Abstract
Dual lumen microcatheters (DLMC) have become indispensable tools in the setting of percutaneous coronary intervention (PCI) of chronic total occlusion (CTO). Other than allowing preservation and treatment of bifurcated coronary branches within or in the proximity of the CTO body, they enable the use of modified parallel wiring, antegrade dissection and re-entry, collateral selection and retrograde negotiation of the distal CTO cap. This EuroCTO consensus document describes current DLMC and suggests a practical guide to anatomies and techniques in which these devices are applicable.
Introduction
Microcatheters (MC) are indispensable for contemporary chronic total occlusion (CTO) percutaneous coronary intervention (PCI)1,2. Dual lumen microcatheters (DLMC) have been introduced more recently and have found multiple clinical applications in CTO recanalisation. This consensus document of the EuroCTO Club describes the technical characteristics of available DLMC and makes recommendations based on an in-depth discussion of their role during the 2020 EuroCTO Club annual meeting in Berlin.
AVAILABLE DEVICES
All DLMC, except the ReCross catheter (IMDS, Roden, the Netherlands), consist of a monorail (rapid exchange) delivery system (distal exit port), combined with an over-the-wire (OTW) lumen (proximal exit port). Radiopaque markers are used to identify the exit ports (Figure 1). An overview of available devices and their characteristics is presented in Figure 1 and Table 1.
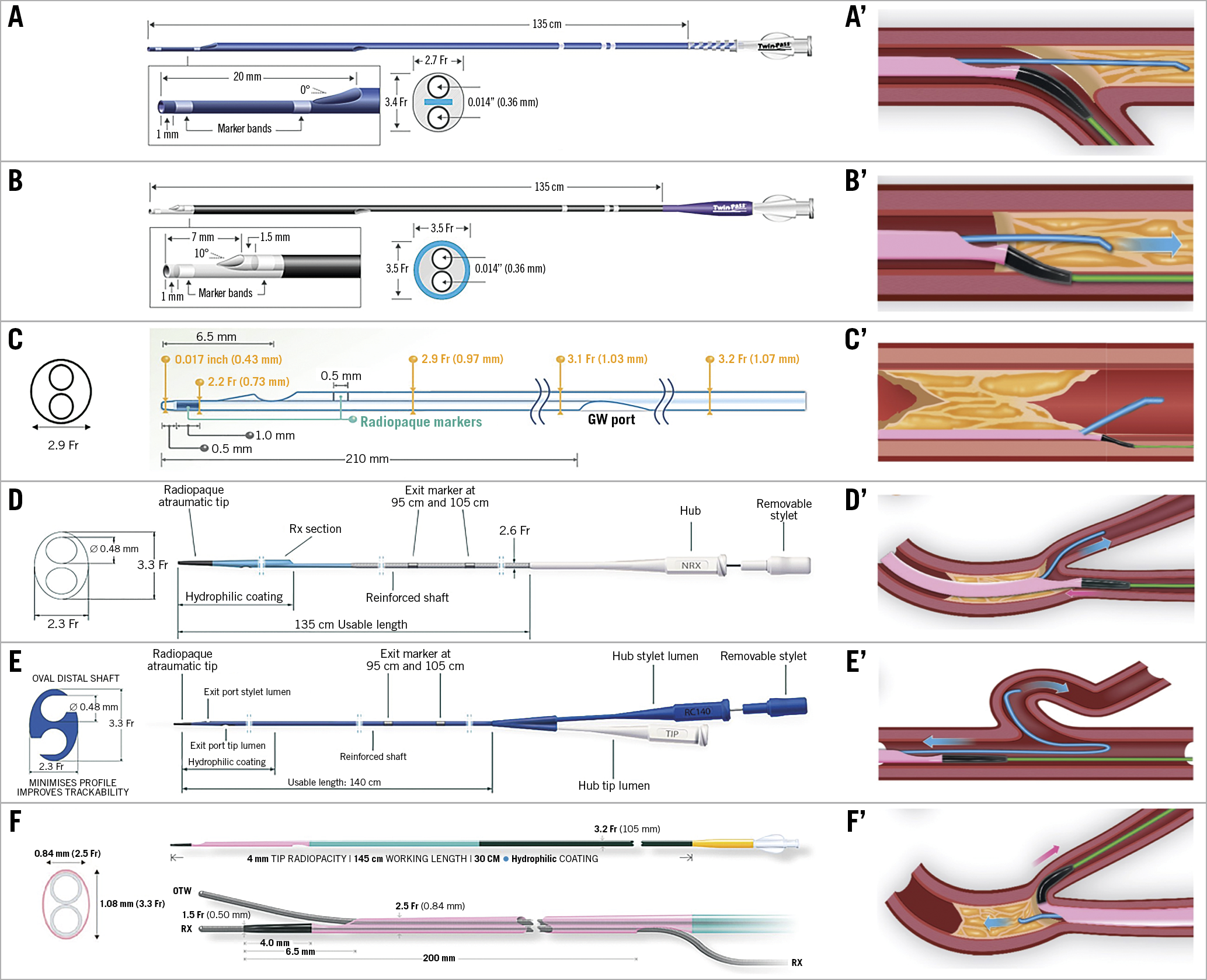
Figure 1. Available dual lumen microcatheters and different techniques of use. Left panel: Principal dual lumen microcatheters in use and their dimensional characteristics. A) Twin-Pass (Teleflex). B) Twin-Pass Torque (Teleflex). C) FineDuo (Terumo). D) NHancer Rx (IMDS). E) ReCross (IMDS). F) SASUKE (Asahi Intecc). Right panel: pictorial representation of anatomical scenarios and relative techniques of use for dual lumen microcatheters. A’) Major side branch near the proximal CTO cap. B’) Parallel-wire technique. C’) Distal re-entry. D’) Access of SB at the distal occlusion cap. E’) Selective engagement of angulated collaterals, using the reverse wire technique. F’) Retrograde crossing and retrograde puncture of the distal CTO cap. Acknowledgement: images of the SASUKE microcatheter, as shown in the right panel, were made by VP Medical and are used with proprietary permission from Asahi Intecc.
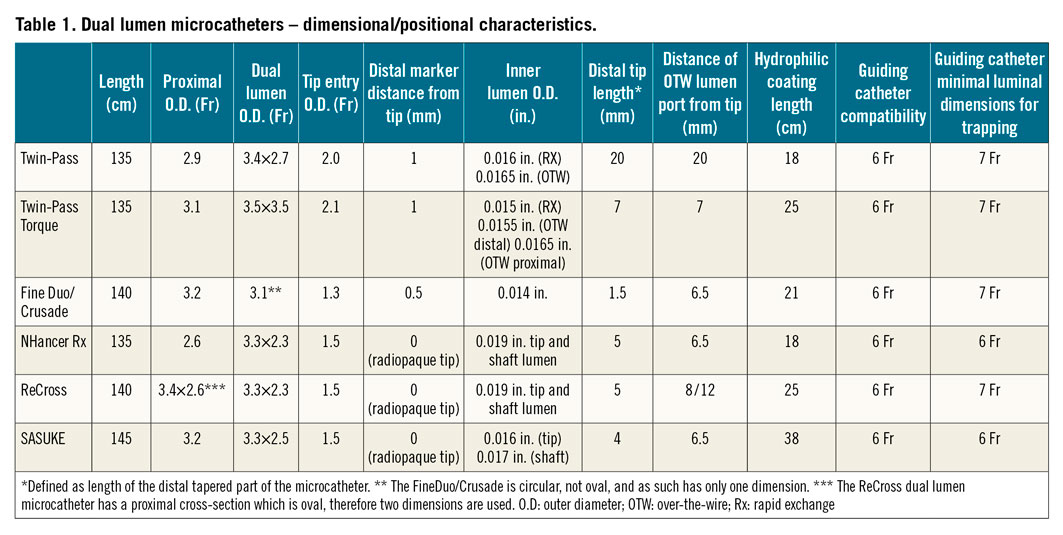
The Twin-Pass® (Teleflex Medical, Wayne, PA, USA) (Figure 1A) is 135 cm long and has a tip-to-OTW-lumen distance of 20 mm. A modification of this catheter (Twin-Pass® Torque; Teleflex Medical) (Figure 1B) has been introduced with a tip-to-OTW-exit port distance of 7 mm and a 10-degree deflection. The main technical innovation of the Twin-Pass Torque is braiding along the catheter. This should theoretically facilitate torquing towards the desired direction (proximal cap, distal true lumen, side branches [SB]); however, in practice this feature is limited by the ability of the operator to control the direction of the distal port.
The FineDuo®/Crusade (Terumo/Kaneka, Tokyo, Japan) (Figure 1C) is a hydrophilic coated DLMC with an OTW lumen and a rapid exchange lumen, with a 1 mm radiopaque marker on the rapid exchange lumen, positioned at a 0.5 mm distance from the distal tip.
The NHancer Rx (IMDS) (Figure 1D) has the smallest crossing profile (2.3 Fr) and uses a removable stylet in the OTW lumen to facilitate advancement.
The ReCross (Figure 1E) has the unique characteristic of having two OTW lumens with the proximal exit port at 12 mm from the tip, positioned opposite the distal exit port.
The SASUKE® (Asahi Intecc, Aichi, Japan) (Figure 1F) is the longest DLMC (145 cm) and is intended to be used both for antegrade and retrograde procedures, taking advantage of the hydrophilic coating of the distal 38 cm. It has an oval design with the OTW exit port having a 20-degree deflection positioned at 6.5 mm from the tip.
Insertion of DLMC is straightforward but removal can be cumbersome as co-ordination is required between two operators to ensure that the OTW and monorail wires both remain in position within the coronary arteries. Balloon trapping is highly recommended to facilitate this manoeuvre but requires a 7 Fr guide catheter, except for the NHancer Rx and the SASUKE.
RECOMMENDATIONS OF USE, CLINICAL INDICATIONS AND TECHNIQUES (Figure 1)
MAJOR SIDE BRANCH NEAR THE PROXIMAL CTO CAP (Figure 1A’, Moving image 1)
Many CTO proximal caps occur at or close to a SB. In this case, the use of a standard microcatheter may be limited by wire prolapse into the open SB, as a result of either unfavourable angulation or the wire following a lower resistance pathway (where the proximal cap is fibrotic or calcified). Under these circumstances, a DLMC placed on a workhorse wire that is sited distally in the SB provides a stable platform for proximal cap penetration, as the operator can control the wire direction towards the CTO cap better whilst also augmenting penetration force in this direction (Ochiai M. Wire Design and New CTO Technologies You May Not Have Yet. Presented at CTO 2014, New York, USA). After successful penetration of the proximal cap, the DLMC should be exchanged for a conventional MC.
PARALLEL WIRE TECHNIQUE (Figure 1B’, Moving image 2)
The parallel wire technique is an integral part of the modified hybrid algorithm recently proposed by the EuroCTO Club3. This technique may be an option in cases where, during antegrade wiring, subintimal tracking occurs. As an alternative to a single wire negotiation to gain access to the true lumen beyond the distal CTO cap, parallel wiring requires the use of a second wire to gain distal luminal wiring, while the first wire remains as visual reference and material that occupies the proximal entry in the subintimal space. In this context, a DLMC can be used over the first guidewire (placed subintimally). Of note, there are no data that support one strategy or device over another. Individual operators need to consider the balance among safety, physician experience, equipment availability and the overall cost of the procedure. The presence of the potential for the loss of a distal SB should still prompt assessment by intravascular imaging to clarify the intravascular course of the second wire after it has reached the distal lumen.
DISTAL RE-ENTRY (Figure 1C’, Moving image 3)
Some operators have been using DLMC in a Stingray-like technique, inserting the DLMC beyond the distal CTO cap, in order to allow re-entry by puncturing the true lumen using the OTW guidewire. We do not encourage this practice because there is a dedicated device that allows a more precise and safer re-entry (Stingray™; Boston Scientific, Marlborough, MA, USA) directing the wire towards the distal true lumen. We acknowledge however that there are some special circumstances when using a DLMC can be considered as an alternative. These are namely: (i) failure of Stingray delivery; (ii) unavailability of the technology; and (iii) clinical investigational purposes.
ACCESS OF THE SB AT THE DISTAL OCCLUSION CAP (Figure 1D’, Moving image 4)
In case of antegrade wiring, particularly in longer CTO lesions, the guidewire may re-enter beyond a bifurcation. Subsequent stenting will seal a tissue flap over the other branch, resulting in its closure and making rescue highly unlikely. Once the CTO is crossed with confirmed lumen entry at the bifurcation, a DLMC can allow safe wiring of the second branch. This will allow kissing inflation or two-stent techniques, as clinically indicated, to manage the bifurcation itself.
SELECTIVE ENGAGEMENT OF ANGULATED COLLATERALS (Figure 1E’, Moving image 5)
This application of DLMC is not limited to CTO but it is especially helpful in retrograde recanalisation whenever it is necessary to engage septal or epicardial collaterals originating with retrovert angles. Following wire engagement, the DLMC can be removed and exchanged for a conventional MC in order to cross the collateral, minimising the risk of trauma. An optimal entry view is recommended, and the use of gentle lubricious guidewires is recommended. Occasionally, the angulated collateral can be engaged using in combination a DLMC and the so-called “hairpin” guidewire technique (180-degree reverse angulated polymer jacket guidewire [SION® black; Asahi Intecc] that is being pulled back, until its tip engages the ostium of the collateral)4. Whilst DLMC may be helpful, a pre-shaped MC (angled tip SuperCross™; Teleflex) or the Venture® catheter (also Teleflex) may prove more helpful in extreme angulation.
RETROGRADE CROSSING AND RETROGRADE PUNCTURE OF THE DISTAL CTO CAP (Figure 1F’)
DLMC are often useful for a distal cap bifurcation, in exactly the same manner as they are for solving proximal cap crossing. They can be considered for this use provided that it is safe to pass them through the collateral (septal with or without dilation with a small balloon and especially in bypass grafts). Their use retrogradely via epicardial collaterals is strongly discouraged. Indeed, the latter can lead to trauma of the collaterals due to the direct contact of the monorail guidewire with the collateral lumen. Retrograde parallel wiring is unreasonable, considering that a retrograde dissection-re-entry technique is far more efficient and safer for the patient.
Conclusion
There is growing interest in the application of DLMC, especially in CTOs with proximal or distal caps at large bifurcations, and for parallel wiring. A systematic approach is required to exploit all the potential of this important addition to the CTO armamentarium.
Acknowledgements
The late Professor Anthony Gershlick contributed to the debate on this subject providing support and advice as a long-standing member of the EuroCTO Club.
Conflict of interest statement
S. Pyxaras reports proctorship and consultancy fees from Boston Scientific, and speaker honoraria from Abiomed and AstraZeneca. T. Levèfre has received consultancy fees, proctoring fees or speaker honoraria from Abbott, Boston Scientific, Shockwave Medical and Terumo. O. Goktekin reports proctorship and consultancy fees from Boston Scientific, Asahi, Terumo, Medtronic, and Abbott. C. Di Mario receives research or educational grants from Abbott, Amgen, Asahi Intecc, AstraZeneca, Boston Scientific, Cardinal Health, Behring, Chiesi, Daiichi Sankyo, Edwards, Medtronic, Menarini, Pfizer, Sanofi, Shockwave, Teleflex, and Philips/Volcano. K. Mashayekhi has received consultancy fees and speaker honoraria from Abbott, Abiomed, Asahi Intecc, AstraZeneca, Biotronik, Boston Scientific, Cardinal Health, Daiichi Sankyo, Medtronic, Shockwave, Teleflex, and Terumo. A. La Manna reports personal fees from Asahi Intecc, IMDS, Terumo Italia, Kardia, and GADA Italia. N. Boudou reports consultancy, and proctorship for Boston Scientific, Terumo, and Asahi Intecc. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Case example of a major side branch near the proximal CTO cap: ostial occlusion of a LAD with retrograde filling over the RCA. A DLMC was used to puncture the proximal CTO cap antegradely using a stiff guidewire.
Moving image 2. Case example of parallel wiring using a DLMC: the first wire is subintimal (rapid exchange port), while the second wire (OTW port) finds its way to the distal true lumen of the LAD.
Moving image 3. Case example of distal re-entry using DLMC: initially, subintimal tracking of the distal RCA. The wire is left in place and – over a DLMC – the second wire performs a puncture into the distal true lumen of the vessel.
Moving image 4. Case example of access to the SB at the distal occlusion cap: the distal CTO cap consists of a bifurcated segment of the Cx; after antegrade wiring of the first marginal branch, a DLMC is positioned over the first guidewire and, subsequently, a second wire passes safely to the second major side branch.
Moving image 5. Case example of selective engagement of angulated collaterals using the “hairpin” technique, as well as retrograde crossing and retrograde puncture of the distal CTO cap.