Abstract
Aims: This study aimed to compare outcomes in unselected patients undergoing cardiac catheterisation via transradial versus transfemoral access and standard versus ultrasound-guided arterial access.
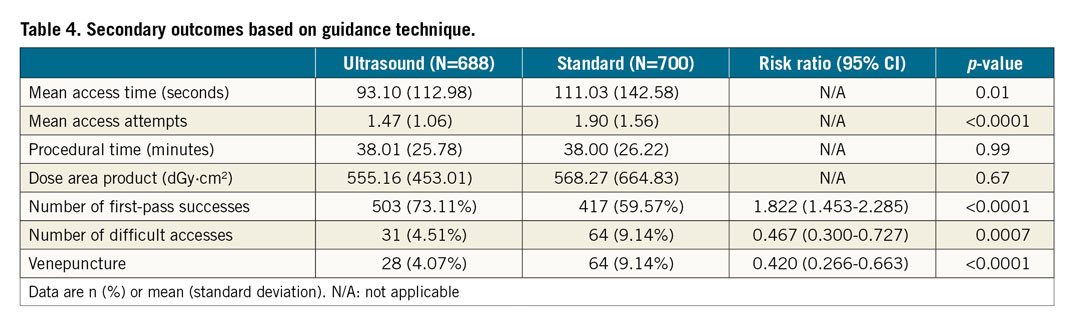
Methods and results: This was a prospective, randomised (radial vs. femoral and standard vs. ultrasound), 2x2 factorial trial of 1,388 patients undergoing coronary angiography and percutaneous coronary intervention. The primary outcome was a composite of ACUITY (Acute Catheterization and Urgent Intervention Triage strategY) major bleeding, MACE (death, stroke, myocardial infarction or urgent target lesion revascularisation) and vascular complications at 30 days. Transradial access reduced the primary outcome (RR 0.37, 95% CI: 0.17-0.81; p=0.013), mostly driven by ACUITY major bleeding (RR 0.343, 95% CI: 0.123-0.959; p=0.041) when compared with the transfemoral approach. There was no difference in the primary outcome between standard and ultrasound guidance (p=0.76). Ultrasound guidance, however, reduced mean access time (93 sec vs. 111 sec; p=0.009), attempts (1.47 vs. 1.9; p<0.0001), difficult accesses (4.5% vs. 9.2%; p=0.0007), venepuncture (4.1% vs. 9.2%; p<0.0001) and improved first-pass success (73% vs. 59.7%; p<0.0001).
Conclusions: Transradial access significantly reduced the composite outcome compared to transfemoral access. Ultrasound guidance did not reduce the primary outcome compared to the standard technique, but significantly improved the efficiency and overall success rate of arterial access.
Introduction
Despite continual improvements in pharmacological and technical measures, bleeding complications still remain a major concern in patients undergoing invasive coronary interventions. A significant number of these arise from the access site1,2. Major bleeding has been associated with recurrent ischaemia and increased in-hospital and one-year mortality3,4. A number of registries5,6 and recent studies7,8 have shown that transradial access reduces vascular complications, major bleeding and all-cause mortality compared with transfemoral access in acute coronary syndrome (ACS) patients undergoing coronary angiography (CA) and percutaneous coronary intervention (PCI). However, only a small number of randomised trials exist comparing access sites in non-ACS coronary investigations9,10.
Furthermore, ultrasound guidance in facilitating arterial access may reduce vascular complications and possible bleeding. It is routinely used when inserting central venous catheters. Multiple randomised trials have demonstrated significant reductions in complications, failure rates, and time accessing central veins when real-time ultrasound (US) guidance is used11,12. There are limited trials assessing real-time US guidance for coronary angiography. To date, only two large randomised trials have examined US guidance for femoral and radial arterial access13,14. Both showed higher success rates in vascular access; however, reduced vascular complications were only demonstrated in the femoral study comparing US versus fluoroscopic guidance.
Therefore, we performed a randomised trial assessing the value of real-time US guidance compared with standard (SD) palpation technique, in both transradial (TRA) and transfemoral access (TFA), on unselected patients, with or without ACS, referred for CA and PCI.
Methods
STUDY DESIGN AND PARTICIPANTS
The Standard versus Ultrasound-guided Radial and Femoral access (SURF) trial was a prospective, investigator-initiated, single-centre, randomised, single-blinded, 2x2 factorial trial. All-comer, consecutive patients 18 years or older referred for CA and PCI were consented for enrolment in the trial conducted according to the CONSORT guidelines (Supplementary Appendix 1). The participating cardiology trainees, fellows and interventional cardiologists were competent, dual-trained in both radial and femoral access, and in using US guidance. All operators had performed at least 75 coronary interventions in the previous year, a minimum of 50 standard TRA and TFA, and 10 proctored US-guided access for both the radial and the femoral artery. All who satisfied the required training numbers were certified before taking part in the trial. For SD femoral access patients, fluoroscopy using a radiopaque marker prior to the procedure was undertaken at the discretion of the operator. A single L25x/13-6 MHz, linear-array transducer (Fujifilm SonoSite, Bothell, WA, USA) was used for both TRA and TFA US guidance. All US guidance was performed freehand without a needle guide.
Ineligible patients were those in cardiogenic shock, those on dialysis, and those who had known severe peripheral vascular disease, previous failed access, or a failed Allen’s test. The trial was undertaken at a large metropolitan tertiary hospital and approved by the local ethics committee (reference number HREC/11/LPOOL/55). All patients gave written informed consent. An independent clinical events committee masked to treatment allocation adjudicated all suspected outcome events.
RANDOMISATION AND MASKING
Patients were randomised (1:1) to radial or femoral access, and (1:1) to either standard or US guidance. Sealed envelopes balanced in blocks of 50 were used for randomisation. Patients and investigators were not masked to access allocation.
ENDPOINTS
The primary endpoint was the composite of ACUITY (Acute Catheterization and Urgent Intervention Triage strategY)15 major bleeding, major adverse cardiovascular events (MACE) comprising death, stroke, myocardial infarction or urgent target lesion revascularisation, and vascular complications at 30 days. The secondary endpoints were access time, number of attempts, venepuncture, difficult accesses and first-pass success. All patients were followed up at one week and one month.
ENDPOINT DEFINITIONS
Access time was recorded from when the local anaesthetic needle first touched the skin until the sheath was successfully inserted, excluding set-up and fluoroscopic imaging time. Attempts were defined as forward motion of the needle separated by any withdrawal. Difficult accesses were those requiring five or more attempts. All were recorded by an independent observer.
STATISTICAL ANALYSIS
At the time of the trial design, a minimum total sample size of 1,388 was calculated in order to detect a 25% relative risk reduction between group vascular complication rates in Factor 1 (TRA vs. TFA) and Factor 2 (SD vs. US), with a significance level of 2.5%, using a two-tailed F-test, accounting for a 10% loss to follow-up. All patients were included in the intention-to-treat analyses. Logistic regression was used to compare the composite outcome between TRA versus TFA, and standard versus US guidance with a rate ratio and 95% confidence interval reported. Pre-specified subgroup analyses based on age, body mass index (BMI), gender, diabetes, operator experience, indication and procedure type were performed. Kaplan-Meier cumulative hazard curves were constructed for the primary endpoint of ACUITY major bleeding, MACE and vascular complications with log-rank testing for significance between strata. A two-tailed p-value of <0.05 was used for significance. Analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA) and Stata v12 (StataCorp, College Station, TX, USA).
Results
BASELINE CHARACTERISTICS AND PROCEDURAL DATA
Between November 2012 and November 2017, 2,440 consecutive patients referred to the cardiac catheter laboratories were screened and 1,388 patients were enrolled, among whom 688 and 700 were randomised to TFA and TRA, respectively. Non-enrolment reasons included inability to provide informed consent, patient’s preference for TRA and operator’s preference for TRA due to favourable evidence in ACS patients. In the TFA group, 357 patients were randomised to the SD technique and 331 were randomised to US guidance. Similarly, in the TRA group, 343 and 357 patients were randomised to SD and US guidance, respectively (Figure 1). Loss to follow-up was similar between the TFA and TRA groups (3.8% vs. 3%), but crossover rates were higher in the TRA (7.7%) compared with the TFA (1.6%) group. This higher rate of crossover was observed in both the SD (8.2%) and US guidance (7.3%) subgroups of the TRA arm, although it was mostly in the SD TFA subgroup (SD TFA 2.5% vs. US TFA 0.6%). Reasons for crossover in the TRA group were radial artery spasm (51.9%), converting to US guidance for arterial localisation (33.3%) and subclavian tortuosity (14.8%). In the TFA group, conversion to US guidance occurred to locate the artery (81.8%), dissection (9.1%) and failure to pass the wire (9.1%). The overall demographic and baseline characteristics were well balanced between the TRA and TFA, as well as between the SD and US guidance groups (Table 1). Of the 1,388 patients included, 591 had unstable angina, 388 had NSTE-ACS and 61 had STEMI. The majority of patients were male, Caucasian with BMI ≥25 kg/m2 and had a history of smoking, hypertension and hypercholesterolaemia. Two patients in the US TRA group had thrombolysis prior to PCI.
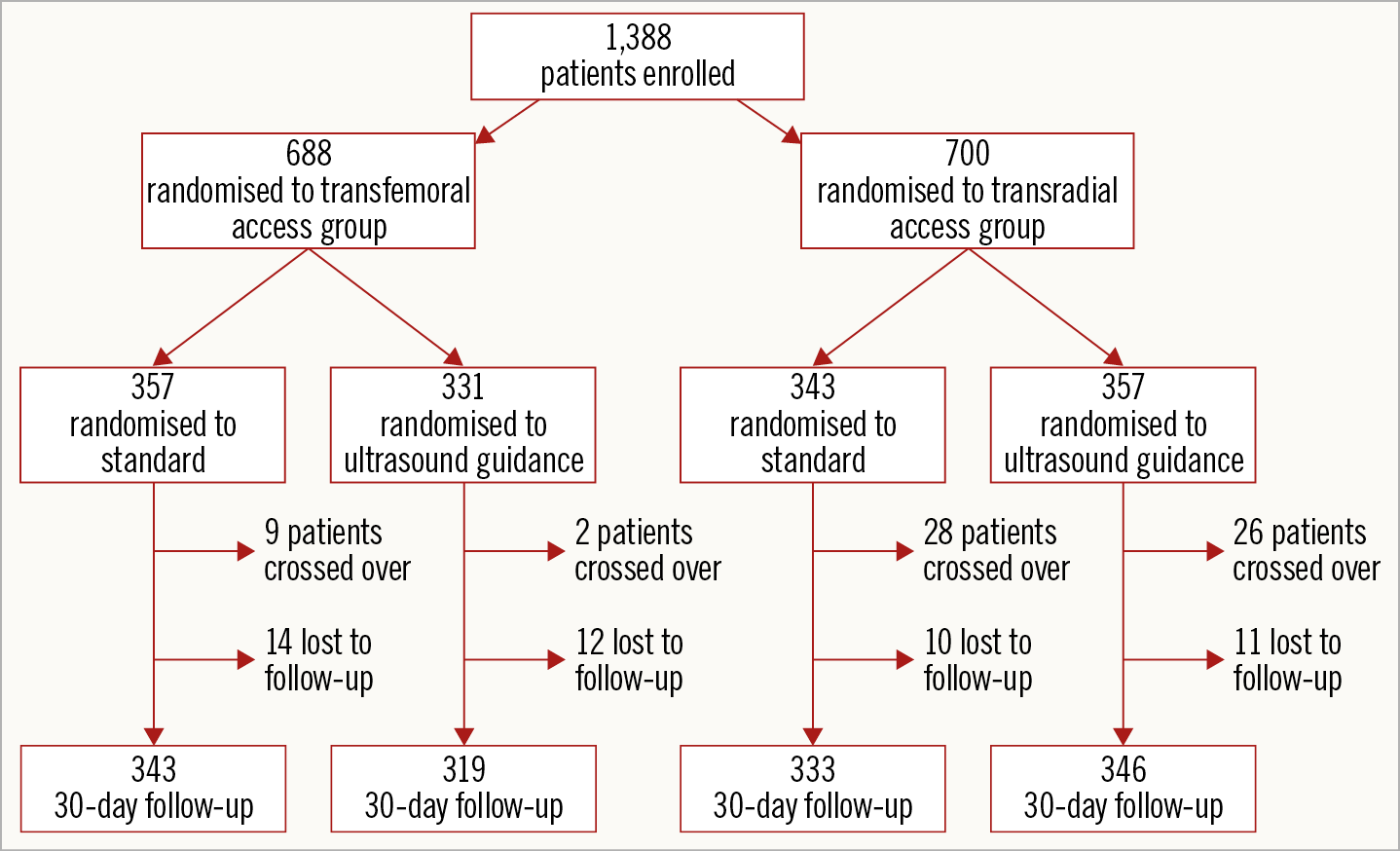
Figure 1. Flow chart of the study.
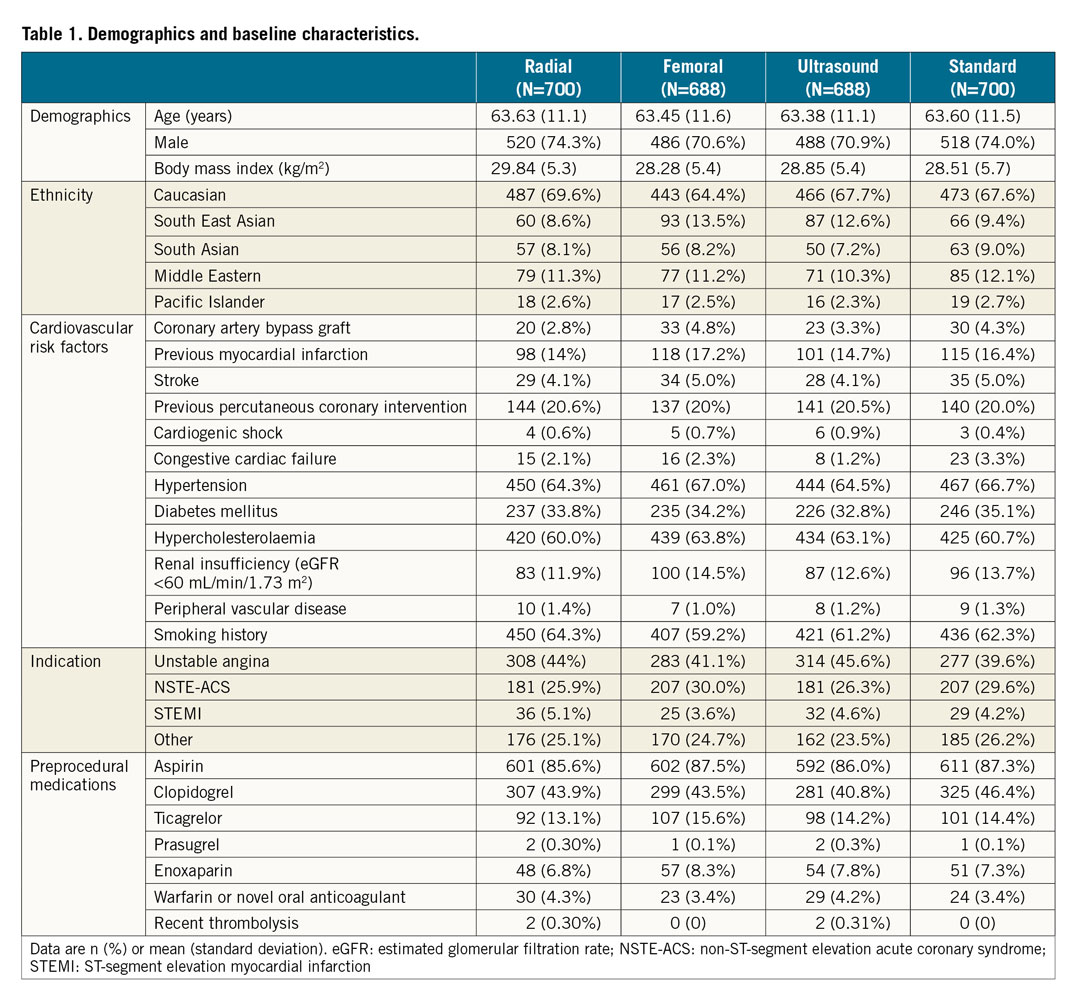
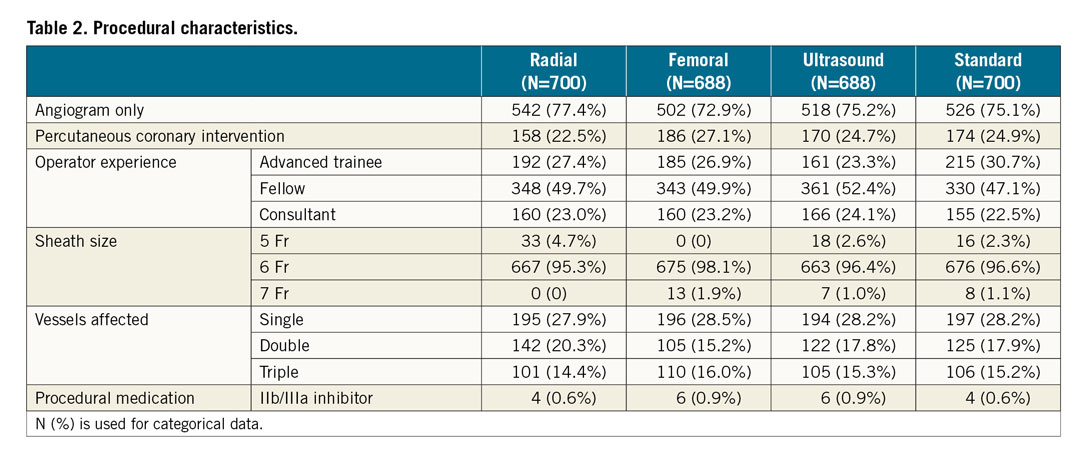
The procedural characteristics were similar among the groups (Table 2). Most patients had diagnostic coronary angiography only. The majority of cases were carried out by cardiology fellows, followed by advanced trainees and consultants. Less than 1% of patients received glycoprotein IIb/IIIa inhibitors. The TR Band (Terumo Corp., Tokyo, Japan) without ulnar artery compression was used for all TRA. The only closure device used for TFA was the Angio-Seal™ VIP (Terumo Corp.) and the usage rate was similar between femoral US and femoral SD groups (40.2% vs. 35.6%).
CLINICAL OUTCOMES
The primary composite outcome of ACUITY major bleeding, MACE and vascular complications at 30 days occurred in 1.3% and 3.5% of the TRA and TFA groups, respectively (p=0.013) (Figure 2, Figure 3). In the subgroup analysis, there was no significant difference between TRA and TFA based on patients’ age, indication or operator experience, but the results were numerically superior with consultant experience. The TRA group had a reduced composite endpoint in females (1.1% vs. 5.1%; HR 0.21, 95% CI: 0.046-0.979; p=0.047), diabetics (0.4% vs. 4.3%; HR 0.098, 95% CI: 0.012-0.77; p=0.027) and patients with BMI ≥25 kg/m2 (0.8% vs. 3.4%; HR 0.22, 95% CI: 0.073-0.664; p=0.007). There was no difference between the US guidance and SD groups in the primary composite outcome at 30 days (Figure 3, Figure 4). The overall event rates were 2.3% in the US group versus 2.5% in the SD group (p=0.756). No difference in the composite outcome between groups was noted in the subgroup analyses.
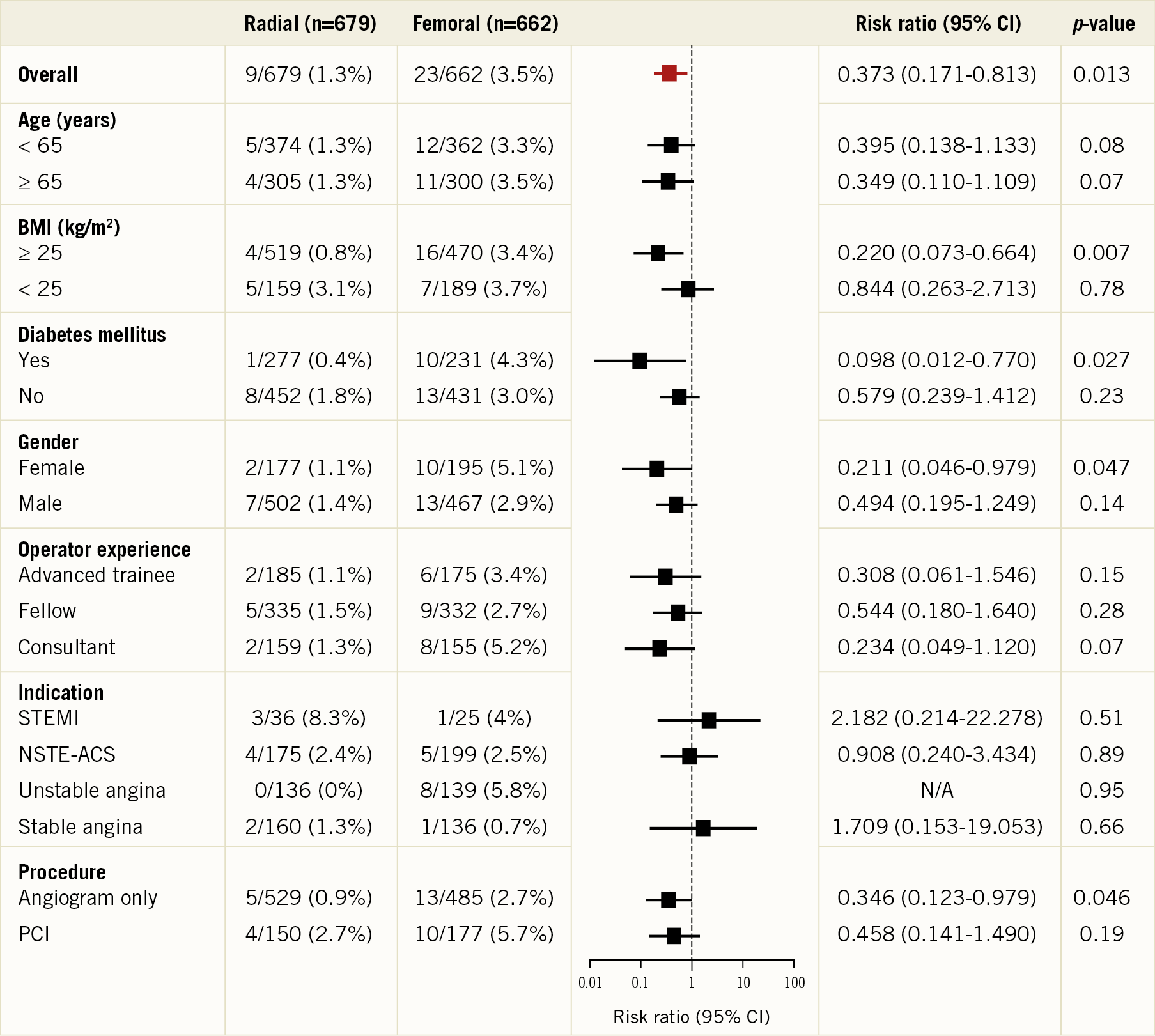
Figure 2. Primary composite outcomes based on access site. Numbers in each subgroup may not equal the total because of incomplete data in some patients. BMI: body mass index; CI: confidence interval; NSTE-ACS: non-ST-segment elevation acute coronary syndrome; PCI: percutaneous coronary intervention; STEMI: ST-segment elevation myocardial infarction
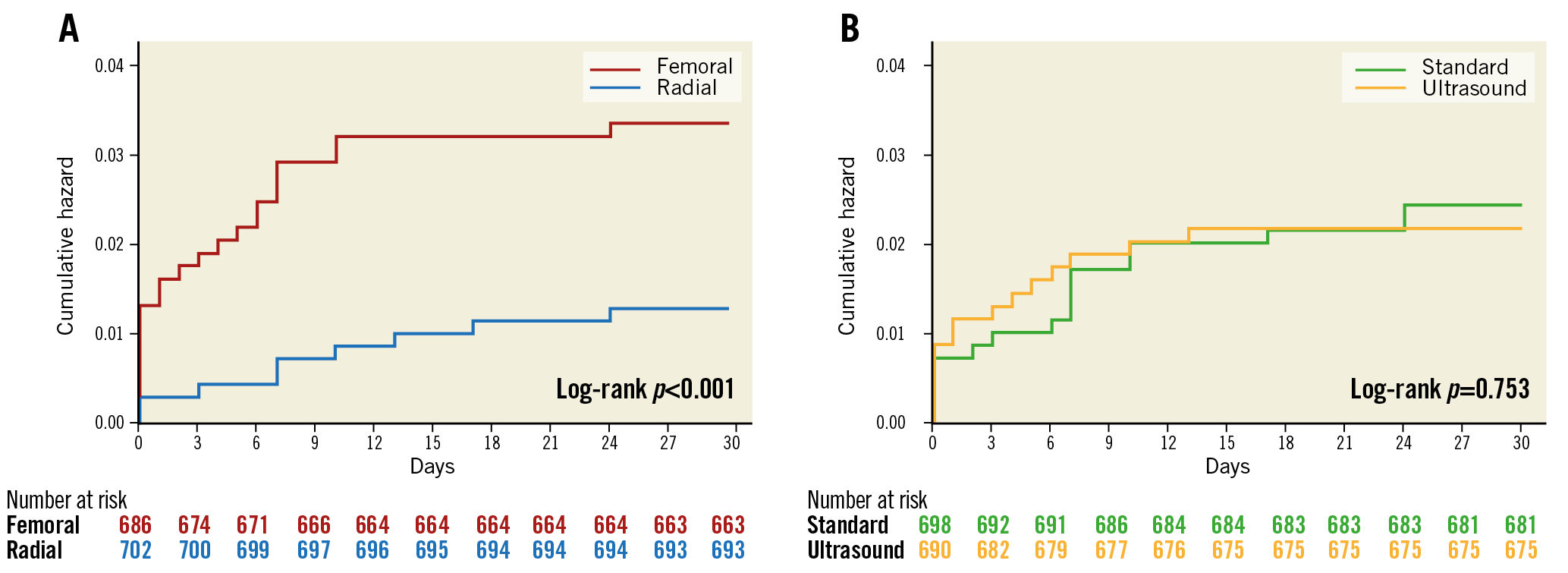
Figure 3. Kaplan-Meier event curves for the primary outcome. A) Radial vs. femoral access. B) Standard vs. ultrasound-guided access.
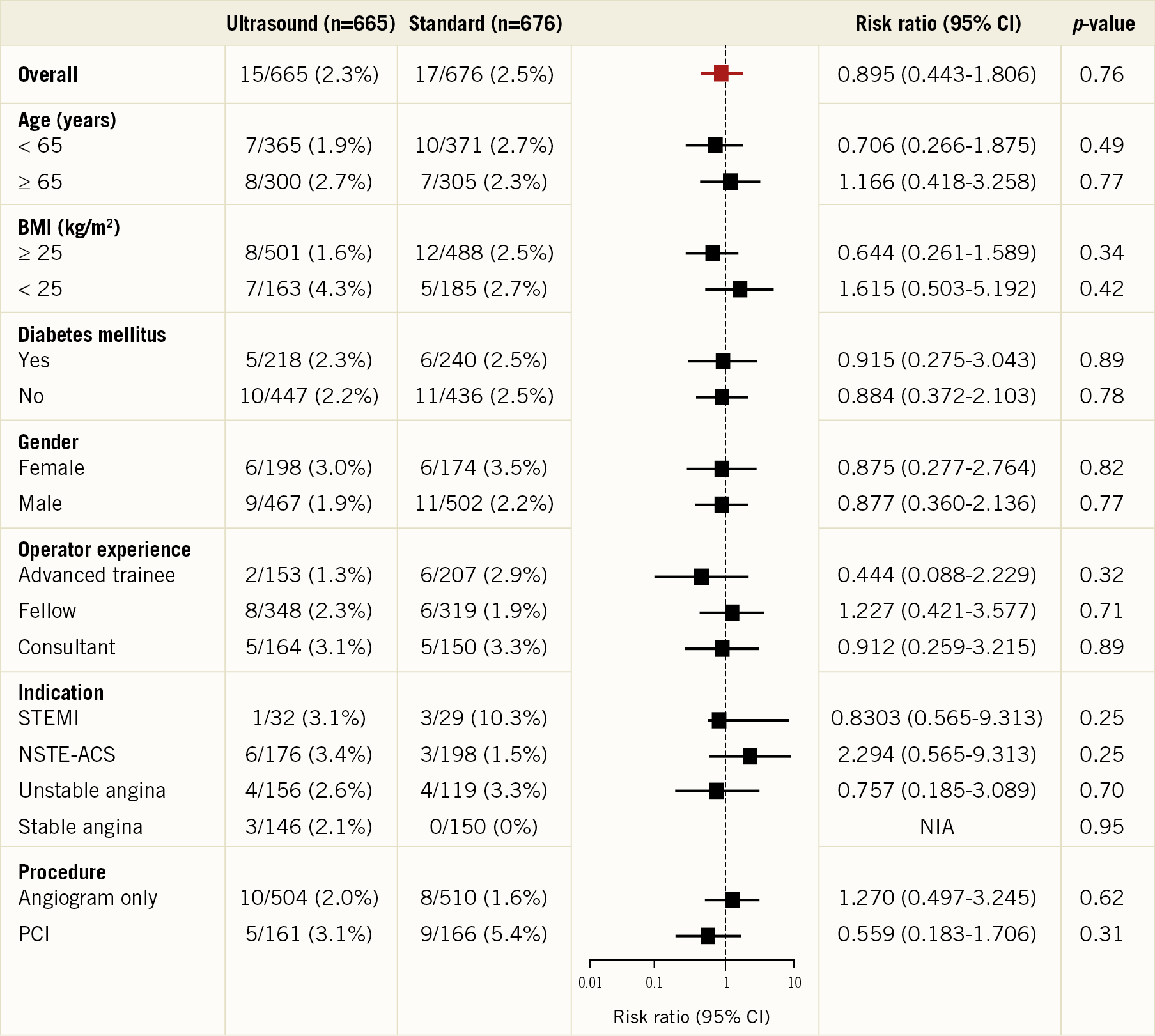
Figure 4. Primary composite outcomes based on guidance technique. Numbers in each subgroup may not equal the total because of incomplete data in some patients. BMI: body mass index; CI: confidence interval; NSTE-ACS: non-ST-segment elevation acute coronary syndrome; PCI: percutaneous coronary intervention; STEMI: ST-segment elevation myocardial infarction
INTRAPROCEDURAL OUTCOMES
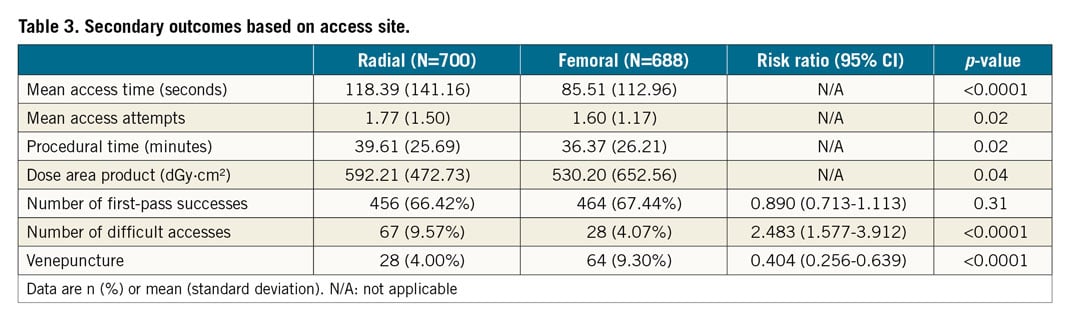
When compared to the TRA approach, TFA was associated with a significant reduction in the mean access time (p<0.0001), mean access attempts (p=0.02), number of difficult accesses (p<0.0001) and dose area product (p=0.04) (Table 3). Venepuncture was higher in the TFA (9.3%) compared with the TRA (4.0%) group (p<0.0001). US guidance resulted in improved procedural outcomes in all subgroup analyses compared with the SD technique. Use of US significantly reduced mean access time (93.1 sec US vs. 111 sec SD, p=0.01), mean access attempts (1.47 US vs. 1.9 SD, p<0.0001), number of difficult accesses (4.5% vs. 9.2%, p=0.0007), venepuncture (4.1% vs. 9.2%, p<0.0001) and improved first-pass success (73% US vs. 59.7% SD, p<0.0001) (Table 4).
Discussion
Among patients referred to our cardiac catheter laboratories, with or without ACS, the use of TRA for CA or PCI significantly reduced the primary composite endpoint of ACUITY major bleeding, MACE and vascular complications when compared with TFA. This was mostly driven by reduced ACUITY major bleeding (0.7% TRA vs. 2.1% TFA; HR 0.343, 95% CI: 0.123-0.959; p=0.041) (Supplementary Table 1). Major bleeding with femoral access in our study was lower than in published studies1,7. This could be explained by the non-ACS cohort studied and the local expertise in TFA. Nonetheless, our result still favoured TRA, in keeping with previous meta-analyses16,17, registries5,6 and the two recent large randomised trials7,8. RIVAL (RadIal Vs femorAL access for coronary intervention)7 initially did not show a significant difference when non-coronary bypass graft-related major bleeding was used. However, when the ACUITY bleeding definition was applied post hoc, the rate was significantly less with TRA. In fact, most previous radial versus femoral studies which favoured radial access were driven by major bleeding, despite variations in bleeding definitions. Females, diabetics and patients with BMI ≥25 kg/m2 demonstrated the greatest benefit from TRA. Whilst these findings were not clearly shown with previous trials, these groups of patients were most often associated with femoral access complications18,19.
US guidance did not affect the primary outcome compared with the SD technique. ACUITY major bleeding (1.4% US vs. 1.5% SD, p=0.85), MACE (0.75% US vs. 0.74% SD, p=0.98) and vascular complications (0.8% US vs. 0.6% SD, p=0.72) were similar in the US and SD approaches, respectively (Supplementary Table 2). This was most likely due to our study being underpowered as a result of the high arterial access success rate and low complication rate observed with the standard technique. By combining radial and femoral US analysis, a dilution of any clinical benefit may have occurred, especially in vascular complications, as demonstrated in the Femoral Arterial Access With Ultrasound Trial (FAUST)13. Another possible contributing factor is the similar BMI between the groups. Our study is the first double-randomisation trial and, although combining both radial and femoral US analysis, the findings were consistent with previous individual radial14,20 and femoral US13 trials. The mean access time for the femoral US group was shorter than for the femoral SD group (73.12 sec vs. 85.51 sec), but that for the radial US group was slightly longer than that for the radial SD group (133.64 sec vs. 118.39 sec). However, this is still well within the three-minute timeframe recommended by the Transradial Working Group21 before changing to an alternative access. This, coupled with a low number of access attempts and a high percentage of first-pass success, suggests that US guidance in TRA is possibly the technique of choice in primary PCI. The majority of the cases were carried out by advanced trainees and fellows; however, despite the operators’ relative inexperience, secondary outcomes remained superior in the US group. This indicates that the learning curve for both TRA and using US guidance is not as steep as previously reported22.
The number of first-pass successes was not significantly different between the TRA and TFA groups (65.1% vs. 67.6%, p=0.3), but the number of difficult accesses was much higher in the TRA group (9.6% vs. 4.1%, p<0.0001). When US was used, both the number of first-pass successes (73% US vs. 59.7% SD, p<0.0001) and of difficult accesses (4.5% US vs. 9.2% SD, p=0.0007) was significantly improved. Due to its small size, the radial artery is often more difficult to access. Minimising TRA attempts may reduce vessel injury, surrounding tissue haematoma and resultant arterial spasm which contributes to access failure23.
Limitations
This was a single-centre study; hence, recruitment took a prolonged period of time. The number of participating proceduralists was initially low as training was required from femoral-dominant to radial-based laboratories. Delays also occurred in acquiring US experience. Conversely, during the later stage, operators were reluctant to enrol patients due to increasing evidence favouring TRA in ACS patients. The low number of PCI patients enrolled was because of outpatients’ CA becoming ineligible when they came back for a follow-up PCI. Also, a proportion of patients were referred for non-ACS reasons, such as cardiomyopathy, ventricular arrhythmia and valvular surgery work-up. Combining TRA and TFA analyses for US versus SD may not reflect accurately the individual access benefit. The US versus SD comparison was underpowered for clinical outcomes. The high success rates for both radial (92.3%) and femoral (98.4%) access, coupled with low complication rates, especially in the radial group, mean that a larger sample size is required to show any difference in clinical outcome. Finally, given that this was a tertiary teaching hospital, the primary operators were mostly advanced trainees and interventional fellows.
Conclusions
In conclusion, our study showed that, for all patients referred to the cardiac catheter laboratories for CA and PCI, TRA significantly reduced the composite outcome, especially in females, diabetics and those with BMI ≥25 kg/m2 when compared with TRA. Whilst US guidance did not demonstrate a benefit in clinical outcomes compared with SD access, it improved the efficiency and overall success rate of arterial access. TRA and US guidance techniques were easily mastered by all operators.
|
Impact on daily practice The SURF trial showed that, for all patients referred for CA and PCI, TRA was superior and reduced the composite outcome when compared with TFA. Diabetics, females and patients with BMI ≥25 kg/m2 derived the most benefit from TRA. US guidance increased success rates in arterial access by reducing access time, attempts, number of difficult accesses, and venepuncture, and by improving first-pass success. US guidance in TRA can be the technique of choice in CA and PCI. |
Acknowledgements
We are grateful for the loan of the ultrasound machine during the early trial period by Fujifilm SonoSite and Western Sydney University. We are also appreciative of the support from all the cardiologists, advanced trainees, interventional fellows, nurses, research and clerical staff from the cardiology departments at Liverpool and Campbelltown hospitals for their support throughout the trial.
Conflict of interest statement
The authors have no conflicts of interest to declare.