The classic, historical, percutaneous approach
Since their introduction, percutaneous cardiovascular (diagnostic and interventional) procedures (PCP) have progressively gained a key position in the contemporary management of cardiac patients.
The term “percutaneous” comes from the Latin and means “by way of the skin”. The “percutaneous approach” in cardiovascular medicine indicates the possibility of accessing the arterial or veinous system without their surgical exposure. A modified Seldinger technique (based on a needle catheter to get access to the blood vessel, followed by the introduction of a wire through the lumen), “sheath” insertion over the wire and sheath removal by manual compression represent the main steps of the classic percutaneous approach. The common femoral artery quickly gained the position of main access to the left heart ventricle, the aorta, the coronaries and the cerebral or peripheral arteries. Accordingly, “transfemoral” (TF) access represented the “classic” approach for PCP.
Over a number of years, the availability of sheaths of different sizes together with the miniaturisation of devices allowed the expansion of the portfolio of PCP and a reduction in the number of patients unsuitable for PCP.
The evolution of the percutaneous approach
During recent decades, the evolution of cardiovascular medicine has benefitted from PCP improvement and the clinical experience has highlighted two main issues.
First, PCP may offer effective treatment to a variety of patients with coronary, peripheral artery and structural heart diseases.
Second, the possibility of causing vascular damage and haemorrhagic complications is a main limitation of PCP efficacy: cardiovascular patients (often requiring antithrombotic therapy) are particularly prone to developing serious sequelae after such complications. The obvious consequence of such a recognition was that vascular accesses potentially safer than TF access were explored, and refinements for TF access management were sought.
The results of this evolution are right in front of our eyes:
1. An increasing number of PCP are carried out through the small, easily compressible, radial artery so that “transradial” (TR) access has become the most adopted arterial access in catheterisation laboratories.
2. TF access has evolved to become the main access for a (growing) series of PCP (structural heart and aortic interventions) based on bulky devices requiring large-bore sheaths.
Looking for standardisation in vascular access selection and management
The net balance between PCP efficacy and risk is strongly dependent on the ability both to perform technically successful procedures and to minimise complications. Thus, the selection and the management of vascular access during each PCP can no longer be considered just a matter of the physician’s discretion. On the contrary, due to its potential clinical implications, vascular access issues should be regarded as a pivotal aspect in the search for the best care of cardiac patients. In other words, the “modern” percutaneous approach is expected to benefit from a standardisation process with access selection and management as pivotal issues.
Operator experience and comfort is important for PCP efficacy and includes various technical selections including devices and vascular access. However, the best practices for vascular access selection according to the planned PCP, the patient’s clinical conditions, and the local resources have to be established. The search for standardisation should take into account general concepts and local factors. As general factors, scientific clinical data and the approaches of high-volume centres may help to understand which vascular selections have a higher probability of ensuring better safety in different clinical presentations and types of PCP. Among local factors, the skills of the interventional cardiologist, the equipment of each catheterisation laboratory and the composition of local multidisciplinary teams (availability of cardiac and vascular surgeons) are pivotal. These aspects should guide the implementation of changes in local practice in order to standardise vascular access selection and the management of patients.
Is contemporary vascular access selection and management standardised?
The radial approach revolutionised the field of coronary diagnostic and interventional procedures and became the recognised standard approach according to the European clinical practice guidelines on myocardial revascularisation1.
The main limitations of the radial approach are the need for dedicated learning to (safely and successfully) navigate into the arm vasculature variants2 and the possible limitations in sheath size selection. This latter aspect has greatly improved over recent years due to major advances in technology. The classic restriction to 4-6 Fr sheaths in radial access causing difficulty (or impossibility) in using 7 or 8 Fr catheters has now been challenged by the availability of “slender” sheaths, and “sheathless” guiding catheters and systems.
Clinical evidence and technical advances have led to the fact that many catheterisation laboratories performing coronary procedures are now mainly using the radial approach. The number of TF procedures is often very low so that some centres or operators may have limited skills in femoral access techniques. Nevertheless, they can be forced to practise the TF approach in specific subsets of patients (radial access unsuitable or failed) posing technical challenges (peripheral atherosclerosis, vessel tortuosity, etc.). On the other hand, high-volume interventional cardiology teams in large institutions are used to performing various coronary and structural interventions and are therefore using both the radial and the femoral approach on a daily basis. Indeed, the TF approach is advised for structural interventions such as transcatheter aortic valve replacement (TAVR) by valvular heart disease guidelines3 and the use of percutaneous cardiac assist devices is mentioned as a valuable option to treat patients with cardiogenic shock or advanced heart failure in equipped centres1. In these contexts, familiarity with advanced femoral access management techniques may generate the feeling that these techniques may override the safety of the TR access. However, such evidence is not based on solid scientific data. Moreover, best practices regarding the percutaneous selection process and management strategies in patients undergoing complex PCP requiring TF access have yet to be established. As an example, across different European guidelines, the usefulness of a dedicated workup before TF percutaneous coronary intervention (PCI) is mentioned for peripheral artery disease patients only4. Nevertheless, ultrasound-guided catheterisation has been proven to enhance the safety of the TF access5, and a series of different endovascular techniques may be selected to facilitate access management in patients, for example, undergoing TAVR6 or percutaneous cardiac assist device implantation7.
In conclusion, an extreme heterogeneity in vascular access selection and management does exist. Furthermore, existing guidelines mentioning PCP in different clinical settings do not cover important aspects such as preoperative workup, femoral techniques (artery puncture guidance), access-site haemostasis and vascular complication management that may impact on the clinical outcome.
What are the modern best practices in access selection and management?
While looking at the (growing) number of PCP that can be performed in our catheterisation laboratories, four main groups of intervention can be highlighted regarding the vascular access needed:
1. Routine urgent or elective coronary angiography and PCI. These procedures require standard catheters, balloons and stents so that 5-7 Fr sheaths are needed.
2. Elective highly technically complex PCIs. These procedures are performed on an elective basis on specific lesion subsets (severely calcific, complex distal unprotected left main, chronic total occlusion lesions) requiring advanced interventional techniques and devices so that large sheaths (7-8 Fr) and more than one vascular access are often required.
3. Percutaneous cardiac assist devices. These devices have a wide range of technical complexity (from intra-aortic balloon pump to left ventricular assist devices and extracorporeal membrane oxygenation) and may be used in emergency or elective conditions. They are used in very high risk (haemodynamic compromise, poor heart function) patients and require large-bore (≥7 Fr up to 20 Fr) sheaths.
4. Structural cardiac interventions requiring large-bore sheaths. These interventions comprise a growing number of procedures (TAVR, paravalvular leak closure, occlusion device implantation) that may permit the treatment of structural heart diseases (valve diseases, valve prosthesis dysfunctions, heart chambers or large-vessel congenital or acquired diseases) and require large-bore (≥12 Fr) sheaths.
Figure 1 provides a possible algorithm for access selection in different PCP groups and may serve as a basis for further discussion and scientific data production.
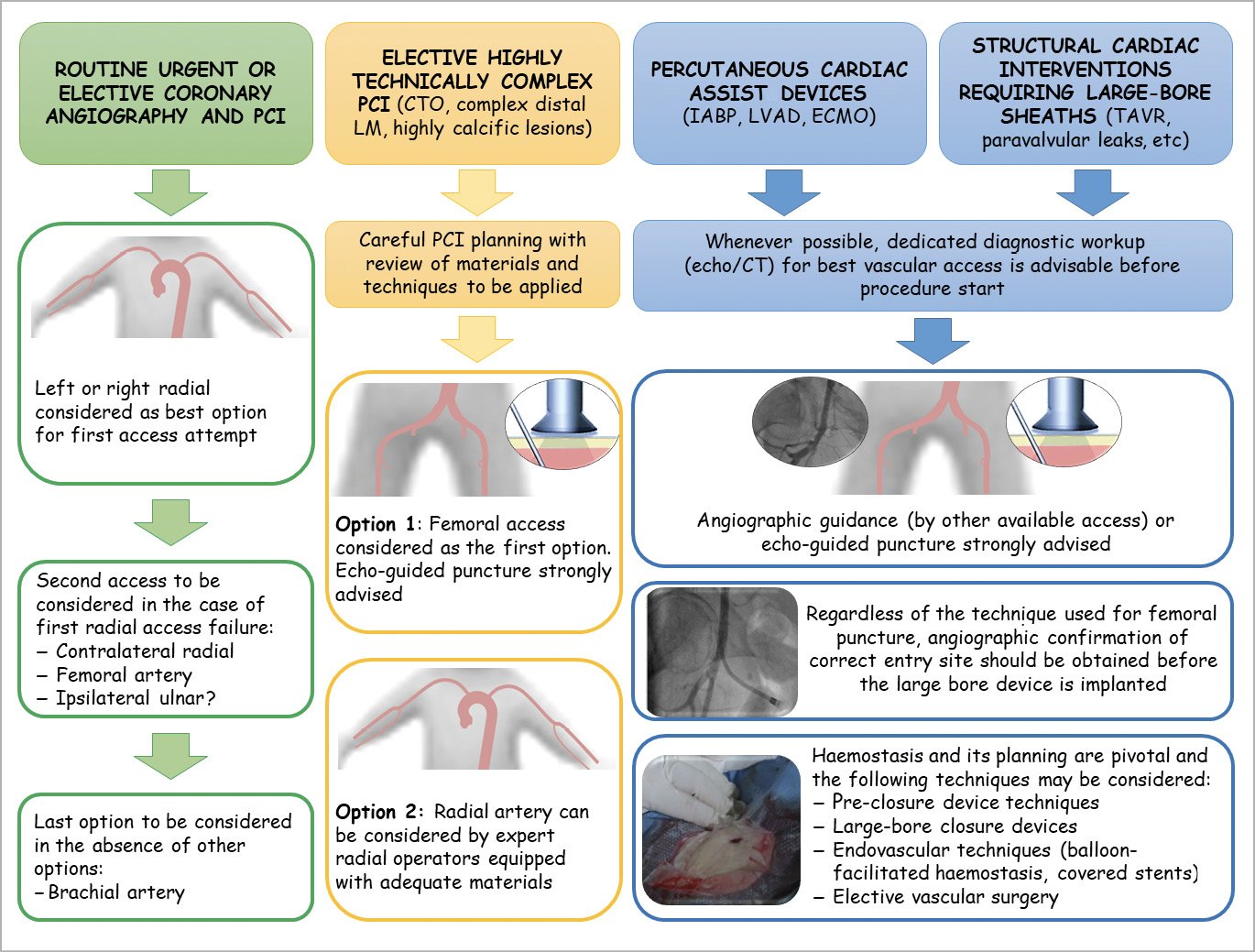
Figure 1. Possible vascular access selection and management according to the type of percutaneous cardiovascular procedure. CT: computed tomography; CTO: chronic total occlusion; ECMO: extracorporeal membrane oxygenation; IABP: intra-aortic balloon pump; LM: left main; LVAD: left ventricular assist devices; PCI: percutaneous coronary interventions; TAVR: transcatheter aortic valve replacement
Conclusion
Vascular access selection and management has the potential to impact on the clinical outcome of patients undergoing PCP. The standardisation of best strategies for vascular access represents an important task for modern interventional cardiology.
Conflict of interest statement
F. Burzotta has received speaker’s fees from Abbott, Medtronic, and Abiomed. D. Dudek has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.