Abstract
Aims: A novel “locking” microcatheter has been developed to address residual failure modes in chronic total occlusion (CTO) percutaneous coronary intervention (PCI). The aim of this study was to report the first clinical experience of this device.
Methods and results: The microcatheter was assessed prospectively in 92 unselected CTO cases across six European sites. Overall technical success was 85.9% (79/92) and 97.5% for patients with a J-CTO score of <3 (39/40). Within-CTO tortuosity was the only lesion characteristic to predict reduced technical success (OR 0.10 [0.01-0.97], p=0.047). Calcification (OR 0.45 [0.04-5.31], p=0.53), lesion length >20 mm (OR 0.58 [0.05-6.81], p=0.66) and a blunt proximal cap (OR 0.47 [0.08-2.90], p=0.42) were not associated with technical failure in this case series. Locking facilitated guidewire crossing (after initial failure) of the proximal cap in 23 cases, distal cap in 11 cases and CTO body in 10 cases, and delivery of the microcatheter through to the distal vessel in 22 cases. The overall procedural complication rate was 1.1% (1/92) with no major events.
Conclusions: Guidewire locking with this novel microcatheter assists penetration and crossing of fibrocalcific anatomy with a high degree of safety. Using this device in CTO PCI may lead to improved primary wiring and overall procedural success rates.
Abbreviations
CABG: coronary artery bypass grafting
CTO: chronic total occlusion
ECG: electrocardiogram
J-CTO score: Japanese Chronic Total Occlusion score
PCI: percutaneous coronary intervention
TIMI: Thrombolysis In Myocardial Infarction
Introduction
Chronic total occlusion (CTO) revascularisation by percutaneous coronary intervention (PCI) relieves symptoms and may be prognostically beneficial in appropriately selected individuals1-5. Advances in equipment and techniques refined within the hybrid algorithm have markedly improved success in recent years6. However, despite considerable progress, procedural difficulties persist, and the success rate of CTO PCI remains less favourable than non-CTO PCI7-10.
Common residual failure modes include an inability to cross the occlusion with a guidewire or to deliver equipment through the CTO after the guidewire has passed11,12. To address these and other persisting technical difficulties, a novel microcatheter with a unique guidewire locking mechanism has been developed. The aim of this study was to describe the first clinical experience of this new device in an unselected CTO PCI population.
Methods
STUDY DESIGN
The NHancer™ microcatheter (Interventional Medical Device Solutions [IMDS], Roden, The Netherlands) was assessed prospectively across six European sites (Royal Infirmary of Edinburgh, Edinburgh, Scotland, UK; Belfast City Hospital, Belfast, Northern Ireland, UK; Ziekenhuis Oost-Limburg, Genk, Belgium; Augusta Krankenhaus, Duesseldorf, Germany; Aarhus University Hospital, Skejby, Denmark; and HELIOS Klinikum Krefeld, Krefeld, Germany). A total of 92 unselected cases were enrolled between July and November 2014. Inclusion criteria were elective patients with a CTO and clinical indication for revascularisation. There were no exclusion criteria. The NHancer microcatheter was the initial and primary microcatheter used in every procedure; otherwise, the approach to each case was at the discretion of the operator. Written, informed consent for the study was obtained from all patients. Research was conducted in accordance with the Declaration of Helsinki.
MATERIALS
The NHancer is an over-the-wire microcatheter available in two working lengths: 140 cm and, designed for retrograde PCI, 155 cm. A hydrophilic polymer coating (distal 25 cm or 60 cm) provides enhanced lubricity. To increase visibility and improve crossing, the atraumatic tip is radiopaque and tapers over 10 mm. The NHancer has the lowest crossing profile of current, commercially available microcatheters with a leading edge outer diameter of 0.42 mm (1.3 Fr) and maximum shaft outer diameter of 0.75 mm (2.3 Fr). The minimum internal diameter is 0.40 mm (0.015”) and is lined for reduced resistance.
A uniquely designed torquer on a compressible shaft allows any commercial 0.014” guidewire and the microcatheter to be transiently locked in combination. Locking improves efficiency of force transmission and allows dynamic alterations in guidewire characteristics when required. By locking close to the guidewire tip (within 2-4 mm of the microcatheter leading edge), wire penetration can be markedly increased in a controlled manner. This may improve the ability of the guidewire, acting in combination with the NHancer, to overcome fibrocalcific resistance. Alternatively, locking further from the guidewire tip (10-20 mm) will primarily enhance wire torque and steering characteristics to facilitate navigation of tortuous or complex anatomy. A structural illustration of the device is shown in Figure 1.
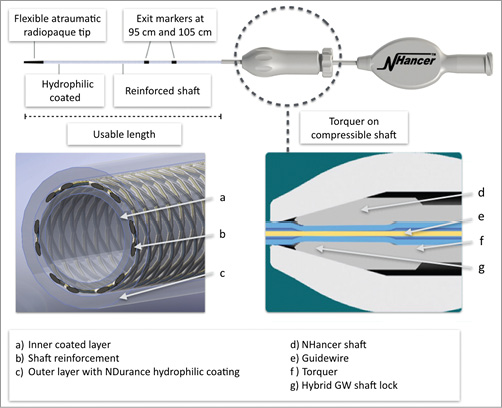
Figure 1. Structural illustration of the NHancer microcatheter.
STUDY ENDPOINTS
In CTO PCI, several different guidewires and/or support devices are often required (within each case) to achieve success. As overcoming each procedural step is as important as the next, reporting the impact of new equipment with reference to distal lumen access or technical success alone can be misleading. To better understand and describe the potential of the NHancer, we defined three major steps towards successful CTO revascularisation based on common key technical landmarks: guidewire crossing of either CTO cap (proximal or distal), guidewire crossing of the CTO body, and microcatheter (or equivalent) crossing of the CTO.
The NHancer was therefore assessed with reference to overall technical success, total number of strategies and microcatheters required per case, success of locking in facilitating guidewire or microcatheter advancement after failure to progress with the current equipment, and the number of cases in which at least one major step towards revascularisation was achieved using the device.
DEFINITIONS
A CTO was defined as angiographic evidence of a total occlusion with Thrombolysis In Myocardial Infarction (TIMI) grade 0 flow and estimated duration of ≥3 months. Multivessel disease was indicated by ≥70% stenosis in either of the two major non-target epicardial vessels. Documented lesion characteristics were described according to the J-CTO criteria13. Technical success was defined by TIMI 3 flow and <30% residual stenosis in the target vessel at the end of the procedure. The NHancer was recorded as having contributed a major step towards revascularisation if successful guidewire crossing of either CTO cap (proximal or distal) or the CTO body had been achieved using the device or if the NHancer was the first microcatheter/balloon to cross into the distal vessel. Procedural myocardial infarction was diagnosed by new Q-waves in two contiguous ECG leads and/or rise in high-sensitivity troponin >5-fold above the assay 99th percentile.
STATISTICS
Continuous variables are expressed as means±standard deviation (SD). Univariable and multivariable logistic regression analyses were constructed to identify predictors of technical success. Two-sided p-values of <0.05 were considered statistically significant. All statistical calculations were performed using SPSS, Version 21.0 (IBM Corp., Armonk, NY, USA).
Results
BASELINE CHARACTERISTICS
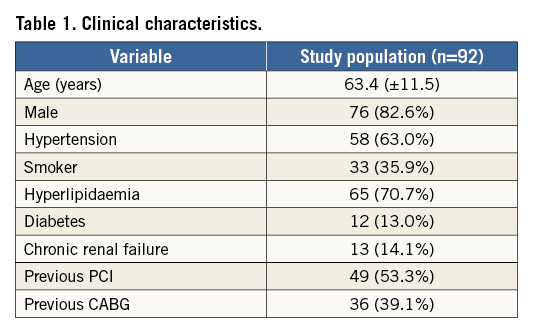
Between July 2014 and November 2014 a total of 92 patients were enrolled. Patient clinical characteristics are presented in Table 1. The mean J-CTO score was 2.79 (±1.36) and 56.6% (52/92) had a J-CTO score of ≥3. CTO characteristics are presented in Table 2.
PROCEDURAL CHARACTERISTICS
Antegrade wire escalation (AWE) was the initial strategy in 82.6% of cases, antegrade dissection re-entry (ADR) in 3.3% of cases, retrograde wire escalation (RWE) in 7.6% of cases, and retrograde dissection re-entry (RDR) in 6.5% of cases. A single strategy was used in 78.3% (72/92) of all procedures and in 79.7% (63/79) of successful cases. The final successful approach was AWE in 73.4%, ADR in 6.3%, RWE in 3.8% and RDR in 16.5% of cases.
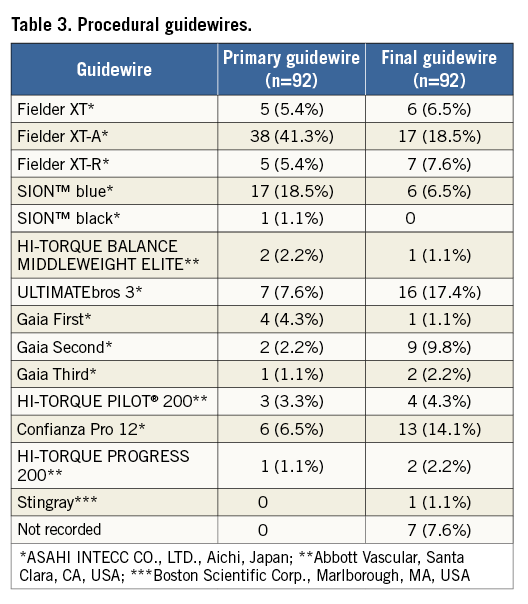
An average of 3.77 (±3.15) guidewires were used per case. Primary and final guidewires are listed in Table 3. Mean procedure time was 89.8 (±46.3) minutes, mean fluoroscopy time was 45.4 (±87.1) minutes, mean estimated air kerma was 1.8 (±1.1) Gray, and mean contrast dose was 221.5 (±92.2) ml.
SUCCESS RATES
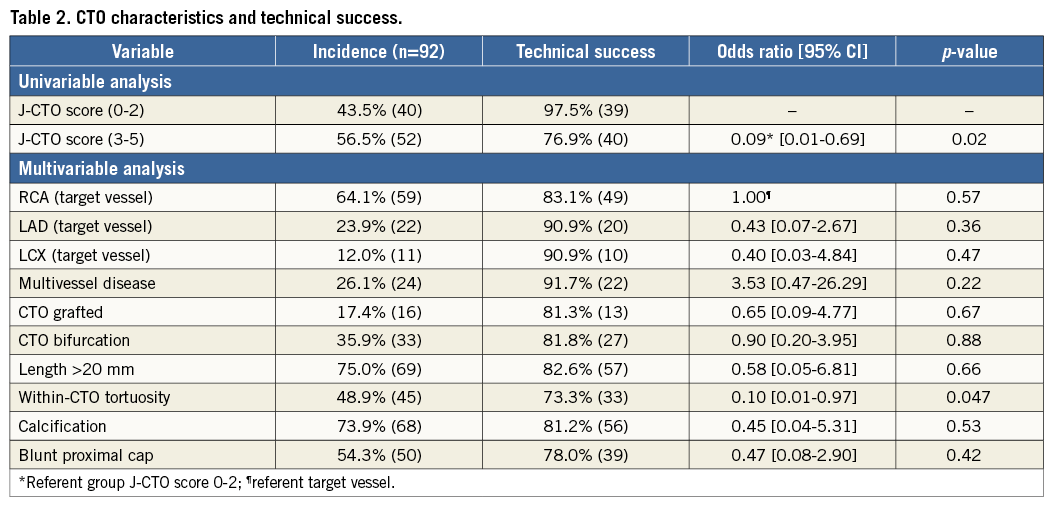
Overall technical success was 85.9% (79/92) for the study group, 97.5% for patients with a J-CTO score 0-2 (39/40) and 76.9% for patients with a J-CTO score of 3-5 (40/52). In 78 of the 79 cases of technical success, stent(s) were successfully implanted.
Within-CTO tortuosity was the only lesion characteristic associated with a reduced risk of technical success (OR 0.10 [0.01-0.97], p=0.047). Technical success was not predicted by calcification (OR 0.45 [0.04-5.31], p=0.53), a blunt proximal cap (OR 0.47 [0.08-2.90], p=0.42) or lesion length >20 mm (OR 0.58 [0.05-6.81], p=0.66).
Locking enabled guidewire crossing, after initial wiring failure, of the proximal cap in 23 cases, distal cap in 11 cases and body of the CTO in 10 cases. Locking also allowed delivery of the NHancer through to the distal vessel in 22 cases. In total, locking was used in 61 cases and assisted successful guidewire and/or microcatheter advancement in 68.9% (42/61) of these cases. Locking did not lead to any loss of position, a need to remove the device or equipment failure.
The NHancer was the only microcatheter required in 68.4% (54/79) of all successful interventions, in 79.5% (31/39) of successful cases in individuals with a J-CTO score <3, and in 81% (51/63) of successful cases resulting from an antegrade approach. In complex (J-CTO score ≥3) and retrograde cases there was a greater requirement for additional microcatheter support (55.8% and 81.2% of cases, respectively). An average of 1.6 alternative microcatheters were used in the 25 successful cases requiring additional support.
The NHancer assisted in overcoming at least one (pre-defined) major step towards successful revascularisation in 85.9% (79/92) of the total study population, irrespective of the final outcome, in 92.1% (58/63) of cases in which the final successful approach was antegrade, and in 68.8% (11/16) of cases in which the final successful approach was retrograde. In 76.9% (10/13) of cases ending in technical failure, at least one major procedural step was achieved using the NHancer prior to case termination.
SAFETY
In terms of procedural complications, there was no incidence of myocardial infarction, emergency surgical revascularisation or death. There was one occurrence of tamponade. This followed wire exit not consequent on locking. The perforation was treated with a covered stent and the case successfully completed. No other perforations occurred. The overall procedural complication rate was 1.1% (1/92).
Discussion
This study demonstrates the efficacy and safety of the NHancer microcatheter in an unselected CTO population. Despite a high incidence of complex anatomy (56.6% J-CTO score 3-5, 39.1% previous CABG), technical success was 85.9% and the procedural complication rate (1.1%) low. In patients with a J-CTO score of <3, technical success (97.5%) approached that of non-CTO PCI.
Locking was easy to apply, did not lead to loss of position and enabled guidewire advancement (after initial attempts had failed) across the CTO cap or body in 23 patients (Figure 2), as well as delivery of the microcatheter through to the distal vessel in 22 patients. Consistent with this success, calcification, lesion length >20 mm and the presence of a blunt proximal cap, traditional markers of fibrocalcific resistance and primary wiring complexity, were not associated with technical failure in this case series. Two of the most common residual failure modes in CTO PCI are an inability to cross the CTO with a guidewire or to deliver equipment through the occlusion after the guidewire has passed11,12. Our initial experience with the NHancer suggests that this novel device, and locking in particular, facilitates penetration or crossing of resistant intimal plaque and would appear to address, at least in part, these prevailing technical difficulties.
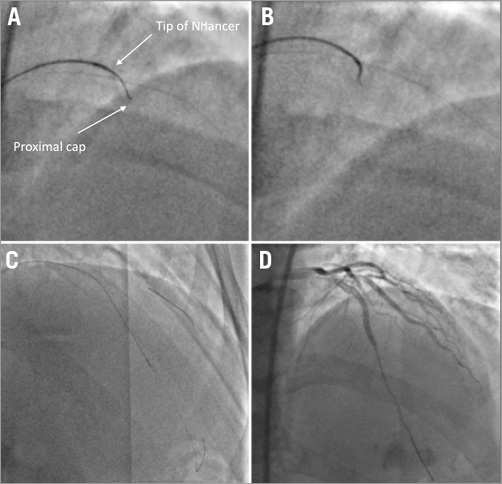
Figure 2. Example of locking used at the proximal cap. After failure to progress at the calcific proximal cap (A), the NHancer was moved closer to the wire tip and locking applied (B). This assisted successful penetration of the cap and subsequent CTO revascularisation (C & D).
There was a high rate of AWE success (initial strategy, 82.6%; final successful strategy, 73.4%) in this study, in keeping with how and where this device performed best. Improving antegrade wire escalation success rates, which have remained relatively static for a number of years, may have a number of advantages beyond increasing technical success alone5,7,14. Many operators are less experienced in dissection/re-entry or retrograde techniques such that complex anatomy or failure to cross the occlusion with AWE can disproportionately affect CTO PCI success, uptake and availability15-18. Furthermore, retrograde procedures are associated with longer case times and higher complication rates, particularly in the learning phase of the procedure19.
Cost-effectiveness and procedural efficiency influence CTO PCI availability and outcomes and are carefully scrutinised in most healthcare systems. The NHancer was the only microcatheter required to complete 68.4% of all successful procedures and 81% of successful antegrade cases. At least one major step towards revascularisation was achieved in 85.9% of patients (79/92) using this device and 62.5% (20/32) of cases in which alternative microcatheter support was required. By limiting the need for additional devices and assisting towards procedural success in a high percentage of cases, we found the NHancer to be an effective first-line CTO device.
Percutaneous CTO revascularisation is predominantly undertaken in stable patients and thus demands a low procedural complication rate. There were no incidences of periprocedural myocardial infarction, emergency surgical revascularisation or death in this case series. The only major clinical event was a single episode of cardiac tamponade that was not directly related to the NHancer. Locking did not result in perforation, loss of position or a need to remove the device.
Locking results in a reduction of tactile feedback and is therefore best applied when the subsequent vessel course is well defined. We would recommend using locking with a non-jacketed wire such as the Confianza Pro 12 (ASAHI INTECC CO., LTD., Aichi, Japan) or Gaia Third PTCA guidewire (ASAHI INTECC). By contrast, there is less rationale for a polymer-coated wire as the increased lubricity is likely to increase the risk of inadvertent subintimal entry. Alternatively, if dissection re-entry is planned, this could be used to the operator’s advantage. On a number of occasions we used locking in an attempt to limit the size of an advancing dissection knuckle and this appeared to be successful. Controlling the subintimal space is important, as excessive disruption can lead to haematoma, compression of the distal landing zone and failed re-entry.
Study limitations
Our case series has a number of limitations. It is a single-arm study that did not include a comparator group. However, as the objective was to describe the first clinical experience of this device and understand the potential of the novel “locking” mechanism, we felt that this study design was appropriate. The total number of CTO cases performed across the six sites during the study period was 255. Not all patients were included, as many of the centres were recruiting to competing studies, some patients declined involvement, each centre was limited to a small number of devices, and use of the NHancer was restricted to one operator (two in Belfast) at each site. Nevertheless, the anatomical and procedural characteristics of our study population are consistent with similar geographical databases including the UK Hybrid and RECHARGE CTO registries, supporting a lack of selection bias20,21. The approach to each case and use of locking were at the discretion of the operator; however, this is likely to provide a more accurate reflection of how the NHancer may be used in everyday clinical practice. The primary approach was antegrade in a high proportion of cases (85.9%) and, given the incidence of complex anatomy, differences in retrograde experience across sites may have influenced initial strategy. No independent angiographic analysis was performed, although in our estimation it is unlikely that this would have altered statistical outcomes.
Conclusions
Guidewire locking with this novel microcatheter assists penetration and crossing of fibrocalcific anatomy with a high degree of safety. Using this device in CTO PCI may lead to improved primary wiring and overall procedural success rates.
| Impact on daily practice This novel “locking” microcatheter may assist primary wiring and overall CTO PCI success by facilitating penetration and crossing of fibrocalcific anatomy with a high degree of safety. |
Conflict of interest statement
J. Spratt is a consultant for Interventional Medical Device Solutions. No sponsorship or funding from Interventional Medical Device Solutions was received for conducting this study. Interventional Medical Device Solutions did not have any role in the design, conduct, analysis and interpretation of data, preparation, review or approval of the manuscript. The other authors have no conflicts of interest to declare.