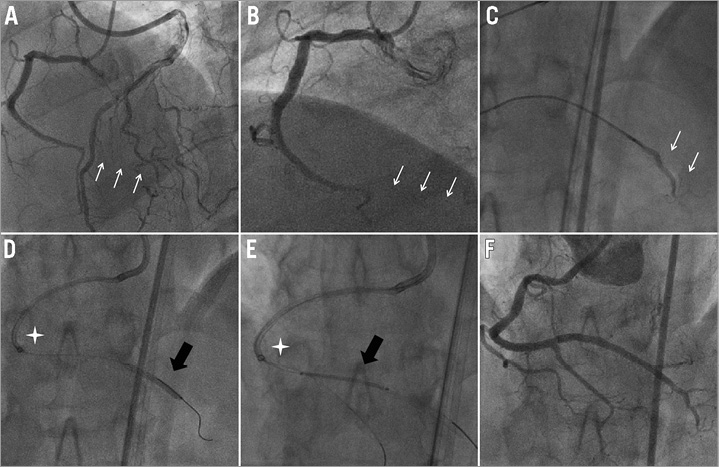
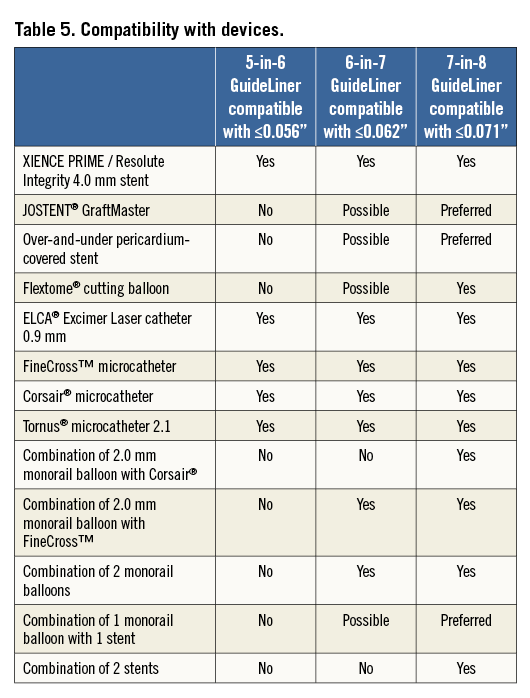
Figure 6. RCA chronic total occlusion. A 69-year-old man, with a symptomatic right coronary occlusion and two previous failed attempts. A Confianza Pro 12 guidewire (ASAHI Intecc) supported by a Corsair catheter and 6-in-7 GuideLiner in a 7 Fr JR4 guiding catheter was successfully advanced across the occlusion. A GuideLiner facilitated delivery of three stents on a Grand Slam (ASAHI Intecc) support wire. A) Distal RCA occlusion shown on bilateral injection. B) Distal RCA occlusion with proximal tortuosity. C) Selective injection with Corsair after guidewire crossed. D) GuideLiner (tip indicated by star) deep-seated with balloon inflated in the occlusion site. E) PDA wired to increase support and aid stent (indicated by black arrow) delivery. F) Final angiographic result.
USE OF GUIDELINER IN BYPASS GRAFT INTERVENTION
In our series, eight patients had saphenous vein graft lesions and five of these had chronic occlusion of the vein graft requiring intervention. The difficulty in these patients arises from the near impossibility of coaxially engaging the ostia of vein grafts which have a shallow take-off from the ascending aorta. Despite the use of multiple shapes of guides, adequate support for guidewire advancement and the passage of balloon catheters and stents could not be readily achieved. The use of the GuideLiner guide catheter extension consistently solved this problem (Figure 7). A recently published series by Fraser et al highlighted the feasibility of guide catheter extension for coronary bypass graft intervention via the transradial approach6. Similarly, for interventions to the LIMA, employing a JR4 or IMA guiding catheter occasionally fails to achieve enough support or deep intubation because of the subclavian tortuosity (Figure 8). The insertion of the flexible and atraumatic GuideLiner can offer an elegant solution, potentially also usable for selective angiography only.
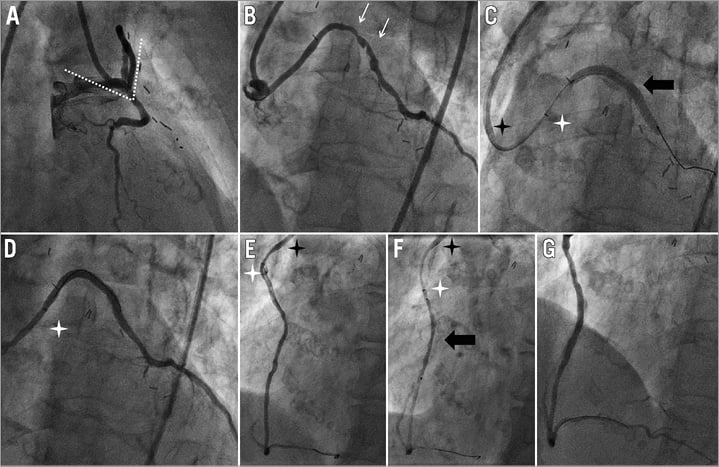
Figure 7. Saphenous vein intervention. An 80-year-old woman, with severe aortic stenosis and previous bypass grafts who underwent hybrid PCI prior to TAVI. Angiography showed non-coaxial engagement of JR4 guiding catheter to SVG-OM. A 6-in-7 GuideLiner catheter successfully engaged and intubated the vein graft to deliver the stent. During intervention to SVG-PDA, the same GuideLiner catheter in a 7 Fr Multipurpose guiding catheter engaged the vein graft and successfully delivered a 38 mm long drug-eluting stent. A) RAO view. Non-axial alignment of guiding catheter with the vein graft ostium (angle indicated by dotted line). B) LAO view. Degenerative vein graft lesions (indicated by arrows). C) LAO view. Stent (indicated by black arrow) delivered to the lesion, tip of GuideLiner indicated by white star while tip of JR4 guiding catheter indicated by black star. D) Final angiographic result on SVG-OM. E) Degenerative vein graft lesion at proximal SVG-PDA, tip of GuideLiner (indicated by white star) intubated into SVG ostium while tip of 7 Fr Multipurpose guiding catheter (indicated by black star) remained outside. F) Stent (indicated by black arrow) delivered to the lesion. G) Final angiographic result of SVG-PDA.
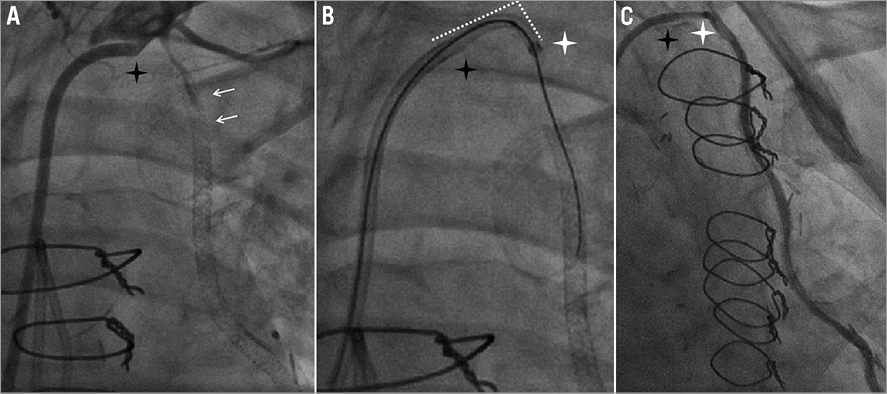
Figure 8. LIMA type IV in-stent restenosis intervention. A 56-year-old woman, with previous stenting to LIMA-LAD, presented with class III angina and anterior ischaemia on thallium. Angiogram showed occluded LIMA (type IV ISR). 7 Fr JR4 and IMA guiding catheters failed to engage the LIMA but, with the support of a 6-in-7 GuideLiner catheter, a variety of dedicated wires within a FineCross microcatheter and over-the-wire balloons were inserted to recanalise the occlusion. A) Tip of 7 Fr JR4 (tip indicated by black star) failed to engage the LIMA. B) Dotted line indicated the angle between the shaft of the guiding catheter and the tip of GuideLiner (indicated by white arrow). C) Final angiographic result.
BIFURCATION LESIONS
Interventions on bifurcation lesions requiring final kissing balloon inflation are feasible with the use of 6-in-7 (and, where necessary, 7-in-8) GuideLiner catheters. In our series, both provisional T-stenting and culotte stenting strategies were performed successfully13. If two coronary guidewires have been placed in the main vessel and side branch respectively, the GuideLiner has to be inserted over both coronary guidewires. Withdrawing the main vessel wire to engage the jailed side branch after main vessel stenting, then switching the jailed side branch guidewire into the main vessel is the recommended strategy. If a new guidewire has to be inserted and the GuideLiner is in situ already, meticulous attention has to be paid to ensure the guidewire passes through the lumen of the GuideLiner tubing rather than outside. In such a scenario, a Twin-Pass (Vascular Solutions) or a Crusade (Kaneka Medix Corp., Osaka, Japan) catheter, which feature two wire lumens and are inserted in a monorail fashion, can be advanced beyond the GuideLiner catheter to facilitate insertion of a second guidewire into the GuideLiner tubing.
GUIDELINER COMPATIBILITY MATRIX
In complex coronary interventions, particularly in CTO, larger lumen guiding catheters, usually 7 to 8 Fr, are used, not only to increase the passive support for lesion crossing and delivering balloons or stents, but to enable usage of a greater variety of dedicated devices to facilitate intervention. Dedicated devices such as the Corsair® microcatheter (ASAHI Intecc), FineCross™ microcatheter (Terumo) and Tornus® catheter (ASAHI Intecc) are commonly used to cross severe, occlusive or calcified lesions, or to facilitate exchange of guidewires. Alternatively, a 0.9 mm Excimer Laser catheter (Spectranetics, Colorado Springs, CO, USA) can be employed when the guidewire successfully passes the lesion but a balloon fails to follow14-16 (Figure 9). Compatibility of such devices with the GuideLiner catheter is of great importance as, on some occasions, two devices may be used simultaneously to facilitate complex coronary interventions. GuideLiner catheters are delivered through the normal coronary guiding catheters, resulting in an inner diameter that is approximately one Fr size smaller than the guiding catheter used. Being familiar with the size of the GuideLiner catheters and knowing their compatibility with different devices is important. For instance, a monorail balloon and a Corsair® catheter cannot be inserted together into a 6-in-7 GuideLiner catheter. This is particularly important when dealing with complex lesions or chronic total occlusions, as these microcatheters cannot be removed or exchanged by using the trapping balloon method when the GuideLiner catheter is in place. Currently, the largest 7-in-8 GuideLiner with an internal diameter of 0.071” is not yet commercially available but could be of great value, particularly in CTO interventions. For antegrade CTO approaches, a microcatheter, usually a Corsair® or occasionally a FineCross™, is used for wire exchange for re-shaping and wire escalation. When a wire successfully crosses the lesion with the microcatheter and must be exchanged for a monorail balloon, either the guidewire can be extended or the balloon trapping method can be used to remove the microcatheter, which is usually a Corsair® catheter. In such a scenario, only a 7-in-8 GuideLiner could accommodate a monorail balloon together with a Corsair® catheter. The use of newer devices, such as the Stingray balloon (Boston Scientific, Natick, MA, USA)17, for facilitating re-entry into the true lumen may also require the use of a 7-in-8 GuideLiner catheter. The compatibility of devices is illustrated in Table 5.
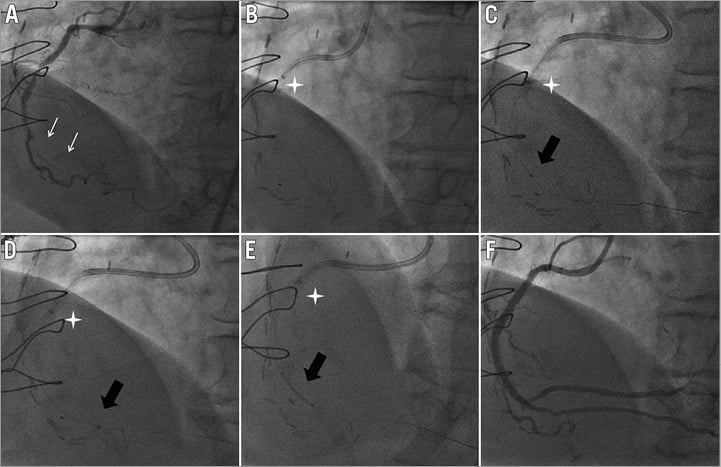
Figure 9. RCA chronic total occlusion. A 77-year-old woman, with severe peripheral vascular disease and previous bypass grafts (LIMA-LAD, SVG-OM and radial artery [RA]-RCA), presented with recurrence of angina CCS II. Angiography showed occluded RA-RCA with native RCA occluded from mid-distal segment. A Confianza Pro 12 successfully crossed the occlusion but even the smallest 0.85 mm NIC Nano balloon (SIS Medical AG, Winterthur, Switzerland) failed to cross. A 0.9 mm ELCA Excimer Laser catheter with the support of a 5-in-6 GuideLiner catheter in a 6 Fr JR4 guiding catheter was able to pass through the RCA occlusion. A) Mid-distal RCA occlusion (indicated by arrows) with retrograde filling from apical collaterals. B) GuideLiner (tip indicated by star) intubated to assist delivery of laser catheter. C) Laser catheter (indicated by black arrow) delivered to occlusion site. D) Laser catheter (indicated by black arrow) successfully crossed occlusion after laser energy delivered. E) Stent (indicated by black arrow) delivered to occlusion site. F) Final angiographic result.
TIPS AND TRICKS FOR SAFE AND EFFECTIVE USE OF THE GUIDELINER CATHETER
In situations such as non-coaxial alignment of the coronary ostium and extreme proximal vessel tortuosity (e.g., the “shepherd’s crook”), it can be difficult to deep-seat the GuideLiner over the intracoronary wire. A balloon inflated distally can be used to “attract” the GuideLiner and facilitate intubation of the coronary artery. Even in easier cases when the GuideLiner can be directly inserted, placing a balloon that can also be used for lesion predilatation (i.e., matching the diameter of the target artery or slightly undersized) prior to intubation with the GuideLiner is always recommended. Even when deflated, the balloon offers not only support but also a centring rail which reduces the chance of damaging the ostium and the proximal vessel during intubation with the GuideLiner. The following sequence is employed: first, insertion of the intracoronary guidewire, then the GuideLiner is passed up to the distal end of the guiding catheter, followed by a predilatation balloon, and the GuideLiner is then advanced into the vessel over the balloon.
However, advancement of coronary stents across the rapid exchange transition zone can occasionally be difficult because the leading edge of the stent can hit the metallic transition zone of the GuideLiner18. In our experience, this can be eased by positioning the transition zone of the GuideLiner in a straight part of the descending aorta rather than at the aortic arch, typically by gently withdrawing and rotating the GuideLiner, rather than forcing the stent in. Performing this manoeuvre under fluoroscopic vision is helpful and stents should be immediately withdrawn if there is any impression of longitudinal compression or strut distortion, a problem more commonly seen with some second-generation stents with super-thin struts19. Inserting a new guidewire can also be difficult, and we advise that all guidewires be positioned in advance and then the GuideLiner inserted over all of them. If this is not possible, rather than risking the frustrating experience of ruining multiple guidewires, a Twin-Pass (Vascular Solutions) or a Crusader (Kaneka Medix Corp.) catheter can offer an elegant solution. We have limited experience (two cases) of the second generation of the GuideLiner catheter (V2), in which the metal transition zone has been replaced by a lubricious polymer. Our impression was that this largely solved the above problem, but our suggested method could still be helpful if difficulties are encountered (Figure 10).
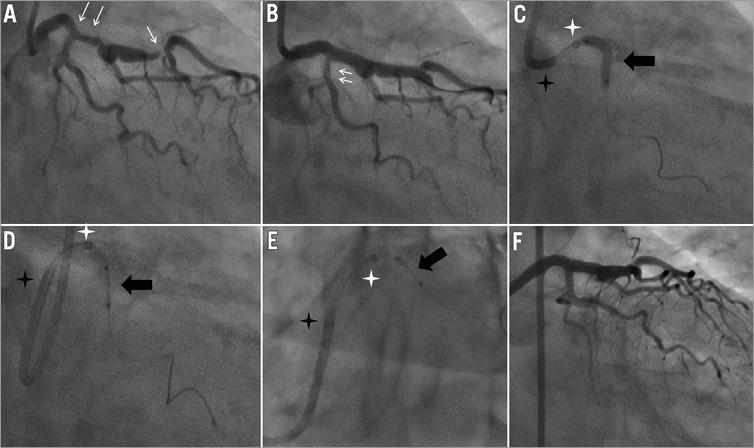
Figure 10. Initial experience with new generation of GuideLiner catheter (V2). An 83-year-old woman presented with class II stable angina with angiography showing distal LAD and diagonal bifurcation lesions and a lesion at the distal LM bifurcation extending into the LAD, followed by aneurysmal dilatation. The distal LAD bifurcation was treated and the LM was stented across into the LAD. Angiographic haziness was noted after the LCX ostium was re-crossed and dilated. An attempt to deliver a XIENCE PRIME™ 2.25×8 mm stent (Abbott Vascular, Santa Clara, CA, USA) failed but with the help of the new GuideLiner V2 catheter the stent was delivered without difficulty. A) Moderate lesion at the proximal LAD and critical lesion at the distal LAD (indicated by arrows). B) Haziness at the ostial/proximal LCX (indicated by arrows). C) Balloon delivered to the proximal LCX (indicated by black arrows) with the aid of a GuideLiner V2 (tip indicated by white star). D) RAO caudal view. Tip of 7 Fr EBU guiding catheter disengaged from LM ostium (indicated by black star) but the stent (indicated by black arrows) was delivered to the proximal LCX across LM-LAD stent strut. E) LAO caudal view. F) Final angiographic result.
Other potential uses of the GuideLiner have been reported previously20-22. Selective opacification of distal vessels in the presence of competitive flow, such as in graft cases, is feasible with the GuideLiner catheter. Contrast use could also potentially be minimised by selective injection, thus reducing the risk of contrast nephropathy in patients with renal impairment.
Conclusion
Analysis of this large series of patients demonstrated the safety and efficacy of utilising the GuideLiner monorail catheter to treat complex type C lesions successfully. In particular, non-coaxial ostial engagements, which are often encountered during saphenous vein graft interventions, and the need for extra back-up support, particularly important in the presence of tortuous and calcified proximal vessels or in selected cases of CTO interventions, can be largely solved by utilising a GuideLiner.
| Impact on daily practice CTOs, bifurcation lesions and graft interventions remain the most challenging subsets of coronary intervention. The use of GuideLiner to provide additional passive support despite a strong back-up guide is advisable when dealing with such complex cases. It can also be helpful in some situations during transradial PCI. Attention should be paid to the compatibility matrix and avoidance of air embolism when using this device. |
Conflict of interest statement
The authors have no conflicts of interest to declare.