Abstract
Aims: Radial artery (RA) access for PCI has a lower incidence of vascular access-site (VAS) complications than the femoral artery (FA) approach. However, even for default radial operators certain patients are intervened upon from the FA. We examined the demographics and incidence of VAS complications when default radial operators resort to the FA for PCI.
Methods and results: The demographics and VAS complications were compared by access site retrospectively for all PCI cases performed by default radial operators (n=1,392). A modified ACUITY trial definition of major VAS complication was used. FA puncture occurred in 25.2% (351/1,392) of cases. Patients were more likely to be female, older and weigh less than patients undergoing PCI from the RA. The FA procedure was likely to be more complex with larger sheaths, more left main stem, graft and multivessel intervention, and there was a greater proportion of emergency cases. Despite increased case complexity, glycoprotein inhibitors were used less frequently in femoral cases (26.5% vs. 36.8%, p<0.001). A VAS complication occurred in 12.5% (44/351) of cases.
Conclusions: The risk factors for access-site bleeding are disproportionately high in the population requiring FA puncture by default radial operators, and as a result such patients have a high rate of vascular access-site complications.
Introduction
Percutaneous coronary intervention (PCI) performed via the radial route is increasingly the preferred choice among interventional cardiologists worldwide. Over the last two decades, radial access has transformed from being the “alternative” approach, used only if the femoral route was contraindicated, to the “primary” choice. Although patient preference and early mobilisation are recognised advantages of the radial approach, probably the main driving factor behind the change in practice was the increasing recognition that PCI carried out via the traditional femoral approach was associated with higher vascular access-site (VAS) complications which are associated with increased morbidity and mortality1. The radial approach, on the other hand, is associated with significantly fewer access-site complications due to the superficial position and small calibre of the artery which allows better haemostasis. The radial approach also improves patient experience, reduces total hospital costs and facilitates day-case PCI2,3.
However, the radial approach has several known limitations. The radial artery diameter will often limit the use of large sheath sizes, although the use of sheathless guides and downsizing of equipment have reduced the need for femoral bail-out. In addition, the radial artery may be very difficult to cannulate in shocked patients or indeed negotiate because of tortuosity, radial loops and intense vasospasm. Therefore, a default radial operator, driven either by necessity or choice, may default to the femoral approach in a proportion of patients.
The hypothesis of the present study is that the risk factors for VAS complications would be disproportionately high in the population requiring femoral artery puncture by default radial operators, and as a result such patients would have a high rate of access-site complications.
Methods
PATIENT POPULATION
To examine our hypothesis we evaluated the demographics of patients who had PCI performed via the femoral artery by default radial operators, and compared the VAS complication of these femoral cases against the historic published data. The University Hospital of Wales provides cardiac care to a population of nearly 1.5 million and performs in excess of 1,500 PCI a year. Within the department four cardiologists were considered as default radial operators, i.e., cardiologists who choose the radial artery as their primary route in all cases if technically or clinically possible. The analysis included all patients who had PCI performed by these four interventional cardiologists over a 12-month period and compared baseline demographics and procedural variables for their femoral and radial access cases. Data were retrieved from the British Cardiovascular Intervention Society Database Central Cardiac Audit Database (CCAD). Data in CCAD are entered prospectively on an individual patient basis, and included in the database are patient demographics and presentation, procedural characteristics and complications, and patient outcomes. For subsequent analysis data can be extracted from CCAD retrospectively in Excel spreadsheet files and analysed in conventional fashion. A total of 1,352 consecutive patients were included. Clinical outcomes including complication data were derived and cross-referenced from a number of sources including CCAD, internal complications audit, hospital haematology database, hospital transfusion log and radiology department records.
COMPLICATION DEFINITIONS
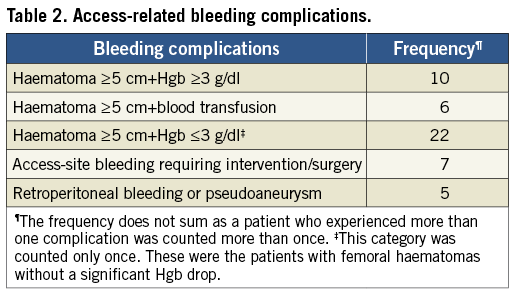
We modified the ACUITY trial bleeding definition recognising only femoral access-site-related complications4. Intracranial and intraocular bleeding were not included as these complications are unrelated to the access site. VAS-related complications were defined as follows: 1) femoral haematomas ≥5 cm, 2) retroperitoneal bleeding confirmed by CT scan, 3) any access-site surgical intervention, and 4) femoral artery pseudoaneurysm confirmed by Doppler ultrasound. For the purpose of data expression, we subdivided the haematomas group into haematomas without significant haemoglobin drop (Hgb drop ≤3 g/dl), haematomas with haemoglobin drop of ≥3 g/dl, haematomas requiring blood transfusion, and haematomas requiring intervention in the form either of surgery or of an external homeostatic device.
DATA ANALYSIS
Continuous variables are presented as mean and categorical data are presented as frequencies and percentages, and are compared using chi-square statistics or a Fisher’s exact test as appropriate. During univariate analysis the majority of the variables captured in the CCAD database were entered. Subsequently, the data were filtered with the irrelevant demographics and procedural information removed, including certain conventional risk factors and procedural details that were not known to contribute to the access bleeding complication. Multivariate stepwise logistic regression analysis was performed by an external statistician with the inclusion of the following variables that were significant in the univariate analysis: sex, age, body mass index, previous PCI or CABG, use of glycoprotein inhibitors, use of special diagnostic or interventional devices (not including rotational atherectomy), use of intra-aortic balloon pump, number of vessels intervened on, left main and graft intervention, and vascular sheath size. A p-value of <0.05 was considered statistically significant.
Results
PATIENT DEMOGRAPHICS AND PROCEDURES
The femoral route was utilised in 25.2% (351/1,392) of cases. With respect to baseline demographics, patients undergoing PCI from the femoral route were more likely to be female (41.5% vs. 21.9%, p<0.001), older (65.1 yrs vs. 63.1 yrs, p=0.003), weigh less than radial cases (80.0 kg vs. 84.2 kg, p<0.001) and have a history of CABG (14.0% vs. 4.1%, p<0.001) or previous PCI (16.5% vs. 13.0%, p<0.003) (Table 1). Closure devices were used in 30.7% of patients undergoing femoral artery puncture.
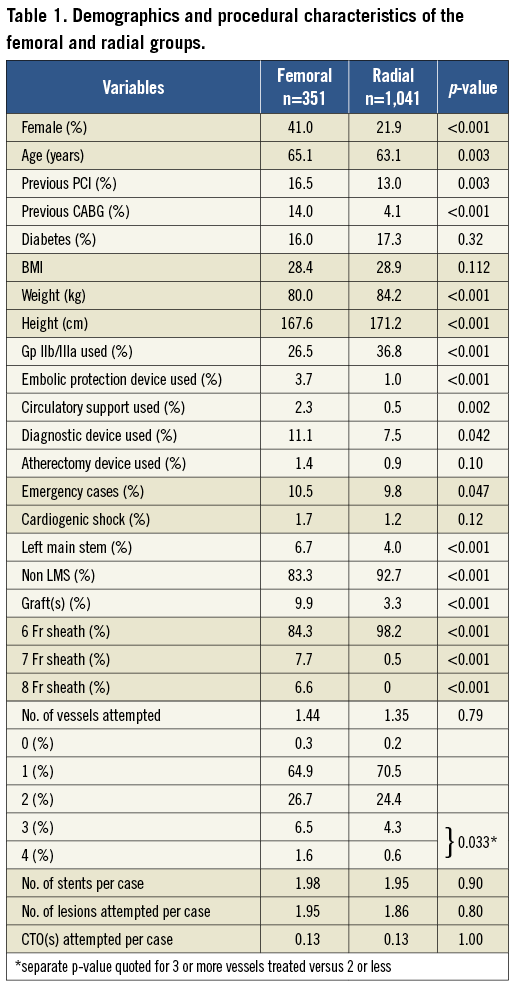
Additionally, the PCI undertaken in patients from the femoral artery was increasingly complex when compared with radial artery procedures. Left main stem intervention (6.7% vs. 4.0%, p<0.001), bypass graft intervention (9.9% vs. 3.3%, p<0.001), 7 Fr and 8 Fr sheath use as well as multivessel PCI were all more likely in femoral cases than in radial cases. Embolic protection devices, such as FilterWire (Boston Scientific, Natick, MA, USA), were used nearly four times more often than in radial cases (3.7% vs. 1.0%, p<0.001). The anticipated need to use intra-aortic balloon pump support, as well as emergency cases, not surprisingly favoured the femoral approach from the outset (2.3% vs. 0.5%, p<0.001). The use of procedural diagnostic devices, such as intravascular ultrasound (IVUS) and fractional flow reserve (FFR) wire, was more frequent in femoral cases (11.1% vs. 7.5%, p=0.042).
There were no differences in the number of stents used, number of lesions and cases of chronic total occlusion attempted. Interestingly, despite this observed increase in case complexity, glycoprotein inhibitors were used much less frequently in femoral than in radial cases (26.5% vs. 36.8%, p<0.001).
The odds ratios for the variables independently associated with femoral access use are illustrated in Figure 1. Independent factors associated with femoral artery access were: larger sheath sizes (OR 34.4), use of circulatory support (OR 4.83), use of an embolic protection device (OR 3.97), history of CABG (OR 3.77), LMS intervention (OR 2.53), multivessel PCI (OR 1.71), and use of a procedural diagnostic device (OR 1.54). Age, sex, and BMI were not independently associated with the use of the femoral artery.
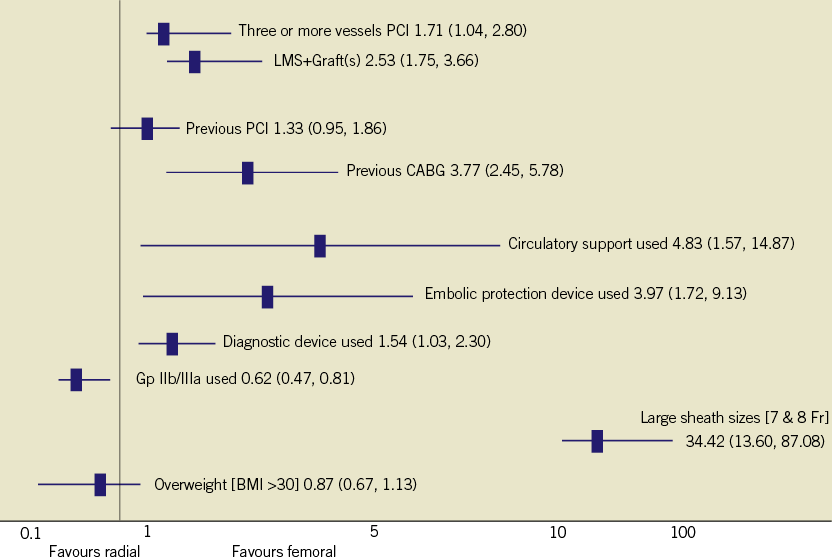
Figure 1. Odds ratios for the variables independently associated with femoral access use.
ACCESS-SITE-RELATED COMPLICATIONS
Forty-four patients (12.5%) in the femoral artery group experienced a VAS-related complication (Table 2). Twenty-two patients developed a haematoma of ≥5 cm without significant haemoglobin drop. Seven patients experienced haematoma with continuous femoral bleeding which required either surgical intervention (two patients) or an external homeostatic device (five patients). Ten patients had haematoma associated with blood loss of ≥3 g/dl, including nine who had additional high-risk features such as blood transfusion (six patients), retroperitoneal bleed (one patient), femoral pseudoaneurysm (one patient) or the use of an external homeostatic device (one patient). Six patients with haematoma underwent imaging investigations (CT and/or Doppler ultrasound scan) with three proven to have pseudoaneurysm of the femoral artery and two retroperitoneal bleeds. There were no VAS-related complication events attributed to a femoral artery closure device.
Discussion
Although historical meta-analyses and recent randomised studies have suggested that the radial approach reduces procedural morbidity and also mortality in certain PCI subgroups, not all patients can be completed without resorting to the femoral artery5-7. In this study it was evident that, when a default radial interventional cardiologist undertakes a PCI from the femoral artery, patients are more likely to be female, older and weigh less than patients undergoing PCI from the radial artery. Additionally, the PCI in the femoral cohort is likely to be more complex with larger sheath sizes, more left main stem, graft and multivessel intervention, with a greater proportion of emergency cases requiring circulatory support. As a result of these associations, a high incidence of femoral VAS complications was observed. Despite the increased case complexity in the femoral cohort, glycoprotein inhibitor use was significantly lower in the femoral cohort, suggesting that interventional cardiologists were cognisant of the increased risk of a VAS complication case irrespective of the potential ischaemic benefit on offer.
The detrimental impact of major VAS complications on patients during PCI has been well documented, and it is a reduction in these events that is likely to be the main driving factor behind the observed morbidity and mortality benefits associated with radial artery access8. Major bleeding is the most common non-cardiac complication for patients with coronary artery disease who have undergone percutaneous coronary intervention (PCI)9. Previous studies have demonstrated that patients who experienced major bleeding had higher in-hospital and one-year mortality compared with patients with minor or no bleeding10. Although comparison between studies is difficult due to variable bleeding definitions, rates of major bleeding between 3.2 and 8.4% are reported in contemporary practice with the femoral arterial puncture site the most frequent source of bleeding11-18. In the present study, femoral VAS complications were observed in 12.5% of patients: this is significantly higher than previously reported in contemporary intervention and probably explained by the disproportionately high number of risk factors for access-site bleeding in the population requiring FA puncture.
Patients in the femoral cohort were more likely to be female than in the radial cohort, and a probable explanation for this observation is the small calibre of the female radial artery. Women are significantly more likely than men to experience a VAS complication during PCI10,19,20. For example, data from the ESPRIT study found that 5.5% of women experienced a VAS complication compared with 2.6% of men21. Our data support this trend with 15.2% of women in our analysis experiencing a major bleeding complication compared with 10.6% of men. Femoral patients in our study were also older, and an excess of radial artery calcification, subclavian tortuosity and aortic dilatation with advancing age may explain femoral bail-out in this cohort. The link between advanced age and vascular complications in PCI has been extensively reported10,22-26. In prognostic risk scoring for bleeding, Nikolsky and colleagues identified older age as the most powerful clinical predictor of major bleeding after PCI24. Similarly, Huynh et al calculated that, for every 10-year increment in age, the risk of bleeding increases by 24%18.
Additionally, the PCI undertaken in patients from the femoral artery was increasingly complex when compared with radial artery procedures. Left main stem intervention, bypass graft intervention, and larger sheaths were all more frequent in femoral cases than in radial cases. Possible explanations for this observation include small radial artery diameter or a perceived lack of guide catheter support from the radial artery, driving radial operators to the femoral approach for complex PCI. Importantly, complex procedures have previously been observed to be closely linked to the occurrence of VAS complications10. The pathophysiological link between complex procedures and vascular complications includes increased procedure length, use of larger sheaths, more intense anticoagulation and additionally perhaps haemodynamic instability. Certainly, the use of intra-aortic balloon pump support was not surprisingly more frequently seen in the femoral cohort (2.3% vs. 0.5%, p<0.001).
Thus these data clearly identify that patients who undergo bail-out PCI from the femoral route by a radial operator are a population at one of the highest risks of a bleeding complication thus far identified in contemporary PCI practice. As such, it is imperative that a clear strategy is developed when dealing with high-risk groups for access-related bleeding. Therefore, all aspects of the case strategy, encompassing further techniques in radial access (such as sheathless guides), careful femoral arterial puncture (guided by x-ray or ultrasound), choice of anticoagulants (the use of bivalirudin has been shown to reduce access-related bleeding over heparin or glycoprotein inhibitors5,27), and femoral arterial haemostasis post procedure (closure devices or early sheath removal), should be carefully considered28,29.
Limitations
Although the femoral crossover rate in our historical study was 25%, our institution - like many high-volume radial centres - is now achieving radial rates of over 90%. However, this smaller “super-selected” cohort is likely to represent an even more extreme subgroup of patients at higher risk of a vascular complication, and therefore the findings of the present study remain important. Additionally, the study only presents observational data rather than clinical trial data. However, no randomised study could provide the insights into the outcome of bail-out femoral access observed. Finally, we do not have data on the relative frequency of bail-out versus elective transfemoral puncture. However, it is usual practice at our institution not to give heparin or to decide on an anticoagulation strategy until it is clear that the case can be completed from the radial artery. Thus, the femoral vascular complication rates should not be influenced by whether it is an elective or a bail-out femoral artery puncture.
Conclusion
The risk factors for access-site bleeding are disproportionately high in the population requiring femoral artery puncture by default radial operators, and as a result such patients have a high rate of VAS complications. The excess of vascular access complications was observed despite a lower frequency of glycoprotein inhibitors in the femoral cohort. Femoral access-site issues are likely to remain a problem even in contemporary practice and they require novel strategies in an attempt to minimise such periprocedural complications.
| Impact on daily practice This study reveals that the patients undergoing PCI via the femoral artery in a default radial centre often have many of the risk factors for vascular complications and major bleeding, and as a result such patients have a high rate of complications. In clinical practice this means that even routine radial operators are likely to face bleeding complications when undertaking a PCI from the femoral artery. Therefore these cases require meticulous peri-procedural and post-procedural care. |
Conflict of interest statement
The authors have no conflicts of interest to declare.

