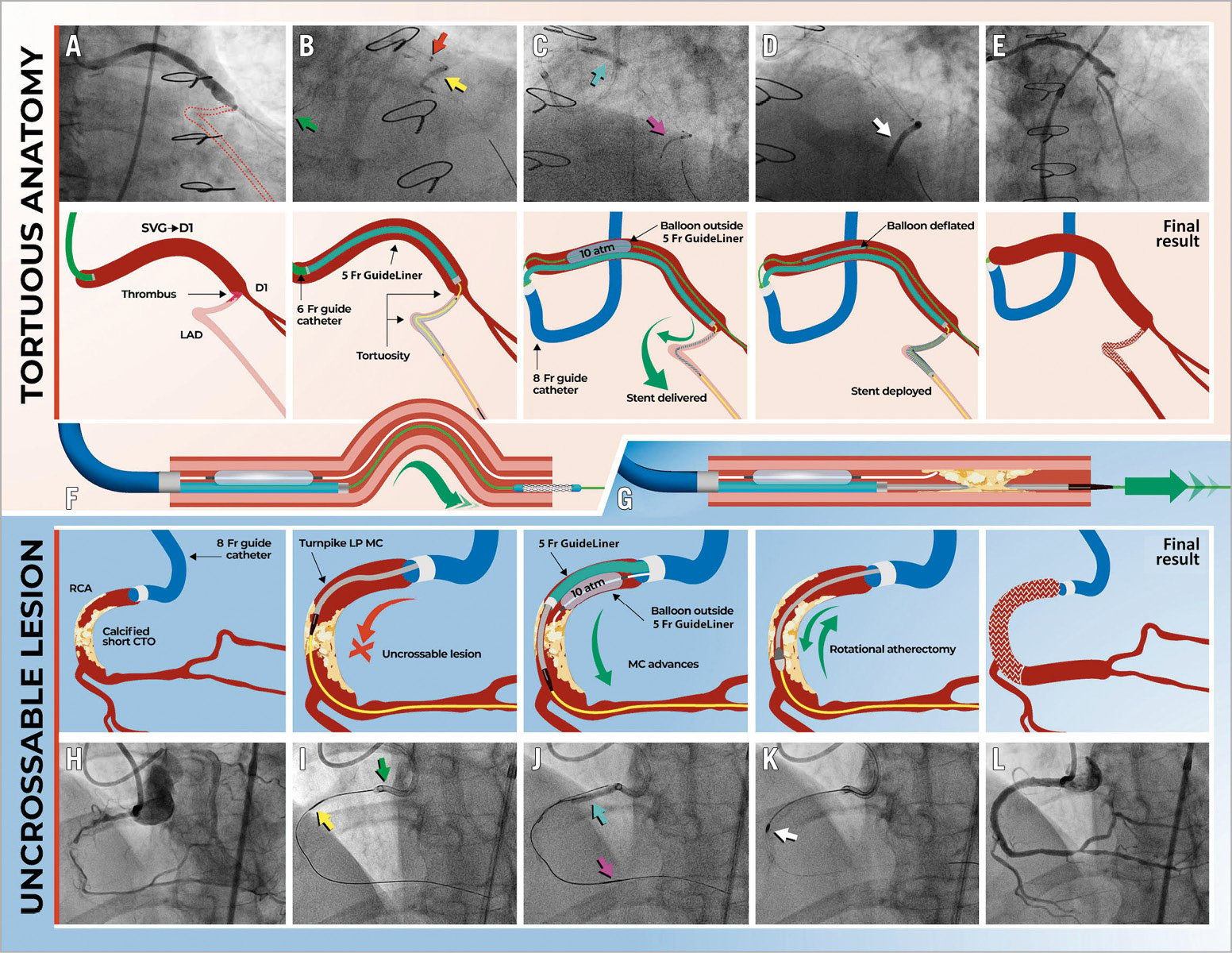
Figure 1. Tunnel in landslide technique (TILT). Case 1 (top panels). A) Thrombotic occlusion of D1 (grafted by an SVG), with no retrograde flow into the LAD (broken lines). B) A balloon (yellow arrow) is delivered through a guide catheter extension (GuideLiner, red arrow), but the 6 Fr guide catheter (green arrow) fails to provide enough support for stent delivery. C) The guide is exchanged for an 8 Fr AL1, the lesion is rewired with two workhorse wires, and a 5 Fr GuideLiner is advanced into D1 to deliver the stent (pink arrow), which is facilitated by pinning of the guide extension by a 3.5 mm balloon (cyan arrow), advanced over the second guidewire and inflated between the GuideLiner and the graft wall. D) Stent delivery and implantation are successful (white arrow). E) Final result. F) Use of TILT in tortuous anatomies. Case 2 (bottom panels). G) Use of TILT for uncrossable lesions. H) Short mid-RCA CTO. I) After antegrade crossing, the microcatheter (yellow arrow) cannot cross the occlusion and the 8 Fr AL1 guide disengages (green arrow). J) A 5 Fr GuideLiner is advanced to the proximal cap and pinned in place by a 3.0 mm balloon (cyan arrow), advanced over a workhorse guidewire and inflated between the GuideLiner and the vessel wall. This provides sufficient support to advance the microcatheter across the lesion to the distal vessel (pink arrow). K) Rotational atherectomy (white arrow) is performed. L) Final result, after implantation of two stents.
An 88-year-old woman presented with acute myocardial infarction. Angiography showed atretic left internal mammary artery to left anterior descending (LAD) graft, patent saphenous vein graft (SVG) to first diagonal (D1), and SVG-to-obtuse-marginal, and faint retrograde LAD filling from D1. Thrombosis of D1 impairing flow to the LAD was considered the culprit (Figure 1A, Moving image 1). The LAD was wired and ballooned from the SVG-D1 (Figure 1B). However, stent delivery was unsuccessful due to tortuosity (Moving image 2). Therefore, we upgraded to an 8 Fr AL1 guide and two workhorse guidewires were advanced distal to the lesion. A 5 Fr guide catheter extension (GCE) (GuideLiner®; Teleflex Inc., Wayne, PA, USA) was advanced into D1 over one of the two guidewires. A 3.5×20 mm balloon was delivered over the other guidewire and inflated between the SVG wall and the GCE, pinning it in place (Figure 1C). This provided enough support to deliver a stent to the LAD/D1 bifurcation (Figure 1D, Moving image 3), with a good final result (Figure 1E, Moving image 4). Figure 1F summarises the use of the technique for equipment delivery in tortuous anatomies, and Figure 1G highlights its role in calcified/uncrossable lesions.
A 74-year-old man was referred for PCI of a mid-right coronary artery (RCA) chronic total occlusion (CTO) (Figure 1H, Moving image 5). The CTO was crossed antegradely. However, the microcatheter could not traverse the CTO, despite the support provided by an 8 Fr AL1 guide (Figure 1I). A workhorse guidewire was advanced proximal to the CTO. A 5 Fr GuideLiner was advanced into the RCA onto the wire that crossed the CTO. A 3.0×20 mm balloon was advanced onto the other wire and inflated between the GuideLiner and the vessel wall. This provided enough support to advance the microcatheter across the CTO (Figure 1J, Moving image 6). Rotational atherectomy was performed (Figure 1K), followed by implantation of two stents, with an excellent result (Figure 1L, Moving image 7).
The impossibility of delivering interventional gear is a frequent reason for procedural failure, which can be mitigated by GCEs by increasing catheter support1. However, occasionally, this might not suffice. Here we describe the “tunnel in landslide technique” (TILT) which facilitates equipment delivery through a GCE (the tunnel), which is pinned in place by inflating a balloon between the GCE and vessel wall (the landslide). TILT requires an 8 Fr guide (I.D. ~0.090”), a 5 Fr GuideLiner (O.D. 0.053”), a 2.5-3.5 mm semi-compliant balloon (O.D. ~0.035”), and a workhorse guidewire. This (second) guidewire is advanced parallel to the (first) guidewire that crossed the lesion. The GuideLiner is then advanced onto the first guidewire. The balloon is delivered onto the second guidewire (proximal to the lesion) and inflated between the GuideLiner and the vessel wall, to trap the former against the latter. The interventional gear is then delivered through the anchored GuideLiner. At variance with alternative approaches1, TILT can be performed via a single guide. Contrary to common belief, balloon inflation does not compress the GuideLiner lumen, as its coil design provides sufficient radial strength to withstand external compression by the balloon. Although to we did not observe any complications, we would discourage TILT utilisation in the setting of significant untreated proximal lesions, as this could create ischaemia or dissection at that level, or in anatomically high-risk settings (e.g., anchoring the GuideLiner in the left main). We hope that TILT will represent an additional solution in the interventionalist’s toolbox.
Conflict of interest statement
R. Santiago has received speaker/proctoring honoraria from Boston Scientific, Abbott Vascular, and Teleflex. V. Del Río has received speaker honoraria from AstraZeneca, Zoll, Philips and Janssen. L. Azzalini has received honoraria from Teleflex, Abiomed, Asahi Intecc, Abbott Vascular, Philips, and Cardiovascular Systems, Inc. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 2. Case 1. Stent delivery is attempted, to no avail. The operator attempts to deliver a GuideLiner with the distal anchor technique, but this is unsuccessful, and wire position is lost.
Moving image 3. Case 1. TILT is successfully performed to deliver a stent through the tortuous anatomy.
Moving image 4. Case 1. Final result.
Moving image 5. Case 2. Mid RCA CTO.
Moving image 6. Case 2. TILT is successfully performed to advance the microcatheter to the distal vessel through this uncrossable lesion.
Moving image 7. Case 2. Final result.
Moving image 1. Case 1. Thrombosis of D1 impairing flow to the LAD.