Irrespective of the outcome of this study, “RAP and BEAT” deserves an award for the most original acronym. In the world of hip hop music, RAP BEAT is a way to spread critical, uncompromising messages, and this is exactly what our Japanese colleagues, under the auspices of the Slender Club Japan (SCJ), have been doing for 10 years. Their message is to “downsize without compromise”.
The use of the radial artery as the default access site for coronary angiography and percutaneous coronary intervention (PCI) undoubtedly reflects an important practice-changing innovation in interventional cardiology. Downsizing equipment is not a goal in itself. It serves to bring the advantages of transradial coronary access (TRA) and transradial interventions (TRI) to patients with small radial arteries, even if their coronary pathology is complex. The armamentarium of the SCJ experts is impressive. Small-bore catheters, sheathless systems, 0.010” balloon and stent catheters are combined using specially designed techniques1.
Downsizing serves other purposes as well. Sheath size is associated with radial artery occlusion (RAO), the dominant complication of TRA2. Use of a smaller sheath reduces mismatch between the radial artery inner diameter (ID) and the outer diameter (OD) of the introduced device, reducing trauma, spasm and RAO. This is of paramount importance since, during the course of a patient’s life, the radial artery will be used more than once. At high RAO rates, TRA and TRI might be victims of their own success. However, smaller sheaths are not always preferable since they limit the use of larger guides for complex PCI. Hence, technical advances allowing reduction of sheath size while maintaining compatibility with larger-bore guides would add to strategies designed to minimise RAO rates. Terumo (Japan) has developed a thin-walled radial artery sheath. The OD of this 6 Fr Glidesheath Slender® (GSS6Fr) is 2.46 mm (a 6.5% reduction compared with a standard 6 Fr sheath) and comes close to the OD of a standard 5 Fr sheath (GS5Fr).
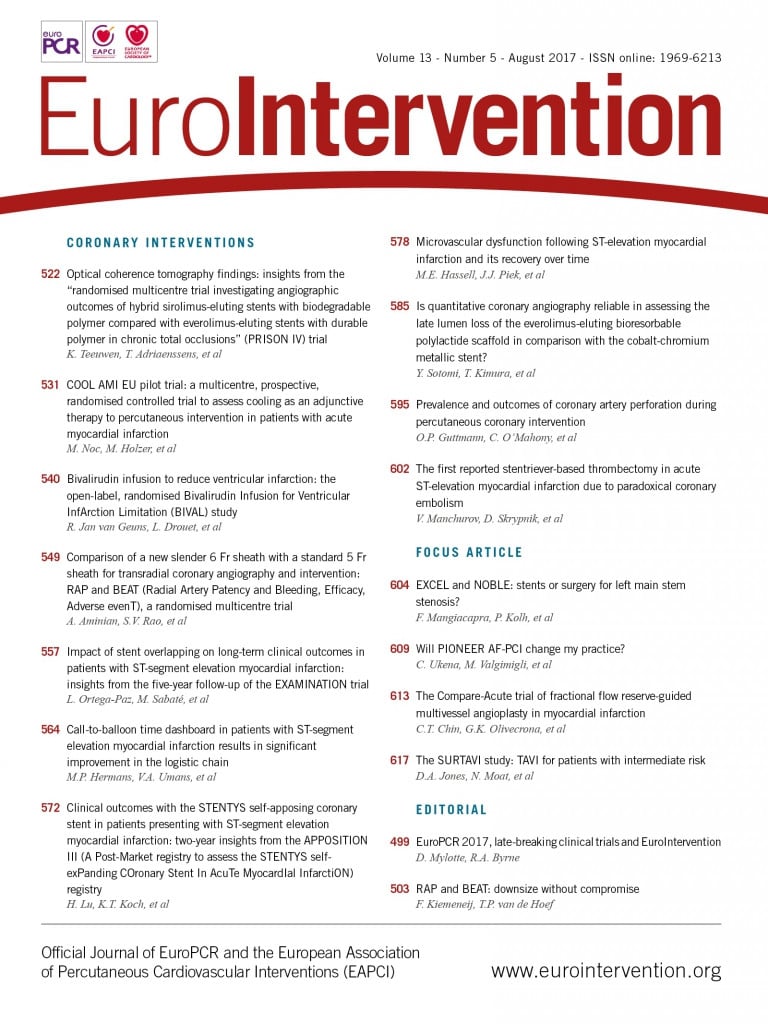
In this issue of EuroIntervention, Aminian and colleagues present a large randomised comparison of this novel sheath with a standard 5 Fr sheath, as well as patent haemostasis versus institutional haemostasis protocols in a 2×2 factorial design3.
The GSS6Fr was documented to be inferior to GS5Fr for the primary endpoint of RAO at hospital discharge. As for the comparison of patent versus institutional haemostasis strategies, no difference in RAO was documented.
According to the authors, the low RAO rates (2.61%) for both arms of the study reflect the expertise in high-volume radial centres and they question the statistical power of the study. However, the use of a set, absolute non-inferiority margin of 2.5% for RAO of the GSS6Fr versus the standard 5 Fr sheath actually biased the study in favour of the GSS6Fr sheath. Also, from a technical perspective, one may wonder how a 6 Fr sheath, even thin-walled, could be non-inferior to a 0.5 Fr smaller 5 Fr sheath. Would a comparison between a GSS6Fr and a conventional GS6Fr sheath not be a more reasonable fight to pick?
Surprisingly, the application of a patent haemostasis protocol did not reduce RAO, despite convincing data4. The authors’ explanation makes sense: patent haemostasis in some form (light compression) is already implemented in all laboratories, irrespective of the local protocol. Actually, two of the 12 institutions involved in the study (responsible for including 434 [23%] patients) already used patent haemostasis as their institutional technique.
Although not described in this analysis, there was significant variation in the duration of haemostasis between centres, which might have influenced outcome, resulting in failure to demonstrate non-inferiority of the GSS6Fr. The impact of haemostasis time on the occurrence of RAO deserves a complementary analysis.
There are important lessons to be learned from this study. First, the use of the GSS6Fr is associated with one of the lowest reported rates of RAO (3.47%) for a 6 Fr catheter-compatible sheath without compromising procedural success rates. This is becoming increasingly important. Whereas the right radial approach is preferred by many operators, crossover to the left radial is frequently required for anatomical or procedural reasons, and left radial access is without doubt more convenient for right-handed patients. However, left radial access leaves the operator in an ergonomically suboptimal position and subject to higher radiation exposure. Distal left radial access has recently been introduced as a more practical route for coronary access5. Yet, more distally, the radial artery is probably smaller and more prone to sheath-to-artery mismatch. For the further development of this technique, advances in sheath technology are crucial.
Second, the usefulness of a time-consuming, strict and systematic patent haemostasis protocol is questionable. A “minimal pressure” strategy associated with early decompression of the haemostasis device may be an alternative approach that can result in low RAO rates.
Conflict of interest statement
The authors have no conflicts of interest to declare.