Abstract
Radial access use has been growing steadily but, despite encouraging results, still varies greatly among operators, hospitals, countries and continents. Twenty years from its introduction, it was felt that the time had come to develop a common evidence-based view on the technical, clinical and organisational implications of using the radial approach for coronary angiography and interventions. The European Association of Percutaneous Cardiovascular Interventions (EAPCI) has, therefore, appointed a core group of European and non-European experts, including pioneers of radial angioplasty and operators with different practices in vascular access supported by experts nominated by the Working Groups on Acute Cardiac Care and Thrombosis of the European Society of Cardiology (ESC). Their goal was to define the role of the radial approach in modern interventional practice and give advice on technique, training needs, and optimal clinical indications.
Introduction
In 1948, Radner1 first described transradial catheterisation using radial artery cut-down. In 1989, Campeau et al revisited Radner’s idea2 and reported on percutaneous entry into the distal radial artery for selective coronary angiography in 100 patients. In 1992, prompted by the need to avoid the frequent femoral bleeding associated with the anticoagulation used at the time of stent implantation, Kiemeneij et al used Dr Campeau’s work as the basis for developing transradial coronary interventions3-5.
Its adoption by some interventionalists demonstrating its feasibility and benefits as well as a growing number of dedicated training courses and workshops helped to expand interest in this technique worldwide. Compared to the femoral access, radial access has been shown to cause fewer complications at the vascular access site, allow more rapid ambulation, offer greater postprocedural comfort for the patient and be cost-effective5. More recently, the radial approach has been shown to confer mortality benefits for STEMI patients and a reduction in mortality, myocardial infarction and stroke for patients undergoing the procedure at high radial volume centres6,7. Radial access use has been growing steadily but, despite these encouraging results, still varies greatly among operators, hospitals, countries and continents.
Twenty years after its introduction it was felt that the time had come to develop a common evidence-based view on the technical, clinical and organisational implications of using the radial approach for coronary angiography and interventions. The European Association of Percutaneous Cardiovascular Interventions (EAPCI) has, therefore, appointed a core group of European and non-European experts, including pioneers of transradial angioplasty and operators with different practices in vascular access supported by experts nominated by the Working Groups on Acute Cardiac Care and Thrombosis of the European Society of Cardiology (ESC). Their goal was to define the role of the radial approach in modern interventional practice and give advice on technique, training needs, and optimal clinical indications.
Position statement on radial approach use in coronary angiography and PCI
FEASIBILITY
The superficial position of the distal radial artery, free of other anatomical structures, makes it easy to find and puncture and safe to compress after sheath removal8. Unlike groin bleeding, subcutaneous bleeding after radial puncture is rapidly noticed by the patient and can be controlled by local compression. The double blood supply of the hand via the palmar arch supplied by the ulnar artery avoids ischaemic complications after radial artery occlusions, which often are asymptomatic9. Although the conventional Allen test to check the efficacy of the dual palmar arch vascularisation has almost been abandoned in routine practice because it is too subjective, it is important to assess good vascular communication between the radial and ulnar arteries using oxymetry or plethysmography which are more objective10,11.
Early trials demonstrated that the risk of access failure was higher with the radial versus femoral approach (7.3% vs. 2.0%, p<0.01)12. However, more recent registries have shown a progressive reduction in the need for conversion (down to 1.5%) due to improved techniques and materials13,14.
Factors influencing feasibility include: radial artery diameter/catheter diameter ratio, anatomical variations and the development of spasm. Operator proficiency and experience with the radial approach greatly influence access feasibility: in the RIVAL trial feasibility improved in centres in the highest tertile of radial approach PCI volume as compared to the lowest tertile, even though all the operators were experts6; moreover, in the PREVAIL study when transradial intervention (TRI) was used in over 85% of cases, the failure rate fell below 4%15. In a recent meta-analysis of randomised studies including only STEMI patients, overall procedure duration was comparable16.
A default radial approach is feasible in routine practice after appropriate training (both in stable and unstable patients including STEMI patients) but proficiency in the femoral approach is required because it may be needed as a bailout strategy or when large guiding catheters are required. Better results with radial access are expected with increasing procedural volume of operators.
SAFETY
BLEEDING
In recent years, the importance of preventing major haemorrhage during and after PCI has been recognised, so that ESC documents and guidelines now recommend a bleeding risk assessment and ischaemic risk stratification to individualise antiplatelet and antithrombotic treatment17-19. Risk factors for bleeding can be classified as patient-related, procedure-related, and drug-related. Patient-related factors like gender, diabetes, renal impairment, hypertension and advanced age are non-modifiable except, possibly, for blood pressure control.
Using radial access significantly reduces procedure access (site)-related major bleeding relative to femoral access, as shown by meta-analyses of randomised studies published both before (OR 0.27; 95% CI: 0.16 to 0.45)20 and after the recent, large randomised RIVAL trial (OR 0.51 95% CI: 0.33 to 0.79)6, as well as by large observational registries21-23. In the National Cardiovascular Data Registry that incorporates 593,094 procedures from 606 institutions, the radial approach was associated with significantly fewer bleeding complications, especially in certain high-risk groups like women and patients with acute coronary syndromes at higher risk for bleeding23. Therefore, in these patients using a more aggressive antithrombotic regimen and radial access has been suggested24, but further studies are needed to assess the safety of this strategy since non-access-site bleeding remains a concern with enhanced antithrombotic therapies25. Indeed, in a recent study, despite the use of radial access26, major bleeding was observed in 5% and it was found to be an independent predictor of death at one month. It should be considered that access-site major bleeding accounts for only 30% to 50% of all major bleeds at longer follow-up27. Recent pooled analysis of three large studies suggests that non-access-site major bleeding more severely affects prognosis and doubles the risk of death relative to access-site haemorrhages27. Numerous studies comparing manual compression and closure devices have shown similar incidence of groin haematoma, bleeding, pseudoaneurysm and blood transfusion, suggesting that radial access combined with optimal anticoagulation remains the safest approach in patients at high bleeding risk28.
The radial approach offers lower access-site bleeding, particularly in patients at higher risk of either ischaemia or haemorrhage. A combined reduction of both access and non-access-site bleeding is expected when radial approach is associated with optimised anticoagulation according to current recommendations.
STROKE
Percutaneous coronary intervention (PCI) carries a low risk of symptomatic cerebral ischaemic damage, but a substantial risk of cerebral embolism responsible for silent cerebral infarction in up to 15-20% of patients29. Potentially, longer procedural time and catheter manipulation in or close to neck vessels constitute risk factors for cerebral embolisation30-32. However, this has never been confirmed in larger cohorts of patients and remains debated33,34. In a meta-analysis of available randomised trials including the RIVAL trial there was no significant difference in the rate of stroke between radial and femoral access (N=10,580, 0.4% radial vs. 0.4% femoral, OR 1.04; 95% CI: 0.57-1.89, p=0.90)6. Consequently, how arterial access sites influence this phenomenon remains uncertain and, as a cautionary measure, special attention should be paid during the phase of transition between femoral and radial access.
Procedure duration and time of catheter handling have been associated with an increased risk of both silent and symptomatic stroke, therefore special caution is required especially during the learning curve in setting up a transradial approach programme.
RADIATION EXPOSURE
There is some concern that transradial access is associated with increased radiation exposure for both patient and operator. Interpretation of data has been the subject of considerable debate35-37, with observational studies generally revealing a 25-50% increase in a variety of indirect measures of radiation exposure38. However, inexperienced radial operators are exposed to 40-50% more radiation than counterparts who are experienced, a difference that decreases rapidly with increasing experience38-40. In an extended meta-analysis of 23 randomised trials involving 7,020 patients, radial access was associated with significantly longer procedural and fluoroscopy times. However, significant heterogeneity was apparent, with larger differences in procedural times in studies performed by non-experts (4.8 minutes; 95% CI: 3.7-5.8 minutes) versus experts (1.7 minutes; 0.7-2.6 minutes, interaction p<0.001). In the randomised RIVAL trial6, longer fluoroscopy time was observed in patients who underwent radial access procedures, but the average proficiency of the radial teams was not optimal41. Indeed, a recent substudy from the RIVAL trial found that the difference in radiation dose between radial and femoral access was only present in lowest volume radial operators and centres.
Finally, a recent observational study showed that the right radial route was associated with a higher radiation exposure than the left radial approach, independent of the operator’s proficiency42.
Magnitude of radiation exposure in transradial procedures relative to femoral procedures is still unclear; however, it is highly influenced by operator experience. Specific attention to radiation exposure and protection is mandatory, whatever access site is used, and is critical during the learning phase, particularly when using the right radial approach.
EFFECTIVENESS
One meta-analysis and several observational studies have suggested that reducing vascular access-site complications and site-related major bleeds via radial access might improve patient outcomes20-22,43,44.
However, in randomised trials involving patients with both stable and acute coronary syndromes, femoral and radial access resulted in similar incidences of MACE after PCI (Figure 1).
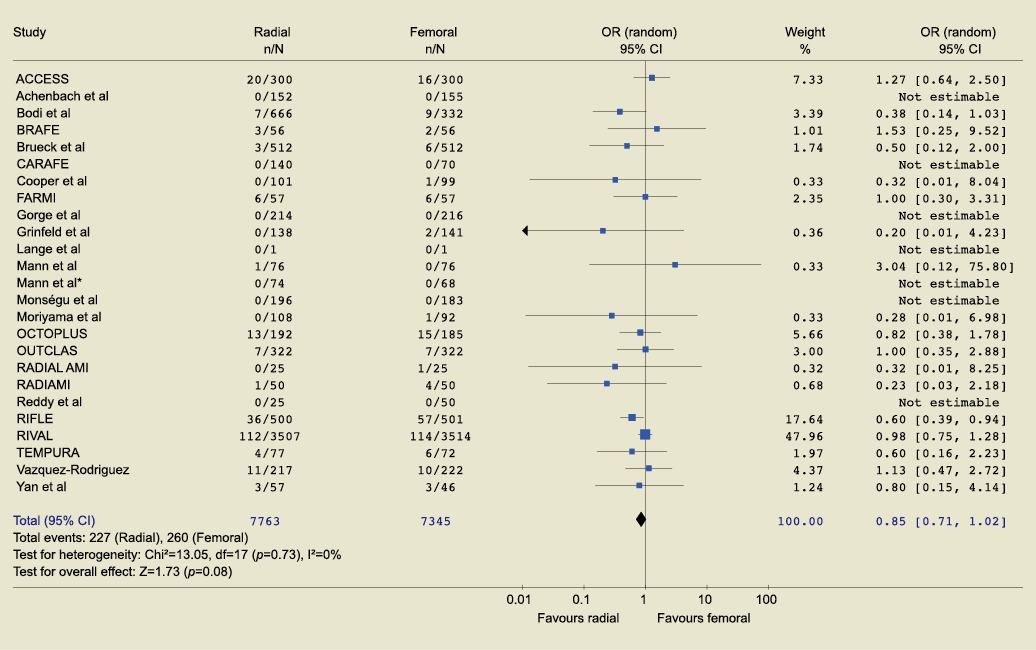
Figure 1. Forest plot depicting a meta-analysis of MACE in randomised studies comparing radial and femoral access for PCI.
Nonetheless, a recent large trial on 1,001 patients with STEMI (RIFLE study) reported statistically significant lower net adverse clinical events, NACE (composite of cardiac death, stroke, myocardial infarction, target lesion revascularisation and bleeding), and cardiac mortality in patients randomised to radial approach as compared to those randomised to femoral approach (NACE: 13.6% vs. 21%, p=0.003, respectively; cardiac mortality: 5.2% vs. 9.2%, p=0.020)7. Indeed, when looking only at STEMI patients in a comprehensive meta-analysis of randomised studies including RIFLE and RIVAL trials, radial access resulted in a statistically significant reduction in MACE relative to femoral access (OR 0.65; 95% CI: 0.49-0.87) (Figure 2).
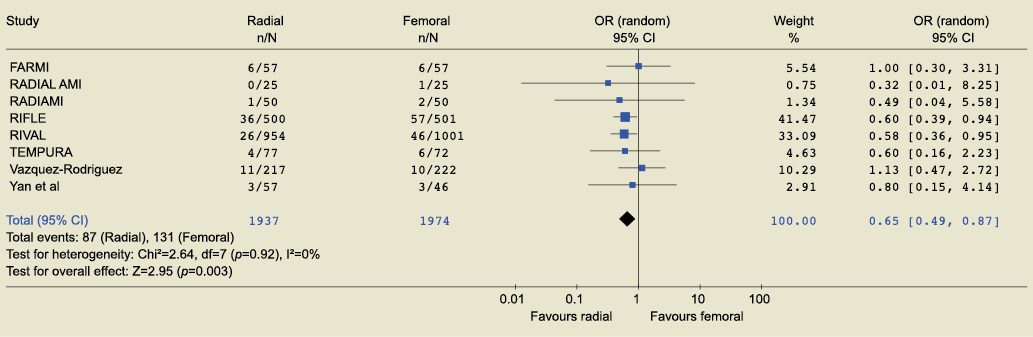
Figure 2. Forest plot depicting a meta-analysis of MACE in randomised studies comparing radial and femoral access for primary PCI.
This improvement appeared to be related to a statistically significant reduction in mortality via the radial versus femoral approach (OR: 0.56; 95% CI: 0.40 to 0.76) (Figure 3).
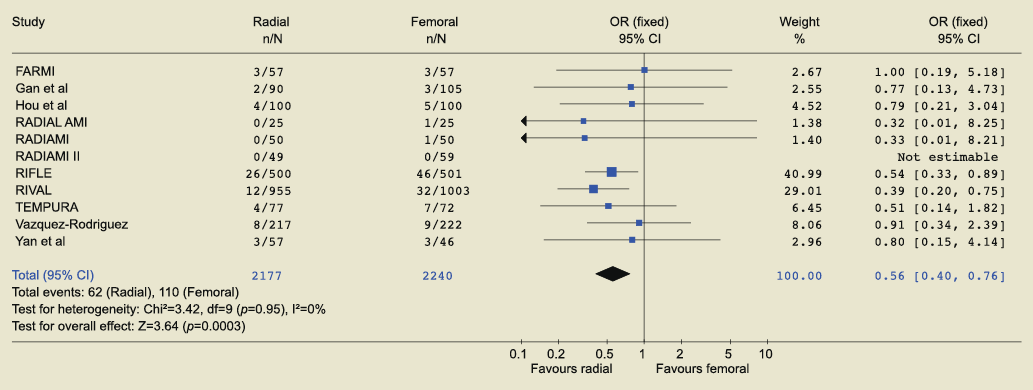
Figure 3. Forest plot depicting a meta-analysis of mortality in randomised studies comparing radial and femoral access for primary PCI.
In the recently published RIVAL trial, 7,021 patients with an acute coronary syndrome (non-ST or ST-elevation myocardial infarction) were randomly allocated to transfemoral or transradial access6. Interestingly, even though the radial and femoral approaches performed similarly with respect to primary and secondary outcomes, patients undergoing the procedure at centres with the highest tertile of radial approach volume and activity achieved statistically superior improvements (NACE HR 0.49, 0.28-0.87; p=0.015, interaction p=0.021; MACE HR 0.50, 0.27-0.92, p=0.027, interaction p=0.013).
TRI does not negatively affect the clinical effectiveness of PCI and, when performed by trained operators, provides better outcomes, including survival, by reducing vascular access site-related bleeding in STEMI patients.
HIGH-RISK SUBGROUPS
Special consideration is warranted for high-risk subsets. Patients undergoing PCI in the context of acute coronary syndromes are expected to receive a combination of multiple antithrombotic drugs that may lead to an increased risk of bleeding and subsequent morbidity and mortality. Radial access therefore appears attractive as a means to prevent such complications. In this clinical setting, radial access has been shown to be consistently associated, both in observational and randomised studies, with a reduction of vascular access site bleeding complications45-47 that could explain a reduction in death observed in adequately powered studies. In a cohort of 21,339 patients suffering from ST-elevation MI in the Swedish Coronary and Angioplasty Registry (SCAAR), the adjusted one-year cumulative risk of death was lower in patients treated via transradial access (OR 0.78, 0.64-0.96; p=0.018)48. In the RIVAL trial6, the combined primary endpoint of death, myocardial infarction, stroke and non-CABG related major bleeding at 30 days did not vary with site access. However, the rates of major vascular access-site complications and ACUITY non-CABG major bleeding (a post hoc definition) were higher in the transfemoral group. Conversely, access site crossover and fluoroscopy time were greater in the transradial group. On subgroup analysis, ST-elevation-related MI and centres with higher radial PCI volumes benefited significantly from the radial approach. Finally, recent meta-analysis of randomised controlled trials in STEMI patients confirmed a reduction in death associated with transradial access, supporting its preferential use for STEMI PCI49.
Women are at higher risk of bleeding and other adverse outcomes after PCI than men50,51. In a recent observational study, routine radial access was associated with reduced bleeding risk in women13. Unfortunately, muscular arterial hyper-reactivity, procedural discomfort and small artery diameter increased the risk of first-access failure (9.6% in women vs. 1.6% in men). It should be underlined that successful radial access does not entitle the operator to use more aggressive combinations of anticoagulants and antiplatelet agents in this group, given that women remain at higher non-access-site bleeding risk13,52.
Elderly patients are also at high risk for bleeding and vascular complications post PCI. Lower limb arteriopathy, tortuosity of the iliac arteries and aneurysms of the abdominal aorta may represent relative or absolute contraindications to femoral access. Because of peripheral artery disease in the elderly, radial access seems to be as feasible as femoral access53. In two randomised trials, the radial approach induced fewer vascular complications in elderly patients54,55.
Position statement on expertise requirements and development of a radial access programme
EXPERTISE REQUIREMENTS
OPERATOR AND VOLUME CENTRE ACTIVITY
The radial approach is a demanding technique, requiring expertise in both the operator and his/her team. Inability to puncture or cannulate the radial artery, inability to select the coronary artery and insufficient support to perform PCI is minimised by experience12. An operator’s annual procedure volume of more than 80 transradial cases correlates with a significant reduction in access failure, sheath insertion time and procedure time56. However, no threshold has been identified above which the volume of radial access procedures is no longer associated with enhanced success15. In the RIVAL study, the primary outcome was better with radial versus femoral procedures also at high-volume radial centres (median operator volume at these centres >146 radial PCI/year), again indicating the importance of experience of both operators and teams6.
To achieve the best results in TRI, individual operators and institutional teams should aim at maintaining the highest feasible rate of TRI. However, a reasonable objective for achieving an average satisfactory proficiency is aiming, after the learning curve has been completed, for over 50% radial access in routine practice with a minimum of 80 procedures/year per operator (including diagnostic and interventional procedures).
ROLE OF PARAMEDICAL STAFF IN THE CATHLAB AND POST-PROCEDURAL MANAGEMENT
Staff expertise is pivotal in the management of radial access, before the procedure, in the catheterisation laboratory and post-procedurally in the ward. Patient reassurance, adequate sedation, proper table preparation and correct selection and preparation of dedicated equipment are indispensable. Nurses also must be able to recognise rare but potentially serious complications that require prompt attention, such as delayed bleeding, that may occur at the level of the puncture site, in the forearm or remotely in the elbow, arm or axillary region. Early recognition is important to prevent compartment syndrome57. Nurses also must manage haemostasis in the hours following the procedure: gradual release of compression and early removal of the compressive bandage are key to preventing discomfort and permanent radial artery occlusion. Radial compression devices should be applied in a non-occlusive fashion by effectively stopping bleeding while leaving a residual flow in the compressed radial artery, which can assessed by plethysmography when manually stopping the flow in the ulnar artery. Compression pressure should then be released gradually, and total removal should occur within two hours56.
Nursing staff should be involved and become competent in radial approach management before, during and after the procedure. Early recognition of complications and haemostasis management are critical nursing responsibilities.
FEMORAL EXPERTISE
Promotion of a high volume of radial access may interfere with the equally important goal of maintaining proficiency in the femoral approach, which is indispensable in a variety of procedures, like intra-aortic counterpulsation and complex structural heart disease procedures, with some cerebral protection devices during carotid angioplasty as well as when radial access fails. As with the radial approach, outcomes depend on the experience of operators and centres. Several studies indicate that the most important determinant of complication prevention with femoral procedures is the overall organisation of hospitals and teams, as indicated by total laboratory volume, rather than the individual volume of operators59-63. Other studies have revealed relationships between outcomes and both laboratory and individual operator activity volumes64-68. Typically, a proficiency threshold has been set at >400 PCI procedures per year per catheterisation lab and >100 procedures per individual operator69.
All radial-proficient teams should aim to maintain optimal proficiency in femoral procedures as well. Some low-risk patients for femoral access site complications and procedures requiring femoral access (IABP, radial access failure or if guiding catheters ≥8 Fr are required) should provide a volume of cases to maintain adequate training in femoral artery puncture.
DEVELOPING A RADIAL ACCESS PROGRAMME
EQUIPMENT
Beyond the normal catheterisation laboratory equipment for femoral access, what is needed to start a radial access programme is minimal. A dedicated board connected to the cathlab table for the left and right arm should be available. The radial artery cannot be cannulated using the large needles used for femoral access. Some operators prefer to start with radial arterial cannulas normally used during general anaesthesia or in intensive care and gradually upsize to normal femoral sheaths; but most prefer to start with slightly more expensive commercially available radial access kits. Their progressive tapering and better lubricated coating facilitate insertion and reduce the risk of arterial spasm. Typical femoral catheters are completely compatible with radial access, but downsizing of the left Judkins to 3.5 for a normal aorta is advisable with the right radial approach. Also, additional dedicated radial shapes are available to allow for cannulation of both coronary ostia and even ventriculography with the same catheter, thereby avoiding the need for catheter exchanges, which are more cumbersome and potentially painful during radial procedures70. Changes of the catheter over-the-wire are indispensable to avoid repeated negotiations of tortuosities of the radial and brachial arteries or at the level of the subclavian/brachiocephalic trunk. A deep breath is very important to straighten subclavian tortuosities, reach the ascending aorta and facilitate catheter manipulation and intubation. Polymer-jacketed wires or even 0.014 inch angioplasty wires are required occasionally in the presence of radial or brachial loops. Their movement must be monitored constantly via fluoroscopy.
Minimal modification in the equipment is required to set up a transradial approach.
MANAGEMENT OF THE LEARNING CURVE
To start with, it is suggested that one use 5 Fr sheaths and catheters for diagnostic procedures and then move to 5 or 6 Fr for easy angioplasties. After the first 50 cases, the feasibility of radial and femoral access procedures should equalise71. At this stage, if no absolute contraindications exist, it is important to perform radial access in consecutive patients, at least for diagnostic procedures. Gradually, more complex procedures can be performed and, in selected patients, 7 Fr sheaths and catheters can be used. A stepwise approach to learning is proposed according to clinical characteristics, presentation and coronary stenosis characteristics. The highest level of competency is obtained when patients requiring complex clinical management can be managed with timely and technically proficient control of coronary interventions, irrespective of vascular access anatomy (Figure 4).
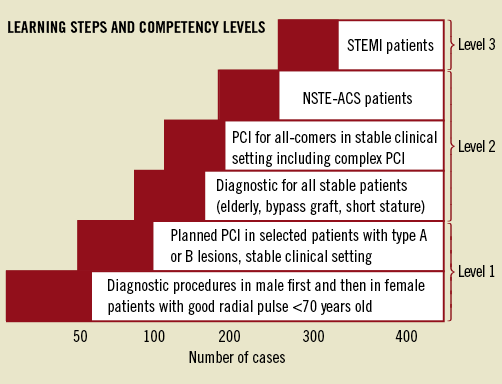
Figure 4. Proposed framework for learning steps and competency levels for TRI. ACS-PCI is proposed as the last step (NSTEMI and STEMI patients), due to expected anatomical variations and to less suitable clinical settings, where time constraints and/or complex pharmacological and clinical management are often required during the procedure.
It is essential to assess progress by monitoring procedural success rate, duration and X-ray doses.
DAY-CASE ANGIOGRAPHY AND ANGIOPLASTY
The immediate ambulation of the patient, safety of the entry site and, for PCI patients, reliable immediate outcome of an optimal coronary stent procedure, theoretically allow patients to be discharged from the hospital after a few hours of uneventful observation. Day-case angiography is already routine practice after femoral access, especially when closure devices are used. Of course, early discharge should not prevent the attending physician from discussing the results with the patient. A radial approach facilitates the process and avoids prolonged hospital stays. Because of the potential risk of bleeding after anticoagulation, day-case angioplasty is less frequently practised with the femoral approach, and is often limited to unstable patients transferred back to admitting hospitals. The first outpatient transradial coronary stent implantation was reported in 199472. Day-case angiography/PCI has several advantages73: patient preference, ease of ward management, shortened waiting lists, and enhanced cost-effectiveness. Overnight stay sometimes is prudent or required in selected groups meeting the following characteristics:
– Preprocedural: unstable angina pectoris, acute myocardial infarction, shock, heart failure, renal failure, severe comorbidities, poor social circumstances limiting family support after discharge.
– Procedural: transient vessel closure, arrhythmias or resuscitation during procedure, prolonged chest pain, persistent ECG changes, suboptimal PCI result, major or symptomatic side branch occlusion, entry site complication(s).
– Post-procedural: any cardiac or vascular complication within the 4-6 hour observation period.
If these criteria are applied consistently, outpatient PCI is safe74-76. However, these data stem from single-centre studies performed by expert operators at high-volume institutions. Therefore, at present, no definitive recommendations can be made based on published evidence; larger studies in the real world remain necessary to confirm the safety and efficacy of this technique.
Stable patients undergoing transradial diagnostic studies without complications in the first 2-3 hours post procedure can be considered for early discharge. Stable patients with an optimal PCI result, optimal pharmacological treatment according to ESC guidelines and no cardiac or vascular complications during the procedure or up to 4-6 hours afterwards can be considered for outpatient treatment if performed at high-volume centres by experienced interventionalists. Close follow-up and immediate readmission should be possible for delayed complications.
Technical recommendations
PATIENT SELECTION
All patients with palpable radial arteries can be considered for transradial access. However, as previously mentioned, while the conventional Allen test has almost been abandoned in routine practice because it is too subjective, more objective oxymetry or plethysmography assessment of the dual palmar arch circulation is recommended.
Transradial coronary access is contraindicated77 in patients with Raynaud’s phenomenon and those with a predictable mismatch between the radial artery and sheath/catheters required for treatment. Lymphoedema is a contraindication since local bleeding might have serious consequences. Also, patients with an AV fistula for renal dialysis should not have transradial access. Known variations in arm vasculature can be considered a relative contraindication. The final choice of procedure will depend on the level of expertise of the operator, and the equipment required. In patients with cardiogenic shock, transradial procedures can be performed if the radial artery is palpable while leaving two potential femoral accesses for intra-aortic balloon counterpulsation or more complex cardiac-assist devices.
RADIAL VS. ULNAR – LEFT VS. RIGHT
Choosing a right or left radial approach is determined by operator preference. Of course, if the right radial artery is inaccessible or left internal mammary must be cannulated selectively, a left-sided approach is preferred. In case of planned bypass with radial grafts, it might be more cautious to preserve the non-dominant radial artery. After the learning phase, left and right radial access procedures are effective and safe; though, in a recent meta-analysis of randomised studies, the crossover rate was higher with right-sided procedures76 and in an observational trial the left radial route was associated with shorter procedures and lower radiological exposure than the right radial approach, independent of operator proficiency40. The right side is usually more ergonomic to the operator; however, the left radial approach might be more convenient in the learning phase because of similar catheter handling when compared to the femoral approach.
Ulnar access has been reported feasible by several groups79-81; however, there are limited data on its safety in large series. Specific precautions should therefore be taken, and ulnar access should be attempted only after formal documentation of the patency of collateral hand circulation and, if performed, should be recorded in the patient’s medical records to allow the possibility of subsequent safe procedures from the radial arteries.
PRE-PROCEDURAL PREPARATION
The patient should be well informed about the different procedural steps, use of local anaesthesia and general intravenous sedation, site of puncture and sheath introduction, expected discomfort during sheath removal and post-procedural compression. Absence of pain as well as physical and mental relaxation should be pursued for all catheterisations, radial or femoral, but more intense sedation may be required with the radial approach, to minimise the risk of arterial spasm. Disinfection of the puncture site to the mid level of the forearm is performed with shaving limited to the wrist quadrant where the final bandage will be applied after compression. The arm must be positioned comfortably for both the patient and operator to ensure puncture success and allow for prolongation of the procedure, when necessary. Having the wrist stabilised and parallel with the table all through the procedure, with slight hyperextension at the time of the puncture, can facilitate access.
ANAESTHESIA, PUNCTURE, CANNULATION AND ADJUNCTIVE PHARMACOLOGICAL THERAPY
First, subcutaneous local anaesthesia is injected carefully using a short subcutaneous needle to minimise the risk of puncturing the radial artery, which is often more superficial than expected. Actual puncture of the radial artery is a critical step. The ideal site for puncture is 2-3 cm above the styloid process. If the puncture is too distal, sheath insertion is more difficult and can lead to perforation of the reticular ligament. The most frequently used techniques today are the bare needle and venous cannula techniques. Choosing between the cited techniques is operator-dependent, with neither technique clearly superior to the other.
After sheath insertion, various spasmolytic cocktails can be given, though this choice too is operator-dependent82. The most commonly used components are nitroglycerine and a calcium antagonist able to reduce the incidence of radial artery spasm to <5% with 6 Fr catheters and <1% with 5 Fr catheters82, while intra-arterial lidocaine should be avoided because it is a vasoconstrictive agent83. Proper heparinisation is important to prevent radial artery thrombosis (UFH 50 IU/Kg or 5000 IU in bolus)84.
ANATOMIC VARIATIONS AND VASCULATURE NAVIGATION VIA THE RADIAL APPROACH
Challenging anatomy must be avoided to minimise the risk of complications and shorten the duration of both the procedure and radiation exposure. For this reason, a systematic preliminary angiogram of the arteries of the forearm through the introducer inserted into the radial artery for two to three cm has been suggested by some authors84.
Different classifications of anatomical variation have been proposed85-87; however, three major anatomical variations –high radial artery bifurcation, loops and tortuosities– generate most procedural failures. High radial artery take-off or bifurcation is frequent. With traditional, type 3 high radial take-off (Figure 5), a remnant radial or slender hypoplasic radial artery exists such that the radial artery diameter may be too small even for 4 Fr catheters. An alternative approach is preferable in this extreme case, because progressing otherwise is painful and associated with spasm and an increased risk of perforation. Contralateral radial access is always a possibility to be considered in this setting, because forearm vasculature tends to be asymmetrical88. Alternatively, conventional femoral access can be used. Angiographic assessment of the radio-ulnar anastomosis at the elbow is mandatory in these cases, because an angiographically-negotiable anastomosis between the radial and ulnar arteries often exists (Figure 6); crossing this anastomosis allows the operator to reach the brachial artery directly.
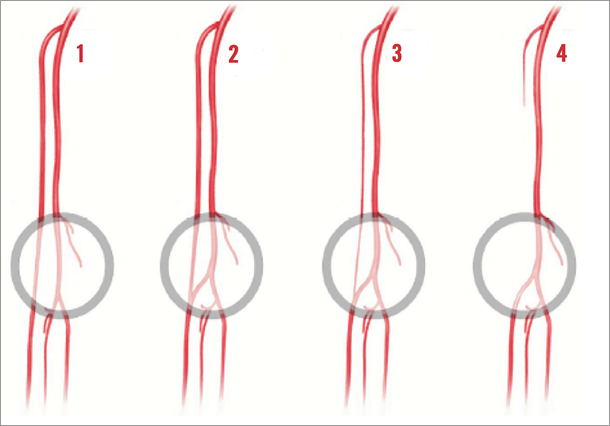
Figure 5. High take-off of the radial artery (high bifurcation). Type 3 is associated with radial access failure. With this variation, the small-diameter remnant radial artery cannot be catheterised and is very prone to spasm.
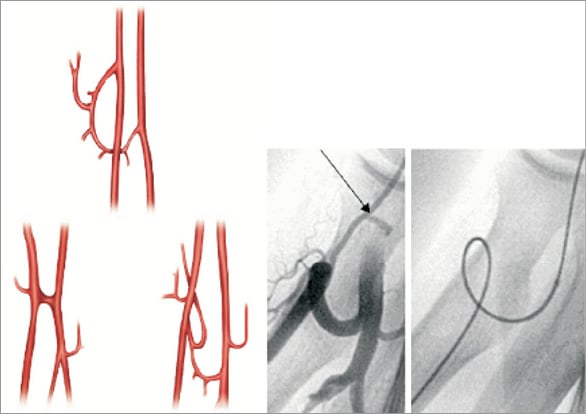
Figure 6. Radio-ulnar anastomoses that can be described require evaluation in cases of high radial artery take-off when the radial artery is slender. In this example, as shown in the angiograms (right side), the large vessel loop connecting the radial and ulnar arteries has been crossed successfully.
Resistance to wire progression can be caused by tortuosities at different levels: the radial artery, the brachial artery before the subclavian artery and the brachiocephalic trunk. These tortuosities are more common in older patients and in patients with a long history of hypertension, and plastic polymer-coated wires or PCI wires can be useful89. A special note of caution is appropriate, especially when the right transradial approach is used, due to the risk of stroke. Systematic fluoroscopy is required for crossing the subclavian artery and the brachiocephalic trunk to avoid penetration of the right carotid, vertebral arteries or a distal taking off mammary artery. During attempts to reach the ascending aorta, the patient should take and hold a deep breath, thereby facilitating the correct orientation and placement of the catheter in the ascending aorta.
Finally, a retro-oesophageal right subclavian artery (arteria lusoria, taking off at the distal part of the horizontal aorta or directly connected to the descending aorta) is rare (0.25%) and, although technically negotiable for both diagnostic studies and PCI90, it invariably requires unnecessary longer radiation exposures. Therefore a rapid diagnosis and conversion to an alternative arterial approach are strongly advised.
Operators should expect anatomical variations and have a plan to overcome them. In the vast majority of cases, caution advancing wires and catheters, angiographic assessment and using specific wires will yield a successful transradial intervention. In cases of high take-off of the radial artery associated with a remnant or slender radial artery, an alternative approach, like femoral or contralateral radial access, is preferable to avoid unnecessary prolongation of the procedure.
CATHETER CHOICE AND HANDLING
Even if dedicated catheter shapes are available, traditional femoral shapes accommodate the radial approach easily. Coaxial alignment with the target coronary artery is mandatory and requires different handling for the right radial versus femoral approach. In some procedures, a single appropriately-shaped diagnostic catheter can be used for angiography of both coronary arteries, potentially decreasing arterial trauma due to catheter exchange as well as procedure duration and costs, with satisfactory angiographic quality. On the other hand, caveats must be acknowledged, like the increased risk of non-coaxial cannulation and associated risk of ostial dissection. Several options can be considered, including femoral multipurpose, Sones type II and Amplatz left or specifically dedicated curves for radial access; however, their use remains a matter of individual preference. Judkins left 3.5 for left coronary and Judkins right 4 or Amplatz left and right 1, 2 are preferred for RCA with a normal-sized aorta.
For PCI, the choice of guiding catheter (diameter, shape, size) is pivotal for adequate back-up. However, this need should be balanced against the correlation between radial artery occlusion rate and the diameter of sheaths and catheters. To minimise radial and coronary artery injury as well as to optimise back-up, 5 Fr large-lumen guiding catheters can be used (active back-up with deep insertion into coronary arteries, when needed). Large-lumen, 6 Fr guiding catheters allow most PCI to be performed, including complex cases, bifurcations with most techniques (excluding simultaneous use of two stents), rotablator use (up to a 1.75 mm burr), thrombus aspiration and distal protection. In selected patients of large stature, larger catheters (7 or even 8 Fr) or sheathless guiding catheters can be considered, allowing for large-lumen guiding catheters to be used in a small radial artery. However, these catheters, though useful in selected cases, are more difficult to handle in complex procedures because of low back-up.
Coronary artery bypass graft angiography and PCI can be achieved successfully by radial access with standard catheters. Both saphenous vein and arterial grafts can be managed, but with single left internal mammary arteries a left-sided approach is warranted. Native double mammary grafts also can be managed by double radial access, while single radial access (preferably right) –especially in inexperienced hands– is more demanding in terms of catheter handling and subsequent procedural duration, with associated risks of increased radiation exposure, vascular complications and stroke.
PERIPHERAL INTERVENTIONS
Lesions of the supra-aortic arterial trunks also can be accessed radially. Radial approach for carotid artery interventions are recommended when femoral access is difficult and in demanding anatomic conditions91,92 (e.g., severe tortuosities, bovine aortic arches or displaced transition of the origins of supra-aortic vessels due to severe atherosclerosis). The brachiocephalic trunk, left subclavian and vertebral arteries can be accessed easily91,93,94.
One limitation of the radial approach is the need for larger-diameter sheaths (e.g., cerebral protection devices or larger-diameter stents) although up to 8 Fr sheaths can be accommodated at the possible cost of increased late radial occlusion rate95,96; in this setting, assessing the diameter of the radial arteries beforehand aids in the selection of suitable cases.
The radial approach is ideal for renal interventions because of the cranio-caudal course of renal arteries after their origin in the aorta, especially in cases of calcified renal or iliac vessels with marked iliac tortuosity97-101. Technically, the left radial approach should be preferred because of the shorter length and reduced need for catheter manipulation. Longer guiding catheters (120 cm) are available.
Mesenteric and celiac angioplasty are also feasible via the radial route99,102,103, while aorto-iliac and iliac lesions are associated with lower complication rates via transradial access104. In cases of absent femoral pulses, severe bilateral iliac artery disease, obesity or conditions prohibiting prolonged supine rest, the proximal superficial femoral artery also can be treated via radial access with very long guiding catheters (>120 cm)105,106.
Radial access in peripheral interventions appears safe and feasible in carefully selected cases and is likely to carry the same reduction in access-site complications as in coronary interventions. However, developing new access-site specific equipment is strongly encouraged to maximise applicability, feasibility and outcomes.
CHRONIC TOTAL OCCLUSIONS (CTO)
Treatment of chronic total occlusions requires a bilateral injection in all patients with good collaterals from a contralateral artery (50-60% of cases)107. A transradial approach is appealing to reduce the bleeding risk consequent to the double arterial instrumentation with prolonged deep anticoagulation. However, many CTO-specific techniques and dedicated devices are difficult to use via 6 Fr catheters. An over-the-wire approach is mandatory in CTO recanalisation and 6 Fr catheters only accept thin OTW microcatheters such as the FineCross™ (Terumo, Tokyo, Japan) which can be inserted together with a second monorail balloon (anchoring, trapping technique) or a second microcatheter (parallel wire technique). If OTW balloons or the Corsair microcatheter (ASAHI INTECC Co., Ltd., Aichi, Japan) are used they can only be used in isolation via a 6 Fr guide. Stability of the guide catheter and positional changes due to patient movements and breathing in procedures that may last hours are other potential concerns, together with the greater risk of radial artery occlusion maintaining 6 or 7 Fr sheaths in situ for hours. Still, innovative operators have developed approaches based on active intra-arterial engagement as well as simplified materials and techniques that are successful in many cases, with relatively simple CTOs. Experienced CTO operators should be familiar with transradial recanalisation also using complex approaches including retrograde for patients with difficult or unusable femoral routes.
COMPLICATIONS: PREVENTION AND MANAGEMENT
Relative to femoral procedures, radial access has reduced vascular access-related complications in both randomised and observational studies. Rare complications are often easily prevented or managed. Radial artery occlusion is the most common complication, affecting 1.5% to 33% shortly after the procedure56,108-111. The true incidence could be underestimated because it is asymptomatic in the vast majority of cases. Critical ischaemia with necrosis has never been reported after a thorough evaluation of palmar vasculature patency via oxymetry; however, critical hand ischaemia requiring surgery has been described because of distal embolisation112. Moreover, occlusion of any radial artery may limit further radial access, though re-access of occluded radial arteries is feasible in selected cases. Therefore, a systematic assessment of radial artery patency after the procedure is strongly recommended. Lower body weight, lower systolic blood pressure at haemostasis and the presence of local haematoma and discomfort after the procedure are more frequent findings in radial occlusion108. To prevent occlusion, anticoagulation is necessary during the procedure with intravenous unfractionated heparin (UH)56 or other more costly anticoagulant strategies113-116. Better patency rates are obtained using smaller catheters115 and careful radial haemostasis techniques, with non-occlusive radial artery compression ideally removed within two hours58,118,119. Once radial occlusion is diagnosed, up to 50% resolve spontaneously within one month119, though increased radial artery patency can be obtained with immediate homolateral one-hour occlusion of the ulnar artery120 and/or low molecular weight heparin administration for four weeks after the procedure121. Finally, successful recanalisation of occluded radial arteries by angioplasty has been reported, but cannot be recommended at the present time122-124.
According to different definitions, radial artery spasm incidence varies widely and may imply clinical consequences (such as catheter entrapment, severe pain, resistance to manipulation of catheters) from 2-22% of patients15,125,126. Spasm is the second most common cause of radial access failure after anatomical variations15. Predictors of spasm are: older age, short stature with small radial artery diameter, female gender, diabetes, failed first arterial access and pain127-129. Spasm can be prevented and/or treated with proper local anaesthesia, hydrophilic arterial sheaths and/or hydrophilic catheters, gentle and balanced movement of catheters, avoidance of cold intra-arterial injections and robust premedication to limit patient anxiety. Several strategies have been proposed to overcome radial spasm including intra-arterial drugs (both singly as well as in combination)80, and using hydrophilic coatings15,126 or dedicated sheaths with a very tapered dilator, thereby avoiding injury induced by the sharp edge of the catheter protruding from the guidewire. The systematic preventative use of spasmolytic drugs is recommended.
The radial approach is effective at reducing haemorrhage; however, interventionalists must keep in mind that only access site-related bleeding can be reduced via radial access. Whatever the access site used, ESC recommendations for antithrombotic strategies must be applied, particularly among ACS patients. Local bleeds usually do not require treatment; but, in very rare instances, a dramatic forearm compartment syndrome may arise after arterial perforation130. Prompt recognition of limb swelling is imperative, while symptoms of motor and sensibility impairment may occur later when permanent neurological damage may already be present. Usually one or two 15-minute local inflations of a sphygmomanometer cuff compressing the perforation site to preserve radial artery patency are sufficient; it is rare that urgent surgical decompression may be required131.
Arteriovenous fistulas and radial pseudoaneurysms occur in 0.2-0.4% of cases6,9. They might be associated with higher doses of anticoagulants or GPI use during the procedure and can usually be treated conservatively.
Anecdotal cases of radial artery eversion or damage as well as sterile granulomas after sheath removal have been described. Another very rare complication is radial nerve injury, caused either by the procedure itself or by aggressive haemostasis via prolonged radial artery compression leading to different grades of causalgia130.
Infrequent and sometimes anecdotal complications have been associated with radial access. Radial occlusion should be prevented during and after the procedure and a systematic assessment of arterial patency performed. Spasm prevention is recommended routinely. Specific early and delayed post-procedural attention to forearm haematomas is a must.
COST-EFFECTIVENESS
While no systematic studies have been published on the cost savings associated with TRI, common sense suggests that significant savings can be achieved by adopting single-day angiography and angioplasty. The earliest study on the cost-effectiveness of transradial versus transfemoral coronary stenting demonstrated significantly reduced hospital stays and costs associated with the diagnostic and therapeutic management (surgery, transfusions) of entry site complications4. In one meta-analysis20, length of stay declined 0.5 days with radial access; and data from the MORTAL Registry (n=32,822) identified a 50% reduction in transfusions22. Reduced access site bleeding could significantly reduce costs associated with closure devices, bleeding complications and transfusions that would be incurred with femoral access. Some studies have shown reductions between $184 and $191 in equipment and supply costs for angiography with radial versus femoral access plus a closure device133-135.
TRI AND PATIENT PREFERENCE
From a patient perspective, radial access offers significantly less discomfort and significantly improved quality of life as compared to femoral access. Patients who have experienced both access routes strongly prefer radial access, primarily explained by their ability to mobilise immediately after the procedure. Patients in the RIVAL trial when asked what approach they would like for a subsequent procedure much more commonly preferred radial6. Cooper et al noted reduced back pain (p<0.0001), reduced difficulty walking (p<0.0005) and improved social functioning and mental health (p<0.01) with radial access136. More recent publications have shown that radial access is associated with reduced procedural discomfort and that TRI is more acceptable than femoral access amongst elderly patients. Never subjected to research, but commonly cited, the “discreteness” of the puncture site far from the pubic area also contributes to patient preference.
Conflict of interest statement
F. Kiemeneij receives Kimny catheter sales royalties from Boston Scientific. The other authors have no conflicts of interest to declare.

