Abstract
Aims: The aim of this study was to compare incidences of radial artery occlusion (RAO) and spasm (RAS) associated with transradial coronary intervention (TRI) using a 6.5 Fr SheathLess hydrophilic-coated guide catheter (SH-GC) vs. a 6.0 Fr Glidesheath Slender (GSS).
Methods and results: We conducted an open-label, single-centre, randomised study to compare radial complications in 600 consecutive patients undergoing elective TRI using 6.5 Fr SH-GC (n=300) or 6.0 Fr GSS (n=300) between 2015 and 2016. The primary endpoint was a composite of RAO evaluated by sonography and symptomatic RAS. The mean diameter of radial arteries was 2.20 mm in both groups; however, the sheath/radial artery diameter (S/RA) ratio was significantly smaller in the SH-GC group (1.03 vs. 1.17, p<0.001). SH-GC was associated with a higher rate of system crossover (1.7% vs. 0.7%, p=0.450) and coronary ostial dissection (1.0% vs. 0.3%, p=0.624), although there were no statistically significant differences. The incidence of major adverse cardiac events was comparable. A lower incidence of RAO and access-site crossover owing to RAS was significantly associated with SH-GC (0.0% vs. 2.0%, p=0.031). Multivariate analysis revealed that a larger S/RA ratio predicted RAO and RAS independently (p=0.007).
Conclusions: The 6.5 Fr SH-GC offers a promising alternative to conventional TRI and is associated with fewer radial complications than the 6.0 Fr GSS.
Abbreviations
AHA/ACC: American Heart Association/American College of Cardiology
CABG: coronary artery bypass graft
CI: confidence interval
GC: guiding catheter
GSS: Glidesheath Slender
MACE: major adverse cardiac events
OR: odds ratio
RAO: radial artery occlusion
RAS: radial artery spasm
SH-GC: SheathLess hydrophilic-coated guide catheter
S/RA: sheath/radial artery diameter
TRI: transradial coronary intervention
TFA: transfemoral approach
Introduction
Transradial coronary intervention (TRI) has been associated with a significant reduction of vascular complications and an improvement in resuming patient mobility, compared with the transfemoral approach (TFA)1,2. Use of TRI may be expanding2, but wider adoption seems to be limited by the occurrence of radial artery occlusion (RAO) and spasm (RAS). The presence of radial arteries smaller than the external diameter of 6.0 Fr introducer sheaths is an inherent risk of post-procedural RAO3. Moreover, RAS causes not only patient discomfort but also procedural failure because of failed cannulation and catheter trapping4,5.
Less invasive TRI devices have been developed to overcome these limitations. The SheathLess Eaucath hydrophilic-coated guide catheter (SH-GC; Asahi Intecc, Aichi, Japan) has a hydrophilic surface coating intended to allow direct insertion via the radial arteries without an introducer sheath6. The 6.5 Fr SH-GC can be used as a 6.0 Fr TRI system and has a smaller external diameter (2.16 mm) than that of conventional 5.0 Fr introducer sheaths (2.29 mm) (Figure 1). A previous study showed that the RAO and RAS rates associated with the 6.5 Fr SH-GC in 146 patients were 0.7% and 0.0%, respectively, with a procedural success rate of 95.2%7. The Glidesheath Slender® (GSS; Terumo Corp., Tokyo, Japan) is a dedicated radial sheath with an inner diameter compatible with 6.0 Fr guiding catheters (GC) and a small external diameter (2.46 mm) because the thickness of the sheath wall has been reduced from 0.20 to 0.12 mm (Figure 1). In a previous feasibility study of 6.0 Fr GSS, the RAO and RAS rates were 0.88% and 4.4%, respectively, with a procedural success rate of 99.1% in 114 patients8.
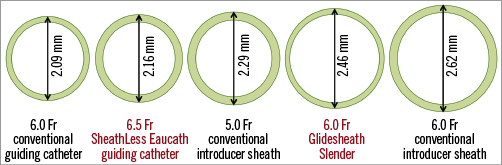
Figure 1. The outer diameters of various sheaths including the 6.5 Fr SheathLess Eaucath guiding catheter, the 6.0 Fr Glidesheath Slender, and the 6.0 Fr conventional guiding catheter.
Although the feasibility of both devices has been confirmed individually, no study has conducted a direct comparison of the incidence of procedure-related RAO and RAS in TRI using 6.5 Fr SH-GC and 6.0 Fr GSS. We performed a randomised trial to compare the incidence of radial complications between these two systems.
Materials and methods
STUDY POPULATION
This study (UMIN000019739) was a prospective, open-label, single-centre randomised trial enrolling patients with coronary artery disease who underwent elective TRI between January 2015 and May 2016. Eligible patients were consecutively included if use of a 6.0 Fr system was planned and were assigned in a 1:1 ratio to TRI using either a 6.5 Fr SH-GC or a 6.0 Fr GSS chosen via sealed envelopes containing random numbers. We excluded patients undergoing emergent revascularisation, those with chronic long-segment total occlusions, those on haemodialysis, and those with a history of coronary artery bypass grafts (CABG) using both radial arteries. Patients requiring an atherectomy with a large rota burr (>1.5 mm) and those with bifurcation lesions requiring a two-stent strategy were also excluded. This study was approved by the institutional review board of our hospital. All patients gave written informed consent.
TRI PROCEDURE
Sublingual nitroglycerine spray was administered to all patients to prevent RAS before local anaesthesia with 2.0 cc of lidocaine 2.0%9. A radial puncture was performed using the Seldinger technique with an 18G needle for both groups. Preprocedural sedation was not performed for any patients.
In patients treated using a 6.5 Fr SH-GC, a 4.0 Fr conventional sheath was initially introduced. The sheath was then exchanged over a J-tipped 0.035-inch wire, and an SH-GC was inserted into the radial artery after making a small skin incision in an access site with a surgical scalpel. In patients treated using the 6.0 Fr GSS, sheath cannulation was performed with a 0.025-inch wire, and a conventional 6.0 Fr GC was used. If TRI could not be completed using the randomised system, a crossover was made to another system and/or access (e.g., femoral) site according to operator decision. At the start of the procedure, unfractionated heparin (7,500 IU) was infused intravenously. Activated clotting time was monitored during the procedure and maintained above 200 sec. The randomised devices were removed soon after TRI was completed. Haemostasis of the access sites was attempted using the TOMETA KUN™ compression system (Zeon Medical, Tokyo, Japan)10. The compression system was deflated at 30 min intervals to 20 mmHg for 120 min, and haemostasis was maintained for six hours at the longest.
ULTRASOUND EVALUATION OF THE RADIAL ARTERIES
Before randomisation, ultrasound evaluation of the radial arteries was performed using a 10 MHz linear transducer. The internal lumen diameter of the radial artery was recorded as the distance between the inner walls by sonographers in the ultrasound laboratory of our institution3. The radial artery diameter was measured to be approximately 1.0 cm proximal to the styloid process, where the puncture was usually made. Operators performing TRI were blinded to the preprocedural radial artery ultrasound findings. Radial artery complications were evaluated using ultrasound at 30 days after TRI again by the sonographers, who were blinded to the randomised TRI procedures as independent observers.
STUDY ENDPOINTS AND DEFINITIONS
The primary endpoint was the composite of RAO 30 days after TRI, defined as absence of antegrade flow on Doppler ultrasound, and symptomatic RAS during TRI. RAS was defined as intolerable pain perceived by patients and/or difficulty of manipulation of sheaths or GCs4. RAS severity was classified as mild (grade 1) to very severe (grade 4) as previously described5. Moderate to very severe RAS (grades 2-4) was defined as symptomatic RAS in this study. Two experienced research staff members adjudicated the incidence and severity of RAS based on patients’ complaints and medical records in the general wards on the day of the TRI procedure. They were blinded to patient randomisation. The secondary endpoints were procedural success without crossover to another system and/or access site, incidences of major adverse cardiac events (MACE), and occurrence of other radial complications within 30 days. Procedural success was defined as post-procedural residual stenosis of <30% and Thrombolysis In Myocardial Infarction (TIMI) grade 3 angiographic flow on final angiography1. MACE included cardiac death, procedure-related myocardial infarction, definite stent thrombosis, and target lesion revascularisation, assessed in the outpatient clinic by attending physicians. The other radial complications included pseudoaneurysm, arteriovenous fistula, and access-site haemorrhage. Pseudoaneurysm and arteriovenous fistula were also evaluated using sonography. Access-site haemorrhage was defined as major if associated with haemoglobin loss of >3.0 g/dl or the need for additional interventions. Minor access-site haemorrhage was defined as local haematoma >3.0 cm diameter without haemoglobin loss of >3.0 g/dl or the need for additional interventions6.
DATA ANALYSIS AND STATISTICAL METHODS
The trial was powered to test superiority of the primary composite outcome. We expected composite RAO and RAS rates of 0.7% in the 6.5 Fr SH-GC group7 and 5.2% in the 6.0 Fr GSS group8. A total of 264 patients per group were chosen to provide >80.0% power and a two-sided α of 5.0% to detect a significant difference in the primary outcome. Categorical variables were reported as percentages and compared using the chi-square or Fisher’s exact test. Continuous variables were reported as means±standard deviation and compared using the t-test. To identify independent predictors of composite RAO and grade 4 RAS, all baseline values of characteristics were pre-screened by univariate logistic regression analysis. Four univariate predictors of RAO and grade 4 RAS were included in a multivariate logistic regression analysis with stepwise procedures where potential predictors were entered and retained in the model at p<0.25. A subsequent multivariate model, including all significant variables, was established to estimate odds ratios (OR) and 95% confidence intervals (CI). Statistical significance was defined as a p-value <0.05. Statistical analysis was performed with JMP® statistical software, version 11 (SAS Institute, Cary, NC, USA).
Results
PATIENT, LESION AND PROCEDURAL CHARACTERISTICS
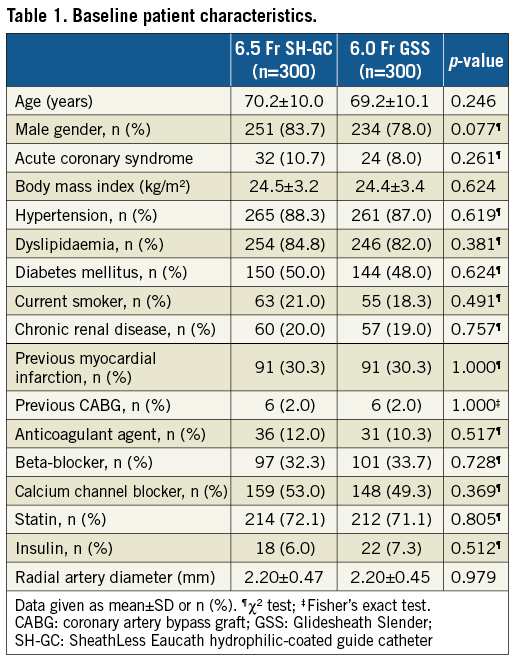
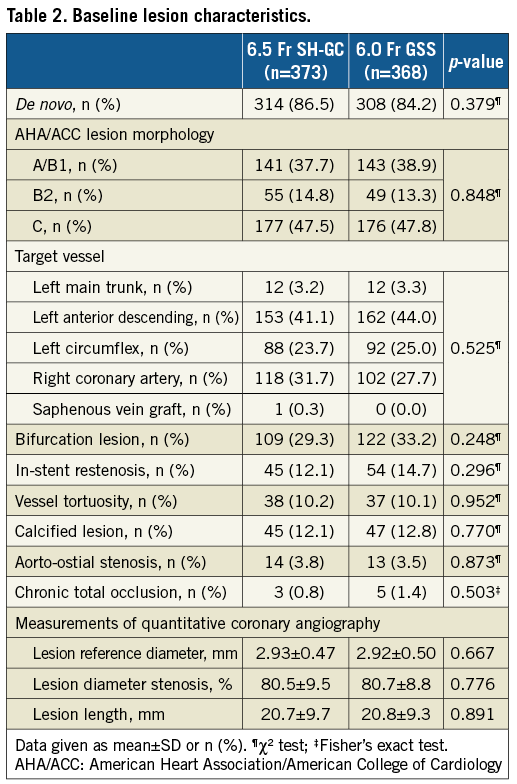
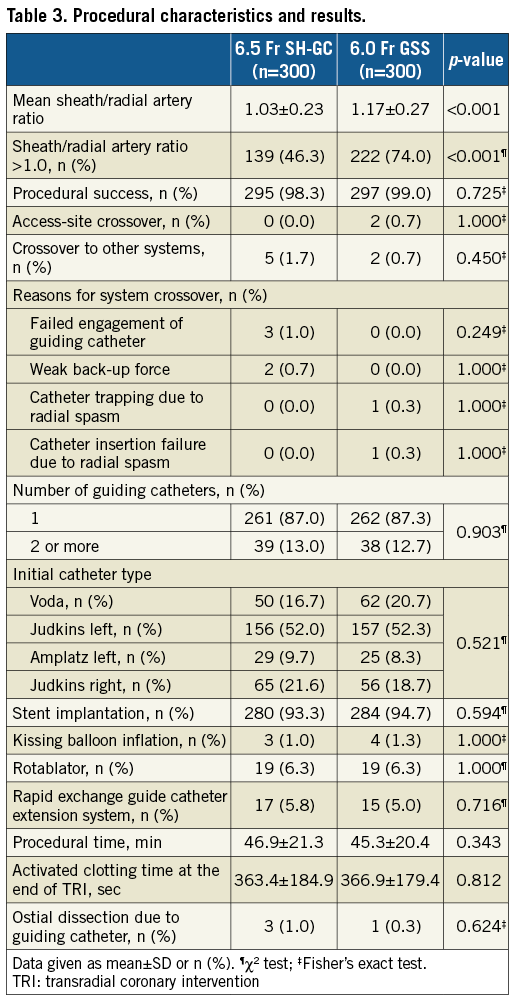
A total of 600 Asian patients with 741 lesions were randomly assigned to elective TRI using either 6.5 Fr SH-GC or 6.0 Fr GSS. The study flow schema is shown in Figure 2. The baseline patient characteristics were similar in both groups, including the preprocedural radial artery diameter (Table 1). The baseline lesion characteristics are shown in Table 2 and the procedural results in Table 3. The ratio of sheath/radial artery diameter (S/RA) was significantly smaller (1.03±0.23 vs. 1.17±0.27, p<0.001) in the SH-GC group (Table 3), because the external diameter of the 6.5 Fr SH-GC is smaller by 0.30 mm than that of the 6.0 Fr GSS (Figure 1). The other characteristics were comparable.
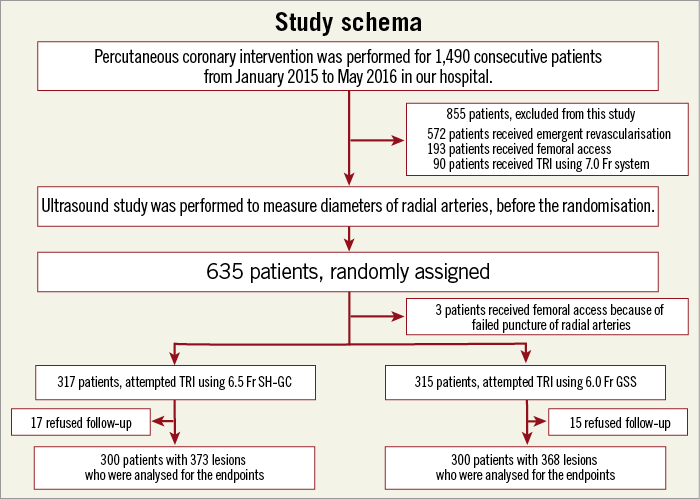
Figure 2. Study schema and flow chart of consecutive patients included in this randomised controlled study to compare the 6.5 Fr SheathLess Eaucath hydrophilic-coated guiding catheter (SH-GC) and the 6.0 Fr Glidesheath Slender (GSS). TRI: transradial coronary intervention
PRIMARY AND SECONDARY OUTCOMES
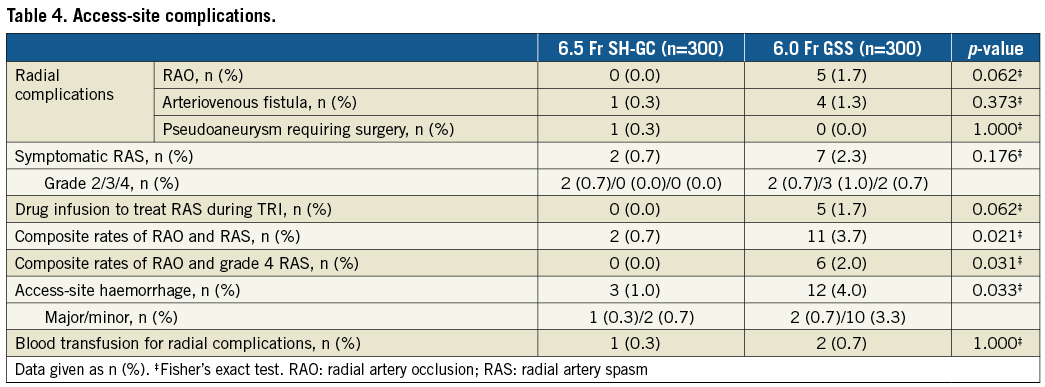
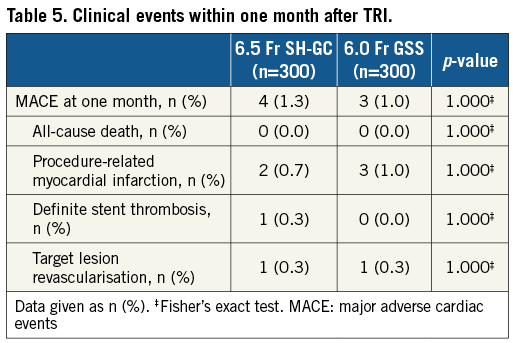
RAO occurred in no patients of the SH-GC group (0.0%) but was observed in five patients of the GSS group (1.7%, p=0.062) (Table 4). Symptomatic RAS during TRI also occurred less frequently in the SH-GC group than in the GSS group (0.7% vs. 2.3%, p=0.176). The primary endpoint of RAO and RAS was significantly less frequent in the SH-GC group (0.7% vs. 3.7%, p=0.021). There was also a significant difference in the composite rate of RAO and access-site crossover owing to grade 4 RAS (0.0% vs. 2.0%, p=0.031). In the GSS group, RAO was detected in four patients, grade 4 RAS in one patient and both complications in one patient. There was a tendency towards a higher rate of system crossover (1.7% vs. 0.7%) in the SH-GC group, although the difference was not statistically significant (p=0.450) (Table 3). In five patients, a 6.5 Fr SH-GC was switched to a conventional 6.0 Fr TRI via the same access sites because of failed engagement or weak back-up force; however, access-site crossover was not performed. On the other hand, in two patients treated with a 6.0 Fr GSS, access-site crossover was required because of catheter trapping or failure of system insertion. There were no between-group differences in MACE onset (Table 5). One patient in the SH-GC group required surgery because of a radial artery pseudoaneurysm. However, the other patients in both groups were asymptomatic and did not experience arm ischaemia and/or additional treatment for RAO or arteriovenous fistula. The rate of major or minor access-site haemorrhage was 1.0% in the SH-GC group and 4.0% in the GSS group (p=0.033) (Table 4).
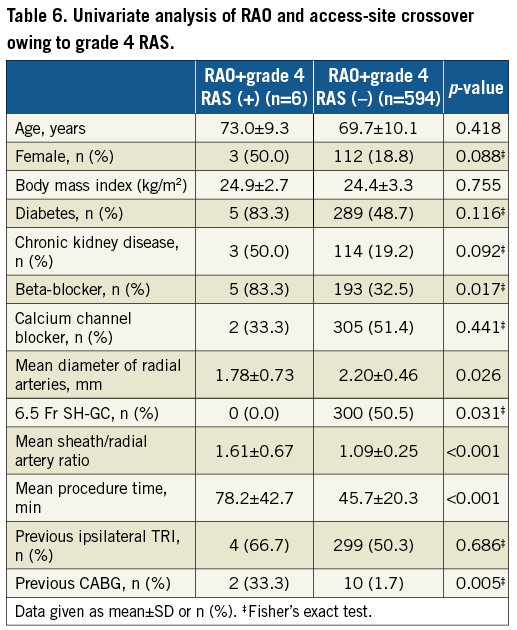
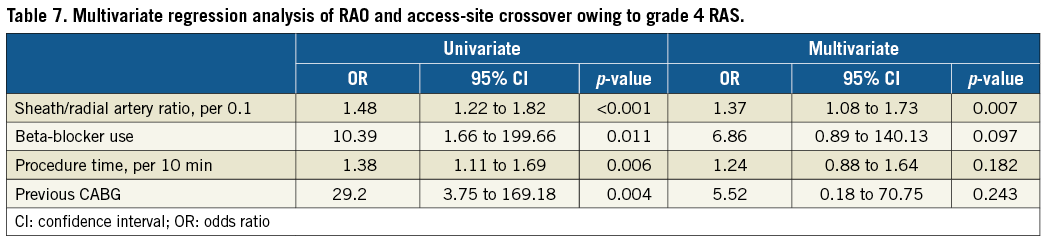
Univariate analysis of factors related to the composite of RAO and grade 4 RAS is shown in Table 6. A greater S/RA ratio, beta-blocker use, longer procedure time and previous CABG were associated with the composite of RAO and grade 4 RAS. The multivariate regression analysis found that a larger S/RA ratio (per 0.1; OR 1.37, 95% CI: 1.08-1.73, p=0.007) was independently associated with the composite of RAO and grade 4 RAS (Table 7).
Discussion
There are three main study findings. First, the composite of RAO and grade 4 RAS was significantly lower in the 6.5 Fr SH-GC group than in the 6.0 Fr GSS group because these complications were independently associated with a greater S/RA ratio. Second, feasibility outcomes, including procedural success and MACE, were not different. Third, access-site haemorrhage was less frequent in the SH-GC group.
To our knowledge, this is the first randomised study to compare the incidence of radial complications between 6.5 Fr SH-GC and 6.0 Fr GSS, although a previous randomised study demonstrated that SH-GC was associated with a higher procedural success rate and less patient discomfort than standard sheaths11. Our study found that the 6.5 Fr SH-GC could prevent serious radial complications compared with the 6.0 Fr GSS, which has the smallest external diameter among the currently available 6.0 Fr sheaths. A meta-analysis of TRI-related RAO demonstrated that the rate of RAO was 11.6% with a 6.0 Fr conventional sheath and that it was strongly influenced by the mismatch of sheath diameter and radial arteries12. The mechanism of RAO is considered to be impairment of antegrade blood flow because of cannulation; severe flow reduction is associated with an S/RA ratio >1.03. Previous studies have shown that the mean inner diameter of adult radial arteries was 2.21 to 2.60 mm, measured by sonography13,14, and Kotowycz et al15 demonstrated that the mean radial diameter was smaller in Asian patients (2.00 mm) than that in non-Asian patients (2.52 mm). Our study included Asian patients, and the mean radial artery diameter was also small at 2.20 mm. This value was greater than the 2.16 mm external diameter of the 6.5 Fr SH-GC but smaller than the 2.46 mm of the 6.0 Fr GSS. Because of fewer patients with an S/RA ratio >1.0, the 6.5 Fr SH-GC might preserve more antegrade radial blood flow and thus reduce post-procedural RAO. Rathore et al4 showed that the RAS rate was reduced by the use of a hydrophilic-coated sheath, which might account for the RAS prevention of the SH-GC. The GSS also has a hydrophilic coating and can be inserted smoothly into radial arteries, but its 16.0 cm length is shorter than the entire length of adult radial arteries. Therefore, a non-coated portion of GCs can come into contact with proximal segments of the radial arteries, and the resulting friction could have induced RAS when GCs were manipulated. In five patients treated using the 6.5 Fr SH-GC in our study, prevention of RAS enabled switching to conventional TRI via the same access sites when revascularisation could not be completed. In contrast, revascularisation could not be completed without access-site crossover in two patients treated using the 6.0 Fr GSS because of severe RAS.
Our study demonstrated the feasibility of the 6.5 Fr SH-GC to reduce radial complications; however, previous reports have suggested that this GC has inherent downsides that need to be better explored6,16. To braid the skin and arterial wall, the SH-GC has a stiffer tip than conventional GCs, and the possibility of coronary ostium injury has been discussed. To avoid this complication, we ensured that SH-GCs were coaxial to the coronary arteries, particularly when injecting the contrast medium. Another limitation is the possibility of less back-up support because of the hydrophilic coating. However, this randomised study showed that the rate of system crossover was not significantly different, and the use of a novel rapid exchange guide catheter extension system was also similar in both groups (Table 3)17. Furthermore, the SH-GC is not always easy to insert into radial arteries. In this study, the SH-GC was successfully inserted in all patients by making a small skin incision at the access sites. Actually, these shortcomings of the SH-GC might not affect procedural success or coronary artery complications significantly, as shown in previous investigations6,7,11.
It should be noted that this patient series included more complex lesions than those of previous investigations using less invasive TRI systems7,18. We excluded only patients requiring TFA and/or a larger GC than 6.0 Fr, and included all consecutive patients planned for elective TRI using a 6.0 Fr system. As a result, 70% of consecutive patients with elective TRI at our institution were randomised (Figure 2), and over 60% of the study patients had type B2/C lesions. Moreover, we performed rotational atherectomy or the kissing balloon technique if necessary. Although previous studies have evaluated the feasibility of less invasive TRI devices such as 5.0 Fr sheath systems7,18, for the most part they included 69% to 80% type A/B1 lesions. Therefore, those devices were used for simple lesions and should not be the preferred initial system. We believe that the 6.0 Fr system should be used as a first-line GC because those smaller than 6.0 Fr have limitations with the use of various devices, and have a potential risk of catheter kinking. Miniaturisation of TRI devices must balance potentially improved safety with the theoretical concern of compromised performance. Therefore, we consider that the 6.5 Fr SH-GC is appropriate for use as an initial TRI catheter, reducing radial complications.
Limitations
Several limitations should be mentioned. First, this was a single-centre study and, even though the sample size was adequate to compare the primary outcome of the study groups, it was relatively small. Second, the primary endpoint was adjudicated by independent observers, but not by an external core laboratory. Third, because our hospital is a highly experienced TRI centre and we are familiar with the SH-GC10,16, the results may not be easily applicable to every operator. Fourth, this study included only Asian patients, who have small radial arteries; therefore, the radial diameter and S/RA ratio may not be the same as those of other races.
Conclusions
The 6.5 Fr SH-GC was effective as an initial GC to perform elective TRI and was associated with a significantly lower rate of radial complications than the 6.0 Fr GSS. This GC is a promising alternative to conventional TRI approaches.
| Impact on daily practice This study noted that the 6.5 Fr SheathLess Eaucath hydrophilic-coated guiding catheter (SH-GC) has a smaller external diameter (2.16 mm) than the mean inner diameter of radial arteries (2.20 mm) in Asian patients. This small ratio of sheath/radial artery diameter had a strong impact on reducing radial artery occlusion, radial spasm and access-site haemorrhage, compared with the 6.0 Fr Glidesheath Slender which has the smallest external diameter among the currently available 6.0 Fr compatible sheaths. Moreover, this study demonstrated that the 6.5 Fr SH-GC could be used in elective transradial coronary intervention for patients with over 60% type B2/C lesions as well as conventional guiding catheters; therefore, we consider that this guiding catheter could be an initial system while preventing access-site complications. |
Acknowledgements
The authors are very grateful to Manami Kumagai, Ai Saito, Shizuka Ito and Nao Abe for their support in data collection.
Conflict of interest statement
The authors have no conflicts of interest to declare.