Abstract
Aims: To evaluate the efficacy and safety of a 5-in-6 double catheter (DC) technique during transradial complex PCI compared to a conventional buddy-wire or balloon-anchoring approach.
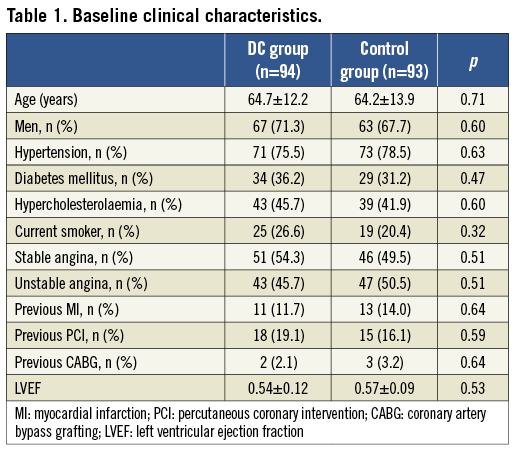
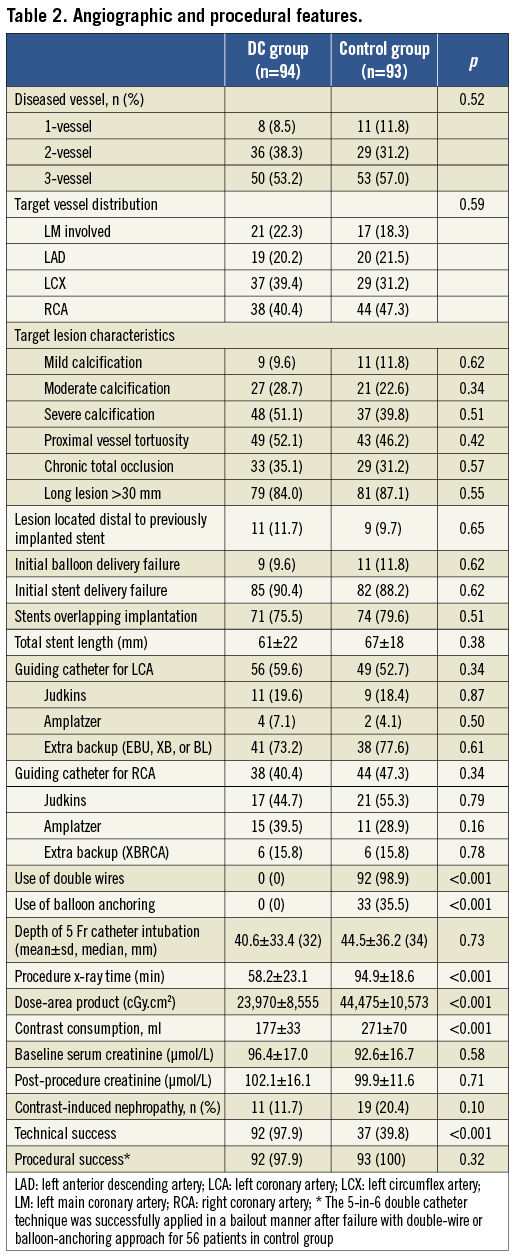
Methods and results: One hundred and eighty-seven patients who failed in stent or balloon delivery after successful wiring of the target vessel were prospectively randomised to further treatment with a 5-in-6 DC technique (DC group, n=94) or by a conventional buddy-wire or balloon-anchoring approach (control group, n=93). Baseline clinical and lesion features were comparable between the two groups. The primary endpoint of technical success was significantly higher in the DC than in the control group (97.9% and 39.8%, p<0.001). Fifty-six patients (60.2%) in the control group with failure of the buddy-wire or balloon-anchoring approach achieved successful PCI with bailout use of a DC technique. Procedural x-ray time (58.2±23.1 min vs. 94.9±18.6 min, p<0.001), patient dose-area product (23,970±8,555 cGy.cm2 vs. 44,475±10,573 cGy.cm2, p<0.001) and contrast consumption (177±33 ml vs. 271±70 ml, p<0.001) were significantly reduced in the DC group. One-year major adverse cardiac event-free survival did not differ between the two groups (89.4% vs. 84.9%, p=0.36).
Conclusions: The use of a 5-in-6 DC technique, especially as a bailout strategy, is a more effective back-up support of the guiding system, subsequently facilitating the success of transradial PCI for complex coronary lesions, than a conventional buddy-wire or balloon-anchoring approach.
Introduction
The contemporary management of coronary artery disease relies more and more on percutaneous techniques, and a transradial approach is now being increasingly adopted for arterial access during percutaneous coronary intervention (PCI)1-3. Despite remarkable advances in interventional devices, in PCI techniques and in operator expertise, transradial PCI for several complex lesion subsets, such as severe calcification, tortuous anatomy, chronic total occlusions or lesions located distal to previously implanted stent(s), continues to present technical challenges4,5. Lack of sufficient back-up support to position or deploy a stent properly is frequently encountered during complex transradial PCI6,7. In particular, when severe coronary dissection has been created after balloon predilation, the operator is reluctant to change the guiding catheter in order to avoid subsequent complications8. Thus, techniques for increasing back-up support with the existing guiding catheter and wire in situ are lacking and can be highly useful during complex transradial PCI. Here, we report the results of our study comparing a 5-in-6 double catheter (DC) technique with a conventional buddy-wire or balloon-anchoring approach during transradial PCI for complex lesions.
Methods
STUDY POPULATION
A total of 4,533 patients underwent transradial PCI in Shanghai Ruijin Hospital between March 2006 and July 2010. Among them, 187 consecutive patients initially experienced failure in stent or balloon delivery during transradial PCI due to lack of support strength from the guiding catheter after the wire was placed correctly in the distal vessel lumen. These patients were then randomised 1:1 by a computer-based system to receive further treatment with a 5-in-6 DC technique (DC group, n=94) or by using a conventional buddy-wire or balloon-anchoring approach (control group, n=93). Patients were excluded if they: 1) were treated without applying the above techniques, or failed in PCI for other reasons (e.g., wire crossing failure in chronic total occlusion); 2) had balloon-unexpandable lesions; or 3) received PCI using a 5 Fr guiding catheter only in the index procedure (Figure 1). Baseline characteristics, procedural features and clinical outcomes were compared between the two groups.
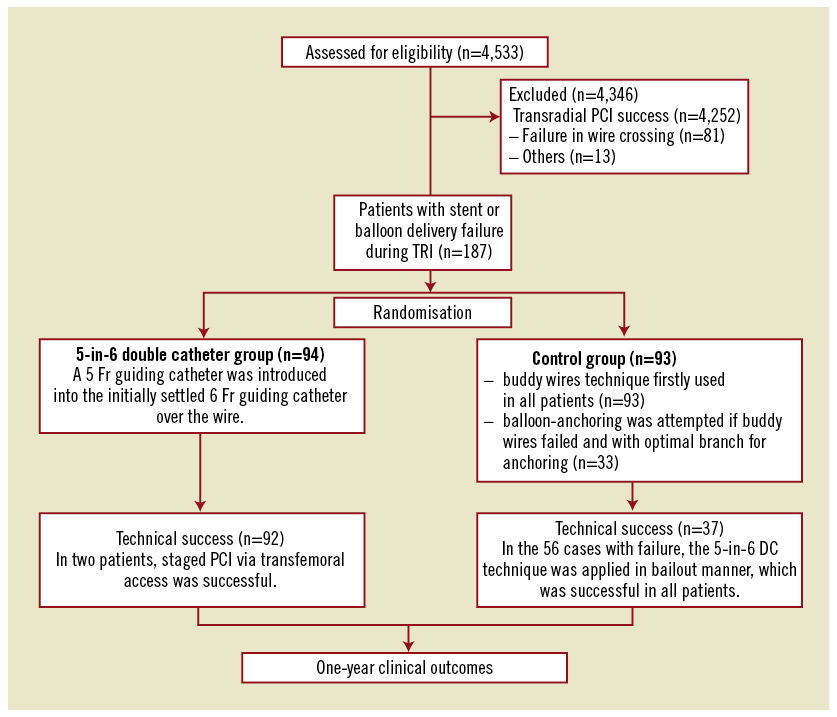
Figure 1. Study flowchart.
The study protocol was approved by the hospital ethics committee. Following an institutional review, written informed consent from the patients was waived, as there were no experimental interventions and patient confidentiality was guaranteed by the study protocol.
MEDICAL TREATMENT AND PCI PROCEDURE
As per protocol, patients were pretreated with a loading dose of aspirin 300 mg and clopidogrel 300-600 mg at least two hours before angiography. Unfractionated heparin was given to maintain activated partial thromboplastin time (APTT) two to three times the normal value during the procedure and over the following 24 hours. Drug-eluting stents (DES) were implanted in all patients. After the procedure, clopidogrel (75 mg/d) was continued for at least 12 months, and aspirin (100 mg/d) was prescribed indefinitely.9,10
Transradial PCI was performed as a default strategy in our hospital from 2005. A 6 Fr guiding catheter was initially used in all patients, but the selection of the type of initial guiding catheter was at the discretion of the operator. Details regarding the 5-in-6 DC method during PCI via transfemoral access have been described previously11. In these cases we introduced the use of a 5-in-6 DC technique during transradial PCI, keeping the initially settled guiding catheter (6 Fr in size) and coronary wire in situ. Briefly, the haemostatic valve was disconnected from the guiding catheter and a 5 Fr Heartrail™ guiding catheter with 0.059” inner lumen diameter and 120 cm length (Terumo Corporation, Tokyo, Japan) was introduced into the guiding catheter over the wire. After the wire protruded out of the 5 Fr guiding catheter, the haemostatic valve was reconnected to the 5 Fr guiding catheter. A balloon catheter could be inflated distally in the target vessel to help deep intubation of the 5 Fr guiding catheter. Stent delivery was then attempted again through the Heartrail catheter with or without repeat balloon predilation (Figure 2 and Figure 3).
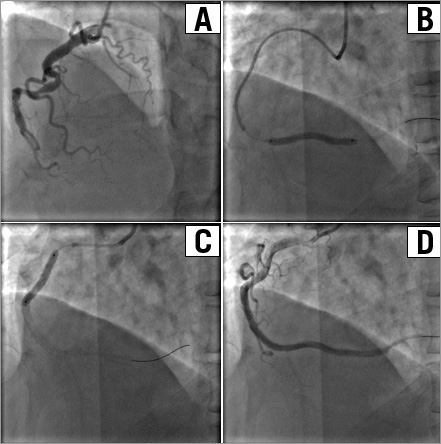
Figure 2. A 73-year-old female patient with totally occluded RCA and proximal tortuous anatomy (A). A 6 Fr XBRCA guiding catheter (Cordis, Warren, NJ, USA) was used. The occluded segment was crossed with a Miracle 3.0 wire (ASAHI Intecc, Aichi, Japan) and predilated with 1.5×15 mm and 2.0×20 mm balloons, but stents could not be advanced through the tortuous mid segment of the vessel. The guidewire was then exchanged for a Runthrough (Terumo Corp., Tokyo, Japan), and a 5 Fr catheter was used and inserted deeply beyond the tortuous mid segment (B). Three Firebird™ stents (MicroPort, Shanghai, China) were deployed successfully (C). Final angiogram showed no residual stenosis with TIMI-3 flow (D).
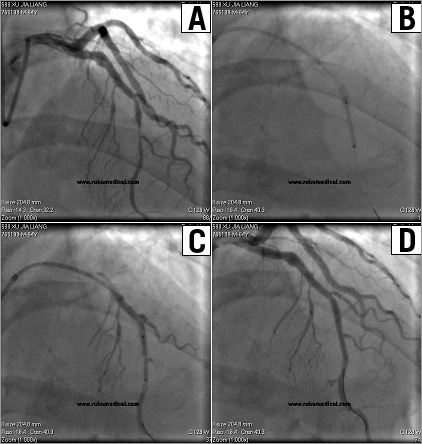
Figure 3. A 64-year-old male patient with unstable angina and stent implantation in the LAD two years ago. Coronary angiography showed a stenosis distal to the LAD stent (A). A 6 Fr XB 3.5 guiding catheter (Cordis, Warren, NJ, USA) was used and the lesion was predilated, but the stent could not pass through the proximal LAD segment (previously stented). A 5 Fr catheter was advanced with the initial guiding catheter and wire in situ, and inserted deeply into the LAD by coaxially anchoring a balloon distally through the 5 Fr catheter (B). A 2.5×18 mm XIENCE V® stent (Abbott Vascular, Redwood City, CA, USA) was successfully deployed through the 5 Fr catheter (C). Final angiogram showed no residual stenosis with TIMI-3 flow in LAD (D).
In the control group, a double-wire approach was attempted in all patients, and a second wire with strong support (e.g., PT Extra Support; Boston Scientific, Natick, MA, USA, or Grand Slam; ASAHI Intecc, Aichi, Japan) was used as the default choice. A balloon-anchoring technique was applied for those with an optimal branch vessel proximal to the target lesion12,13.
For those with stent delivery failure, adequate balloon predilation was routinely performed. The use of a non-compliant balloon with a diameter slightly smaller than that of the target vessel segment was encouraged.
STUDY ENDPOINT AND DEFINITIONS
The primary endpoint was technical success either by a 5-in-6 DC technique or by a conventional approach (i.e., buddy-wire or balloon-anchoring approach), which was defined as a final residual stenosis ≤20% and TIMI-3 flow after stent implantation in the target vessel. Procedural success was defined as immediate angiographic success without major clinical complications (death, myocardial infarction or emergency coronary bypass surgery) during hospitalisation according to ACC/AHA PCI guidelines14. The secondary endpoints included procedure x-ray time, patient dose-area product and contrast use during the index procedure. Contrast-induced nephropathy was defined as a rise in serum creatinine by either ≥0.5 mg/dL or ≥25% from baseline within the first 48-72 hours after PCI9.
Clinical follow-up information was obtained through out-patient clinic visits or by telephone interview with patients or their relatives every three months after discharge and extending to one year for each patient15. Major adverse cardiac events (MACE, including cardiac death, recurrent myocardial infarction and target vessel revascularisation) at one-year follow-up were compared between the two groups. Stent thrombosis was classified according to the Academic Research Consortium (ARC) definition as definite, probable, or possible16.
STATISTICAL ANALYSIS
Continuous variables are presented as mean±standard deviation and were compared using the two-tailed Student’s t-test. Categorical variables were compared with the chi-square test or Fisher’s exact test. MACE-free survival distribution was calculated by the Kaplan-Meier curve and compared by log-rank test. A two-sided p<0.05 was considered statistically significant. Statistical analyses were done using SPSS 13.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
BASELINE DEMOGRAPHICS AND PROCEDURE RESULTS
The two groups did not differ significantly with respect to baseline demographics, lesion distribution and features (Table 1 and Table 2). The major reason for using an additional technique during index PCI was stent delivery failure (90.4% and 88.2% in DC and control groups, respectively), as a result of various target lesion characteristics. The primary endpoint (technical success rate) was significantly higher in the DC group (97.9% and 39.8%, p<0.001). Patients who had failed using a conventional approach were eventually treated successfully with the 5-in-6 DC technique. The 5 Fr catheter could be advanced over the guidewire alone in 119 patients and required a distal balloon to anchor it in 31 (20.7%). The final procedural success rate during the index procedure was high in both groups (98.9% vs. 100%). For two patients with initial failure of stent implantation in the DC group, the target lesions were located at the distal left circumflex or right coronary artery with extreme proximal tortuosity and calcification. They underwent successful PCI after switching to femoral access using a 7 Fr guiding catheter.
Procedural x-ray time was significantly shortened and patient dose-area product was smaller in the DC group. This was mainly due to a higher technical failure rate with the conventional buddy-wire or balloon-anchoring approach, causing the operator to switch to the 5-in-6 DC technique to achieve final procedural success. Likewise, more contrast medium was used in the control group, though the rate of contrast-induced nephropathy did not differ between the two groups (Table 2).
CLINICAL OUTCOMES
The length of hospital stay was similar between the two groups, and seven patients (three in the DC group and four in the control group) experienced periprocedural myocardial infarction during hospitalisation. At one-year clinical follow-up, the MACE-free survival rate was 89.4% and 84.9% in the DC and control groups, respectively (p=0.36) (Figure 4). Four patients (4.3%) in the DC group and five (5.4%) in the control group had definite and probable stent thrombosis (Table 3)
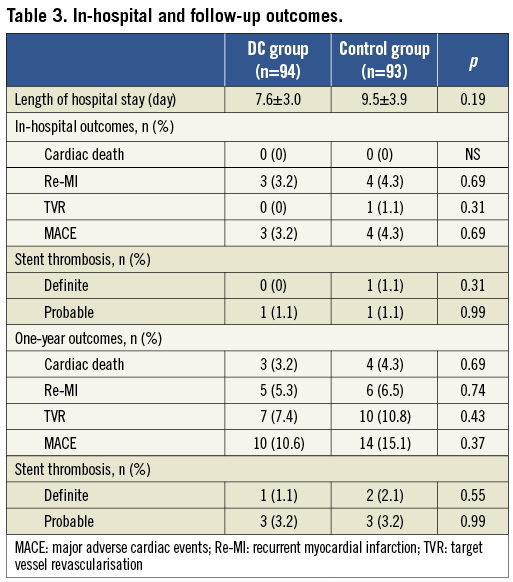
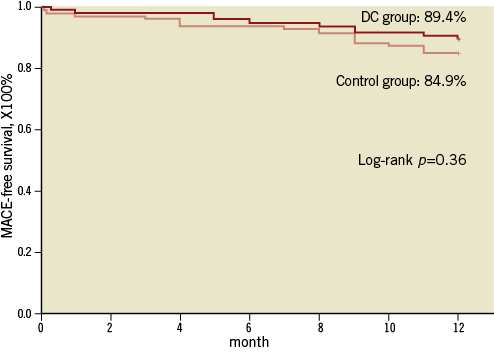
Figure 4. One-year MACE-free survival between the two groups.
Discussion
There has been growing interest in transradial PCI, due to significantly reduced bleeding and access site complications2,3,17. However, with the use of a 6 Fr guiding catheter because of the small calibre of the radial artery, combined with more varied angles to the coronary ostia from the upper extremities, back-up support may be compromised with the transradial approach7. Although this problem can be partly overcome by using specially designed guiding catheters (such as Amplatz, XB and EBU) and improved operator skill18, difficulties in stent implantation may still be encountered particularly during complex PCI for very tortuous or calcified lesions19,20. In these cases, especially after balloon predilation has been performed, operators are usually reluctant to change guiding catheters for fear of losing distal wire access.
This study is the first to compare a conventional buddy-wire or balloon-anchoring approach with a novel 5-in-6 DC technique, and the results indicated that use of the 5-in-6 DC technique was more effective in achieving technical success (97.9% and 39.8%, p<0.001). Moreover, for those who had failed PCI procedure with a buddy-wire or balloon-anchoring approach, bailout use of the 5-in-6 DC technique can also be a good alternative to facilitate successful stent deployment while maintaining existing guide and wire access12,19. Meanwhile, use of the 5-in-6 DC technique resulted in significantly reduced procedural x-ray time, patient dose-area product and contrast consumption. Reduced radiation exposure was reported to be important in lowering the skin injury during PCI for complex coronary lesions20. However, the procedural time is dependent on the operators’ level of experience in the 5-in-6 technique. One-year MACE-free survival was not significantly higher in the DC group (89.4% and 84.9%, p=0.36).
It is noteworthy that deep insertion with a 5 Fr Heartrail catheter (more than 30 mm) was often required and was possible, facilitating sufficient back-up support, coaxial alignment between the catheter and the vessel, and stent delivery. In the current study, the median intubation depth of the 5 Fr catheter into the target vessel was 32 mm, and 34 mm in the DC group with bailout use of DC, respectively, which was greater than that previously reported (20 mm)11. Furthermore, we found that although the 5 Fr catheter could be advanced over the guidewire alone in more than three quarters of patients, the use of a coaxial balloon anchoring (i.e., inflating a balloon at the target lesion while advancing the 5 Fr catheter over a balloon catheter) could help further advancement of the 5 Fr catheter.
In general, the soft and flexible tip of the 5 Fr Heartrail catheter could be inserted deeply into the severely tortuous or calcified segments without trauma to the vessel walls21. Nevertheless, meticulous care should be taken in the manipulation and advancement of the 5 Fr catheter to avoid complications (such as dissection, thrombus formation, or distal embolisation). Pressure damping may occur occasionally after deep insertion of the 5 Fr catheter, but in our experience this did not raise major concerns, and no hydraulic dissections were noted. The diameter of a 5 Fr catheter (1.67 mm) complies well with the inner lumen of a 6 Fr guiding catheter (1.80 mm), avoiding extra bleeding during the procedure. Air trapping and embolism are known to occur with 5 Fr guiding catheters. Thus, vigorous aspiration after set-up of the DC system is required to minimise these possibilities. While inserting a 5 Fr catheter, careful monitoring of the tip of the wire under fluoroscopy is mandatory, especially when using stiff wires (e.g., for chronic total occlusions). With these caveats and with careful attention to detail, in the majority of cases the 5 Fr catheter was able to be advanced just proximal to the target lesion, and stent delivery was then successful. In comparison to the GuideLiner catheter (Vascular Solutions Inc., Minneapolis, MN, USA) with a smallest size of 6 Fr, the current 5-in-6 DC technique is ideally adaptable to the 6 Fr mother guiding catheter in transradial PCI22.
There are a few additional limitations of the 5-in-6 technique. First, because the 6 Fr “mother” guiding catheter is only able to accommodate a single 5 Fr “daughter” catheter, this precludes the use of additional devices between the two catheters. Second, the inner lumen of the 5 Fr catheter accommodates one stent or balloon catheter on a single wire; thus, the two-stent technique or kissing balloon inflation for bifurcation lesions is not feasible. Contrast injection may be limited and may require more force through the 5 Fr Heartrail catheter during stent positioning. While contrast injection through the deeply inserted Heartrail catheter has the potential for hydraulic dissections, the smaller lumen and superselective engagement of the target vessel with a 5 Fr catheter could reduce contrast use during PCI. Careful analysis of the branch vessel and the desired stent position should be determined before deployment. Third, the DC technique may still not facilitate stent delivery in some cases, and conversion to femoral access should always be considered as a final bailout technique during transradial PCI23. Finally, operators’ experience of the 5-in-6 DC technique should be taken into account in the interpretation of the results. Likewise, although this new technique was very successful, the low number of patients enrolled precludes any generalisation of this technique. Also, deep intubation of a vessel is not trivial, and can lead to dissection (even if not seen in the current study). When a stent failed to cross after using only one wire, a buddy-wire technique should still be the first step, if the anatomy is favourable, with a 30% chance of success.
Conclusions
The results of this study demonstrate that the use of a 5-in-6 DC technique, especially as a bailout strategy, is more effective in enhancing the back-up strength of a guiding system, and subsequently facilitates the success of transradial PCI for complex coronary lesions, compared to a conventional buddy-wire or balloon-anchoring approach. One-year clinical outcome after transradial PCI with the 5-to-6 DC technique for these patients with complex settings is acceptable.
Funding
This study was supported by the China National Science Foundation (30900589).
Conflict of interest statement
The authors have no conflicts of interest to declare.