The combination of calcification and tortuosity remains a significant challenge to the interventional cardiologist due to poor lesion compliance and difficulties with stent delivery. Improvements in stent design have been matched by increasing case complexity such that failure to deliver a stent remains one of the commonest causes of procedural failure. Techniques to aid stent delivery include vessel straightening using buddy wires and support wires, vessel preparation using rotational atherectomy and high pressure dilatation, and methods to increase backup support such as deep intubation, anchor balloon techniques and the use of guide catheter extensions (GC extensions). GC extensions include over-the-wire devices such as the 5 Fr-in-6 Fr Heartrail II and 4 Fr-in-6 Fr Kiwami catheters (Terumo, Tokyo, Japan) and the rapid exchange GuideLiner catheter (Vascular Solutions, Maple Grove, MN, USA). Kiwami is not available in Europe.
In this issue of EuroIntervention, Frits de Man et al report the largest cohort to date of patients undergoing PCI with the aid of the 6 Fr compatible GuideLiner catheter (5 Fr-in-6 Fr system)1. The cases are performed by experienced operators from a single centre and indications include backup support and stent delivery (41 cases), improvement in catheter alignment (20 cases) and selective contrast injection (20 cases). Of five device failures, all involved failure to deeply intubate the device, either due to proximal vessel disease (four cases) or iliac tortuosity. There were no major device related complications and specifically no cases of vessel dissection or embolisation despite intubation depth of up to 10.6 cm (mean 3.3 cm). These findings are in keeping with reported series using GC extensions in which stent delivery is the commonest indication, device related complications are rare and procedural success exceeds 90%, with failures largely due to the inability to deeply intubate2-6.
Whilst significantly adding to the reported experience with this device, details of the mechanism by which stent delivery is achieved are limited.
Backup support can be defined as the resistive force of a guide catheter within the aortic root against which stents are advanced into the coronary artery. This force is greatly increased as intubation depth is increased. However, backup support per se is only one of several mechanisms by which stent delivery may be achieved using a GC extension. Importantly, a GC extension may itself be advanced across points of resistance or tortuosity in the proximal vessel allowing delivery of a stent within the catheter directly to the mid or even distal vessel with little or no resistance (Figure 1)2-5. Distal delivery of a GC extension across segments that a stent will not cross is possible due to the greater flexibility of these catheters than a stent, their smooth coating and techniques such as advancement using an anchor balloon, advancement over a deflating balloon, use of the low profile 4 Fr-in-6 Fr Kiwami catheter, and facilitated proximal to distal stenting3-6. The anchor technique typically involves advancement of the extension over a balloon catheter inflated in the distal target lesion. The inflated balloon catheter increases support by locking the mother guide in place during GC advancement. To aid GC extension delivery, traction on the balloon catheter helps to pull the extension away from the outer curve of the vessel and into the central lumen (Figure 2). The technique of advancement over a deflating balloon is a different technique that allows an extension to be advanced through a balloon expandable stenotic lesion7. In this technique the stenosis is dilated with a balloon larger than the diameter of the GC extension. As the balloon is deflated the GC extension is advanced over the deflating balloon before the lesion recoils.
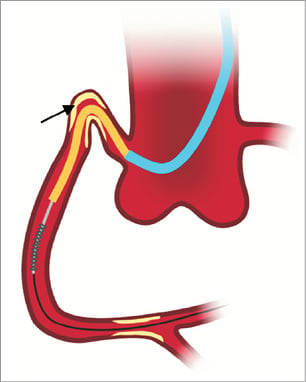
Figure 1. The guide catheter extension (GC extension, yellow) extends beyond the tip of the guiding catheter (blue) and is used to deeply intubate vessels. In addition to improving back-up support, a GC extension may itself cross points of proximal obstruction (arrow), allowing direct delivery of a stent to the mid or distal vessel.
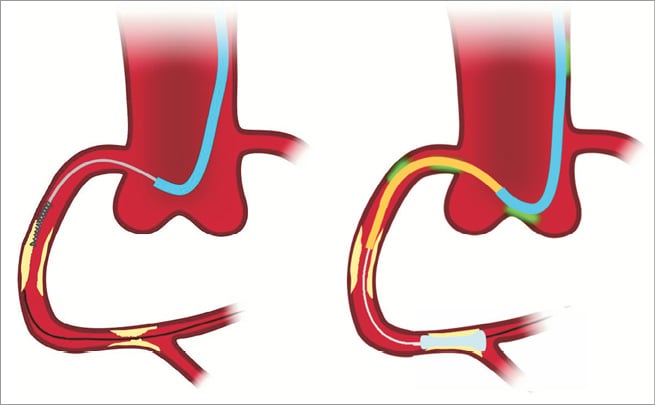
Figure 2. A stent may fail to pass disease on the outer curve of a vessel. A GC extension may be advanced through this segment by inflating a distal anchor balloon in the target lesion, pushing on the GC extension whilst exerting gentle traction on the balloon catheter. Traction pulls the balloon shaft off the outer curve, directing the GC extension through the central lumen.
Initial failure to deeply engage the GC extension due to obstructive proximal disease may also be overcome using these techniques. Facilitated proximal to distal stenting is especially useful in this setting4,5. This involves stenting of the proximal disease, followed by careful intubation of the stent with the GC extension (Figure 3). Once the extension has entered the stent it may be further advanced using the anchor and/or balloon deflation techniques. In this way proximal obstruction may be overcome and, with the resultant deep intubation improving backup support and coaxiality, more distal stent delivery may be achieved. In this way, in the most complex lesions, progressive stenting from a proximal to distal direction may, in fact, be the optimal method. Adequate vessel wall apposition of the proximal stents and coaxial intubation of the stent inlet are essential in this technique to avoid stent trauma (longitudinal stent deformation) associated with intubation of a deployed stent8.
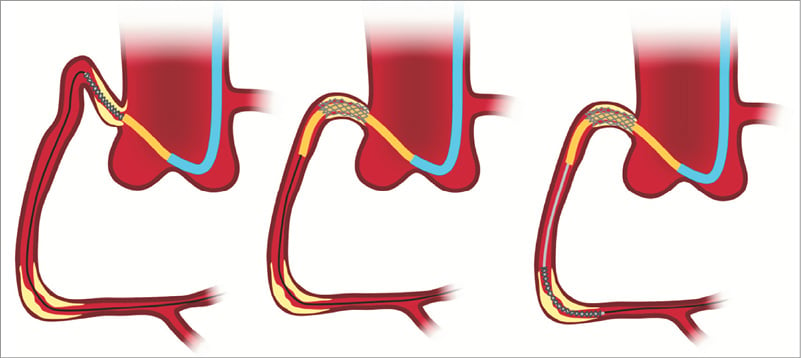
Figure 3. Severe proximal disease may prevent GC extension intubation. Facilitated proximal to distal stenting involves stent deployment in the proximal disease, followed by advancement of the GC extension through the deployed stent. The proximal obstruction is thereby crossed allowing stent delivery to a distal target lesion.
In addition to stent delivery, Frits de Man et al include “coaxial alignment of the guiding catheter” as a common indication1. This refers to the ability of a guide catheter extension to change the shape of a guide catheter by protruding from the tip to create a more optimal shape for coaxial engagement. Shepherds crook RCA and superior take-off LCA are cited as examples. The combination of a JR4 resting on the aortic valve with an extension, extending into a Shepherds crook RCA is a good example in which support from the aortic valve cusps below the RCA is achieved in a similar way to using an Amplatz left catheter. In contrast to the stiffer Amplatz catheter that is difficult to coaxially align in this setting (and so associated with a significant risk of vessel dissection), the flexible tip of the extension aligns itself to the proximal RCA and so is much safer. Similar techniques are useful to intubate grafts, the most marked example being the “Swan-neck” technique where the mother guide rests on the aortic valve and the extension reaches up several centimetres to the vein graft ostium5.
Frits de Man et al also describe GC extension use for selective contrast injection achieved by deep intubation1. As contrast is delivered directly to the target lesion, the volume required is greatly reduced and opacification improved. This may be especially useful in the setting of renal failure and opacification of vessels with dual native and graft supply8,9. GC extension use for diagnostic angiography is also described. However, it should be noted that this can only be achieved when using guide catheters as the devices are not compatible with the smaller lumens of 5 Fr or 6 Fr diagnostic catheters.
Despite very deep intubation, and seemingly aggressive intubation techniques, complications associated with GC extension use are rare and, specifically, no cases of vessel dissection, perforation or distal embolisation have been reported in more than 200 published cases1-6. This is largely due to the soft atraumatic tip, as well as the flexible shaft allowing coaxial alignment with the vessel. As described by Frits de Man et al, because contrast is injected directly to the tip of the extension catheter, it is essential that an adequate pressure waveform is present and forceful injection is avoided1. Stent dislodgement when an undeployed stent is withdrawn back into a GC extension, and stent disruption entering the collar of a GuideLiner, are also described in this and previous series1,4-6. These complications may be minimised by ensuring coaxial alignment with the GC extension tip and the GuideLiner collar respectively.
The GC extensions available are all used in similar ways5. Whilst the 4 Fr-in-6 Fr Kiwami catheter is the most deliverable, it has the smallest lumen (0.050 inches) and has the highest risk of air embolism6. Whilst stent catch at the collar is a limitation of the GuideLiner catheter, it is easier to use due to its rapid exchange construction that does not require removal of the Y connector. Advantages of this system also include better control of the “mother” guide catheter, reduced risk of air embolism, and larger sizes for 7 Fr and 8 Fr guides4.
So, where are GC extensions taking us?
Are they simply a tool to deliver stents when conventional methods fail, or do they significantly extend the complexity of disease that can be safely treated?
Certainly, to be used to their full potential, a range of advanced techniques can be employed, and to avoid the few associated complications there is a learning curve. The answer to this will be an individual one. For the authors of this editorial, GC extensions have almost eliminated the problem of not being able to deliver a stent, and are increasingly being used upfront when difficulties are anticipated. This has led to highly complex disease being treated more quickly and more safely than before, thereby significantly extending the types of cases that can be confidently attempted.
Conflict of interest statement
Dr Douglas Fraser has consulted for Vascular Solutions and Terumo; Dr Mamas A. Mamas has consulted for Vascular Solutions.

