Meta-analyses of individual participant data (IPD) aim to identify, appraise, and summarise the evidence from various studies that share the same research question or topic. Unlike most meta-analyses, they do not rely on data extracted from medical journals (i.e., aggregate data meta-analyses), rather, they handle and combine the original databases from eligible studies. IPD meta-analyses offer multiple potential advantages over aggregate data meta-analyses, including greater statistical power, more consistent definitions, outcomes, and follow-up times, subgroup and sensitivity analyses, and adjustments for confounding effects. IPD meta-analyses can produce the highest level of evidence when the synthesised data are quantitatively and qualitatively sufficient, the statistical approaches are appropriate, and the research question cannot be adequately addressed with individual trials. However, these advantages often demand an extraordinary collaboration among investigators, institutions, organisation, and companies, a considerable commitment of resources − both temporal and financial − and advanced statistical methods.
Access site selection for coronary procedures has been a matter of debate for a long time. In recent years, transradial access (TRA) has become the recommended route due to the observation in randomised trials and large-scale registries of reduced rates of major bleeding and vascular complications compared with transfemoral access (TFA). A recent comprehensive IPD meta-analysis of 7 randomised trials including 21,600 patients undergoing elective or urgent coronary angiography, with or without percutaneous coronary intervention (PCI), overcame the limitations of the individual trials by showing that TRA is associated with reduced mortality compared with TFA1. However, TFA is still needed when large-bore catheters are required, when the manipulation of catheters from the radial artery to the coronary arteries is challenging, and in cases where the radial artery is occluded or difficult to engage. Considering that TFA-related vascular complications are approximately 10 times more frequent than any other mechanical complication of coronary angiography or PCI and that many of these complications necessitate additional procedures and prolonged hospitalisation, the quest for strategies to improve TFA safety remains ongoing. In recent years, ultrasound-guided TFA (US-TFA) and vascular closure devices (VCDs) have been tested in randomised trials in the hopes of lowering vascular complications and bleeding rates.
In this issue of EuroIntervention, d’Entremont and colleagues provide the highest-quality evidence on the topic by pooling IPD from 4 randomised trials comparing US-TFA (1,208 patients) and standard non-US-TFA (1,233 patients) for coronary angiography or PCI2. This remarkable study concluded that patients who were allocated to US-TFA experienced fewer major vascular complications and major bleeding events compared with non-US-TFA (2.8% vs 4.5%; odds ratio [OR] 0.61, 95% confidence interval [CI]: 0.39-0.94; p=0.026) mainly driven by lower rates of major vascular complications (2.4% vs 4.0%; OR 0.58, 95% CI: 0.36-0.93; p=0.023) (Figure 1). These findings are reasonable overall and should promote a broader application of US-TFA over traditional palpation- and fluoroscopy-guided procedures. Indeed, US-TFA stands out not only for its simplicity and limited requirements in terms of costs and time but also for its higher accuracy. Indeed, this IPD meta-analysis showed that US-TFA was associated with a lower number of puncture attempts and a lower rate of venipuncture. Notably, the rates of major vascular or bleeding complications were consistent between fellows and consultants (pinteraction=0.81)2.
Although this IPD meta-analysis provides an outstanding opportunity for advancements, it still does not address questions surrounding the net prognostic effect of US-TFA. Indeed, the reduction in major vascular complications associated with US-TFA was essentially driven by a lower occurrence of haematomas >5 cm in diameter (2.1% vs 3.6%; OR 0.54, 95% CI: 0.33-0.89; p=0.016), while other more complex variants of vascular complications − including retroperitoneal haematoma, arteriovenous fistula, and femoral artery pseudoaneurysm, and surgery for lower limb critical ischaemia − were quite comparable between groups (Figure 1). Consistently, the difference in Bleeding Academic Research Consortium (BARC) 2, 3, or 5 events did not reach statistical significance, and the numerical trend observed was essentially driven by BARC 2 events (3.0% vs 4.2%, OR 0.68, 95% CI: 0.44-1.05; p=0.08), while the incidence of BARC 3 events was similar between groups (0.7% vs 0.6%; OR 1.32, 95% CI: 0.49-3.54; p=0.59) and no BARC 5 events (e.g., fatal bleeding) were observed in the study (Figure 1). Notwithstanding, in the as-treated analysis, accounting for crossover, a possible advantage in terms of BARC 2 emerged in favour of US-TFA2.
The study opens new research questions. Indeed, the study population included only 12.1% of patients suffering from peripheral vascular disease (PVD), and 65.5% of the procedures were coronary angiographies without PCI. In this context, it may be reasonable to suppose that the potential benefits of US-TFA would be most pronounced in patients with PVD undergoing PCI, especially when the coronary artery disease is complex and large-bore catheters are required. However, the limited number of patients with PVD did not adequately permit an exploration of this question, although a formal subgroup analysis did not reveal significant interaction. Consistently, the summary estimates from a complementary aggregate-level meta-analysis of randomised trials predominantly focused on PVD were in line with those of the IPD meta-analysis. Moreover, the subgroup analysis in terms of sheath size (≤7 Fr or >7 Fr) did not reveal significant differences (pinteraction=0.93). Overall, the persisting residual uncertainty about specific aspects of this matter is evident in the present IPD meta-analysis, as manifested by the constant differences between fixed- and random-effects summary estimates, and the constraints imposed by the available sample size permitted the authors to conservatively account for the differences in baseline risk across trials by random-slope mixed-effects models.
A provocative finding of this IPD meta-analysis is the highly significant interaction between the effects and the use of VCDs (pinteraction=0.009)2. Accordingly, the reduction of major vascular complications or major bleeding associated with US-TFA was substantial when a VCD was employed (2.1% vs 5.6%; OR 0.36, 95% CI: 0.19-0.69; p=0.002), while the benefit was no longer observed when a VCD was not employed (4.1% vs 3.3%; OR 1.21, 95% CI: 0.65-2.26; p=0.54). The interpretation of this finding is challenging. Indeed, it might be hypothesised that a synergistic effect between US-TFA and VCD use produced improved clinical outcomes. Yet, previous trials on VCDs have shown mixed results, and some considerations are required. Indeed, the study population of the present IPD meta-analysis exhibited an unbalanced use of VCDs between US- and non-US-TFA, and the results were not multivariable-adjusted. Moreover, a leave-one-out analysis demonstrated that the effect seems to be predominantly driven by the UNIVERSAL trial3. Finally, the subgroup analysis was not corrected for multiplicity, thereby limiting its finding to exploratory insights only.
In conclusion, can 4 negative/neutral RCTs reach a positive result? Yes, this is exactly the aim of meta-analyses, and this study offers important, summarised high-quality evidence on the potential benefits of US-TFA. Can this study conclude we should routinely use US-guided TFA? Maybe not; the number of patients is insufficient for individual hard endpoints, the results are not entirely consistent, and some points remain to be addressed. One may wonder whether TRA remains superior to TFA even when TFA is optimised through US guidance; however, TRA has been shown to reduce all-cause mortality, and this is only partially related to reduction of major bleeding1. Therefore, while TRA remains the recommended route for most coronary procedures, TFA is still needed in some cases. Optimising TFA remains technical and clinically relevant and should be considered as part of daily practice, while future studies will further assess its benefits on clinical outcomes.
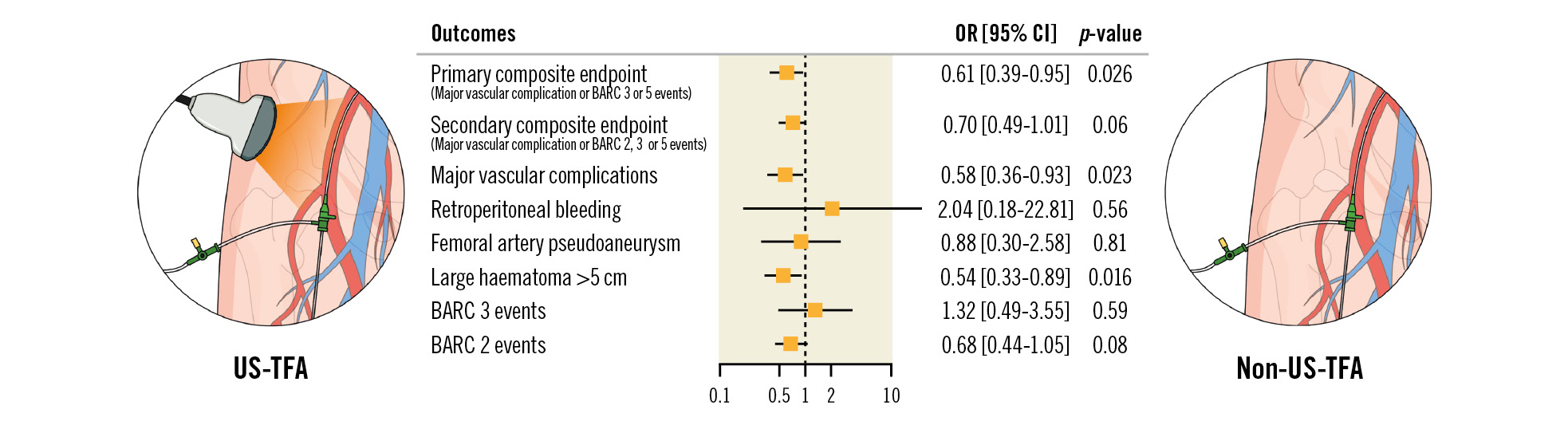
Figure 1. Main results of the IPD meta-analysis2. BARC: Bleeding Academic Research Consortium; CI: confidence interval; OR: odds ratio; US-TFA: ultrasound-guided transfemoral access
Conflict of interest statement
The authors have no conflicts of interest to declare.