The birth and growth of transradial access and interventions
Faced with a significant incidence of major bleeding, vascular complications and related mortality following transfemoral artery Palmaz-Schatz stent (Johnson & Johnson) implantation in the late 1980s, research focused on stent design, stent technique, haemostasis techniques, and a proper balance between arterial haemostasis and antithrombotic treatment to prevent stent thrombosis.
It was at this time that Lucien Campeau’s study on transradial coronary angiography was published1 which formed the basis for the cardiology group at the OLVG Hospital in Amsterdam, the Netherlands, choosing to adapt this technique to transradial coronary interventions (TRI). The safety of transradial access (TRA) is determined by the favourable anatomical relationship of the radial artery to its surrounding structures. No major veins or nerves are located near the artery, minimising the risk of injury to these structures. Because of its superficial course, haemostasis can be easily obtained by local compression. Thrombotic or traumatic radial artery occlusion (RAO) does not endanger the viability of the hand as adequate collateral blood supply is usually present. These anatomical aspects should translate into increased safety compared to transfemoral artery access (TFA).
This was the start of an exciting chapter in the history book of interventional cardiology. In those early years, we still needed to wait for the availability of 6 Fr guide catheters, since 8 Fr was the standard. The outer diameter of stent delivery systems was not compatible with the inner diameter of the 6 Fr guides, so stents had to be removed from those systems and manually crimped onto low profile monorail balloon catheters. We also had to deal with the risk of stent loss during attempts to position them correctly, because the available stents were quite rigid and their fixation to the balloons was suboptimal. Needles, sheaths, dedicated guides and haemostasis devices were not yet available, so the whole procedure was quite challenging, requiring multiple manoeuvres to safely place the stent.
The rewards of these technical challenges were clearly evident after stent placement: the sheath could be removed immediately after the procedure, haemostasis was easily established with available tools, and the patient was mobile and self-supporting the moment the sheath was removed. This clinical advantage was striking when compared to those patients who had only undergone transfemoral stent placement and who were bedridden for several days before haemostasis could be achieved. In our early analysis of the first 100 TRI procedures, no bleeding complications were encountered2. Crossover to TFA was necessary in 6 patients.
The first exposure of these results, during the American College of Cardiology (ACC) conference in 1993, resulted in visits to the OLVG Hospital by international colleagues eager to learn this technique. Dedicated TRI courses were organised in Amsterdam, resulting in a growing community of pioneering transradial interventionalists, who started to form circles of knowledge all over the world. The technique was refined, and the medical industry started to develop dedicated tools like needles, wires, sheaths and haemostasis devices. Case reports were published, followed by numerous feasibility studies in all clinical and angiographical subsets, meta-analyses and randomised controlled trials (RCTs).
Transradial access and interventions in the family of guidelines
The advantages of radial access for coronary interventions were immediately seen by the operators after performing only a few procedures, with a dramatic reduction in access-site complications (bleeding, haematoma, need for blood transfusions). These encouraging results were associated with the similar success of angiographic percutaneous coronary intervention (PCI) in single-centre registries. A clear and absolute demonstration of this initial positive feeling was confirmed by the results of RCTs comparing clinical outcomes of PCI following radial access versus femoral access in patients with clinical presentation of high bleeding risk, especially in ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI).
In comparison with TFA, primary PCI in STEMI patients performed via TRA was associated with not only a significant reduction of access-site complications but also a lower mortality rate. Consequently, the different published guidelines established a Class I indication3456.
In 2017, the European Society of Cardiology (ESC) guidelines for the management of STEMI recommended TRA over TFA, if performed by an experienced radial operator, with a Class I recommendation and level of evidence A.
The 2020 ESC guidelines for the management of NSTEMI recommended radial access as the standard approach (Class IA), except in the presence of overriding procedural considerations.
The 2021 ACC/American Heart Association (AHA)/Society for Cardiac Angiography and Interventions (SCAI) guidelines for coronary artery revascularisation established that, in patients with acute coronary syndrome (ACS) undergoing PCI, a radial approach is preferentially indicated compared to a femoral approach in order to reduce the risk of death, vascular complications and bleeding (Class IA). In patients with stable ischaemic heart disease undergoing PCI, the radial approach is recommended to reduce access-site bleeding and vascular complications (Class IA).
Transradial access and interventions in current and future practice
After a long fight between “radialists” and “femoralists”, scientific data has been progressively accumulated, resulting nowadays in the radial approach gaining recognition as the standard approach for unselected coronary diagnostic and interventional procedures (Figure 1). So, what are the challenges TRI faces today and what will the future bring?
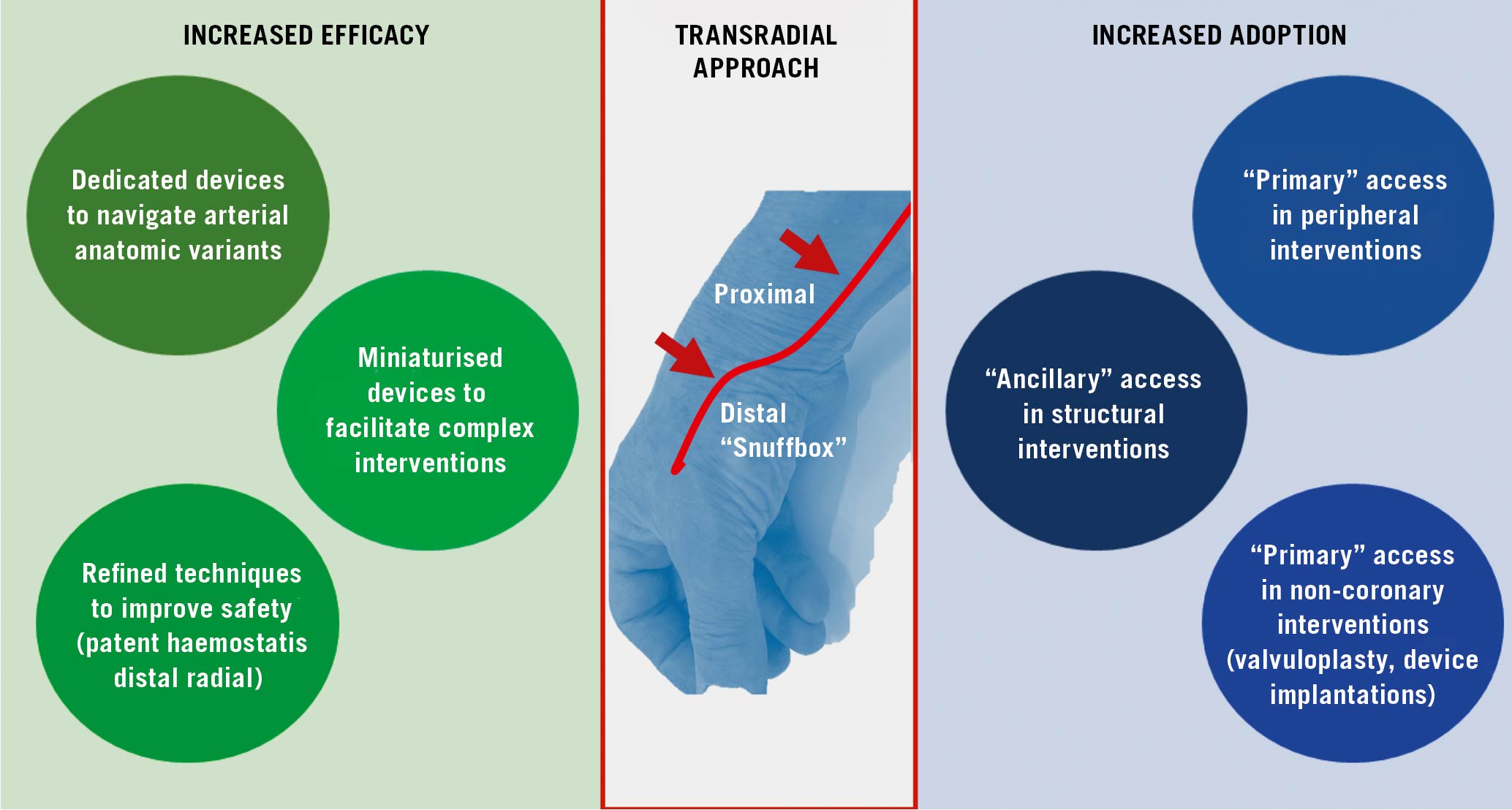
Figure 1. Thirty years in the evolution of transradial coronary interventions: “first-in-man” in 1992 to increased efficacy and adoption in the guidelines in 2022.
In terms of challenges, a sizeable subgroup of patients presents vascular anatomical variants of the arm that continue to hinder catheter advancement and manipulation7. This might result in increased radiation exposure, procedural failures and (rarely) vascular complications. In this regard, improvement in materials is expected to continue to evolve, making TRI suitable for more patients and more procedures. Another well-recognised Achilles’ heel is the preservation of radial artery patency, since RAO might occur after TRA, hindering repeat TRA or surgical arterial grafting. The incidence of RAO can be reduced by employing several simple and effective methods to minimise radial artery injury: reduction in sheath and catheter size, adequate procedural anticoagulation, non-occlusive haemostasis, prophylactic ipsilateral ulnar artery compression, and shorter compression duration. Developed to promote both patient and doctor comfort, the distal radial access technique (distal TRA or “snuffbox access”) has the potential to facilitate proximal radial patency; new scientific data will provide novel insights in this field8.
Last but not least, TRA is just starting to gain respect beyond the border of coronary procedures. In terms of device compatibility and techniques, many endovascular interventions (angioplasty in the iliac-femoral and splanchnic arteries, carotid stenting) have reached the point where operators can switch from a femoral to a radial approach9. Actually, in many catheterisation laboratories, patients are already receiving these procedures transradially from experienced interventional radiologists and neuroradiologists. Furthermore, while the rise of percutaneous cardiac support and transcatheter structural heart interventions is providing a new nobility to femoral artery access, the radial artery has yet to establish its usefulness in this field. Indeed, most new procedures requiring large-bore devices also simultaneously need other forms of arterial access. In this regard, such “ancillary” access selection is not currently being investigated.
In conclusion, the standardisation in the selection of arterial access in cardiovascular interventions has recently begun to be advocated10, and the radial artery is expected to become the primary access point in several settings.
Conflict of interest statement
F. Kiemeneij received speaker fees from Merit Medical. F. Burzotta received speaker fees from Abbott, Medtronic, Terumo, and Abiomed. J. Fajadet has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.