Introduction
In percutaneous coronary intervention (PCI), the reduction in catheter diameter has been reported to decrease the occurrence of bleeding complications at the puncture site1 and subjective discomfort.2
The outer diameter of the sheath, whose inner diameter is the same as the catheter size, is approximately 2 Fr sizes larger than the catheter size. For example, the outer diameter of a 5 Fr guiding catheter is equal to the outer diameter of a 3 Fr sheath. Thus, it is an attractive idea to insert a guiding catheter directly, without using a sheath, in order to reduce complications at the approach site.
In recent years, sheathless guiding catheters have been developed to reduce catheter size.3,4 Recently, a virtual 3 Fr PCI by WORKS system (Medikit Co., Ltd. Tokyo, Japan) was reported.5 Since the outer diameter of the 5 Fr guiding catheter is approximately 2 Fr sizes smaller than a conventional guiding catheter system, this system ensures a less invasive angioplasty and a puncture site injury equivalent to a conventional 3 Fr introducer sheath.
Here we report on a case of complex PCI in both left and right coronary arteries using a 5 Fr Ikari type guiding catheter6 and the WORKS system, which is equivalent to a 3 Fr sheath size.
Device description
The 3 Fr central dilator (WORKS, Medikit Co., Ltd. Tokyo Japan) used in this case was an inner catheter with a total length of 117 cm. This dilator can be placed in a regular 5 Fr guiding catheter, and is compatible with a 0.025 inch guidewire (Figure 1).

Figure 1. System components: A 0.025 inch guidewire and a 3 Fr central dilator were inserted together into a 5 Fr guiding catheter.
The tip is sharp, and it has a smooth tapered design to reduce the clearance gap between the catheter and the guidewire. This is the first system that supports insertion of a 5 Fr guiding catheter without a sheath to our knowledge.
Technical specifications
The method of insertion of the 5 Fr sheathless guiding catheter is as follows:
After puncturing the radial artery with a 22 gauge needle, a 0.018 inch guidewire was advanced (Figure 2A and 2B).
Figure 2. A: After puncturing the radial artery with a 22 gauge needle, a 0.018 inch guidewire was advanced. B: Removal of a 22 gauge outer needle. C: A 3 Fr sized short dilator was inserted, and the 0.018 inch guidewire was exchanged for the 0.025 inch guidewire with a length of 260 cm into the radial artery. D: Insertion of a 5 Fr guiding catheter and manipulation with the central dilator.
A 3 Fr sized short dilator was inserted and the 0.018 inch guidewire was removed. A 0.025 inch guidewire with a length of 260 cm was inserted into the radial artery up to the ascending aorta (Figure 2C). The unit of the guiding catheter and long dilator were inserted on the 0.025 inch guidewire into the ascending aorta (Figure 2D). The central dilator was removed and the catheter was engaged into the coronary artery.
Case detail
A 78-year-old male with effort angina was treated with PCI. Angiography showed a 90% stenosis in the proximal left anterior descending artery (LAD) which straddled over the diagonal branch (Figure 3A), and a 90% stenosis in the right coronary artery (RCA) (Figure 4A).
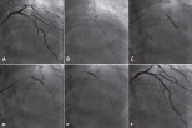
Figure 3. A: A control angiogram of the left coronary artery showing stenosis of the mid-LAD. B: An Athlete slender 01 guidewire and a TEN-NYO 0.010 inch guidewire were advanced into the LAD and the diagonal branch, respectively. IVUS was performed on the LAD side. C: A 3.0 x 23 mm Cypher stent was deployed in the distal LAD at 16 atm. D: A 3.5±18 mm Cypher stent was deployed in the proximal LAD at 16 atm. E: A 3.5±15 mm and a 2.0±15 mm Ikazuchi-X (0.010 inch guidewire compatible balloons) were advanced into the LAD and the diagonal branch, respectively. The final KBT was performed at 10 atm. F: Final angiogram of the left coronary artery.
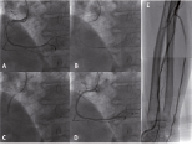
Figure 4. A: The guiding catheter used in treating the LAD was turned over and an angiogram of the right coronary artery was obtained. Stenosis of the proximal RCA was observed. B: The guidewire used in treating the LAD was advanced into the RCA and IVUS was performed. C: A 3.0±23 mm Cypher stent was deployed at 16 atm. D: Final angiogram of the RCA. E: Angiogram of the radial artery after completion of the procedure.
A 5 Fr Ikari L4 guiding catheter (Terumo, Tokyo, Japan) was inserted according to the method described above using the transradial approach. Two 0.010 inch guidewires, an Athlete Slender 01 (Japan Life Line Inc., Tokyo, Japan) and a TEN-NYO (Kaneka Medix, Osaka, Japan) were inserted into the LAD and the diagonal branch, respectively. Intravascular ultrasound (IVUS) (View it; Terumo, Tokyo, Japan) was possible (Figure 3B). Two Cypher stents (3.0±23 mm and 3.5X18 mm; Cordis, Johnson & Johnson, Warren, NJ, USA) were deployed in the mid-LAD and the proximal LAD at 16 atm (Figures 3C and 3D). Then, two Ikazuchi-X balloons 3.5±15 mm and 2.0±15 mm balloon (Kaneka Medix) compatible with the 0.010 inch guidewires were advanced and a kissing balloon technique (KBT) was performed at 10 atm (Figure 3E and 3F).
Next, the guiding catheter was engaged into the RCA as reported by Youssef et al.6 The IVUS was performed on the TEN-NYO guidewire (Figure 4B). A Cypher stent (3.0±23 mm; Cordis, Johnson & Johnson, Warren, NJ, USA) was implanted to mid-RCA at 16 atm (Figures 4C and 4D).
Angiography was performed via the guiding catheter pulled back to the radial artery. No spasm was observed at this site, and adequate antegrade blood flow was maintained to the distal radial artery (Figure 4E).
No haemorrhage or haematoma was observed at the puncture site during the PCI procedure (Figure 5A). Haemostasis was performed using a haemostatic device which used compression pressure, adjusted with a strap (Adapty; Medikit Co., Ltd. Tokyo Japan) (Figure 5B). The next morning, the patient was discharged uneventfully from the hospital.
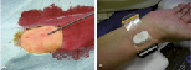
Figure 5. A: Puncture site during the procedure. B: Compression haemostasis after completion of the procedure.
Discussion
There had been limitations in devices and techniques in a 5 Fr guiding catheter. However, KBT is possible with a 5 Fr guiding catheter using 0.010 inch guidewires and specialised balloons compatible with a 0.010 inch guidewire.7 In addition, high success rates have been reported for CTO, even with a 5 Fr guiding catheter.8 Despite the slender guiding catheter size, there is still a considerable number of small female patients with small radial arteries not suitable for a 5 Fr sheath.9 Systems smaller than the 5 Fr would therefore be welcome. Since the outer diameter of a 3 Fr sheath is approximately equal to the outer diameter of a 5 Fr size guiding catheter, there is a reduction of approximately 2 Fr sizes by direct insertion of guiding catheter without a sheath. It enables transradial intervention (TRI) in patients with small radial arteries. However, the limitations of this method are low backup force and difficulty in catheter replacement.
The Ikari guiding catheter has been demonstrated to have stronger backup force in TRI than the Judkins type or other backup types of guiding catheter.10 The shape of the Ikari guiding catheter is also very useful as a catheter for dual use in the left and right coronary arteries with high success rate (98.2%).6 Thus, the use of an Ikari guiding catheter may overcome the limitations of the method without a sheath. A 5 Fr catheter without a sheath can reduce the likelihood of bleeding complications because of equality to 3 Fr size.
Conclusion
We reported a case of complex PCI with a treatment size of 3 Fr, including IVUS, KBT and the treatment of both the left and right coronary arteries using a single guiding catheter without a sheath in a single procedure.

