Abstract
Aims: There is an increasing amount of data suggesting that transradial approach is associated with lower incidence of complications in vascular access site and improved clinical outcomes compared with transfemoral approach in the setting of ST-segment elevation myocardial infarction (STEMI). The objective of this study was to assess the safety and efficacy of radial versus femoral percutaneous coronary intervention (PCI) for patients with STEMI.
Methods and results: We searched MEDLINE, EMBASE, and Cochrane databases for randomised, case-control, and cohort studies comparing access-related complications and clinical outcomes from January 2001 to October 2011. Twenty-one studies involving 8,534 patients were identified. Transradial approach was associated with a significant reductions in major adverse cardiac events (odds ratio [OR] 0.56, 95% confidence interval [CI] 0.44-0.72, p<0.001), mortality (OR 0.55, 95% CI 0.42-0.72, p<0.001), and major bleeding (OR 0.32, 95% CI 0.22-0.48, p<0.001) compared to transfemoral approach. There was a shorter hospital length of stay with transradial access with a weighted mean difference of 2.23 days (95% CI –3.32-–1.14, p<0.001) compared to transfemoral access. There were no differences in fluoroscopic time, door-to-balloon time, and procedure time between the two access routes (p=0.09, p=0.38, p=0.82, respectively). The rate of access site crossover tended to be higher with transradial access (p=0.06).
Conclusions: This updated meta-analysis demonstrates that transradial PCI reduces the risk of significant periprocedural bleeding and improve clinical outcomes in patients with STEMI.
Introduction
Transradial access has been shown to be a safe and effective technique with a decreased incidence of major bleeding and composite endpoint of death, myocardial infarction (MI), or stroke compared with transfemoral access in patients undergoing coronary angiography or intervention1,2. Recently, transradial route is gaining popularity for primary percutaneous coronary intervention (PCI) in ST-elevation myocardial infarction (STEMI). It is well known that the transradial access has lower access site bleeding compared to the transfemoral route. Procedure related bleeding and consequent need for blood product transfusions are equally well known to result in higher mortality in patients undergoing primary PCI. However, any interventions reducing the risk of bleeding have reduced risk of mortality and ischaemic events in patients with significant bleeding at time of PCI3,4.
Several retrospective observational studies have reported the feasibility of transradial intervention for patients with acute MI5-7. However, none of these studies were powered to assess whether the use of the transradial instead of the transfemoral route may translate into an improved clinical outcomes in the setting of primary PCI. Recent publication of the RadIal Vs femorAL access for coronary intervention (RIVAL) trial8 has provided substantial evidence concerning transradial access in patients with STEMI. Therefore, we performed an updated meta-analysis of randomised trials and observational studies to assess the safety and efficacy of transradial PCI in patients with STEMI.
Methods
Data sources and searches
We identified relevant studies through electronic searches of MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials from 2001 through October, 30th 2011. Medical subject headings and keyword searches included the terms “radial access”, “transradial”, “myocardial infarction”, and “percutaneous coronary intervention”. Reference lists of selected articles and pertinent available quantitative meta-analyses were systematically reviewed for other potentially relevant citations. Data from unpublished sources were not searched or included. No language restriction was enforced.
Study selection and data extraction
Two investigators (J-SJ and T-HY) independently conducted the literature search, data extraction, and quality assessment by using a standardised approach. Selected publications were reviewed by the same investigators to assess if studies met the inclusion criteria: (1) comparison of the transradial versus transfemoral approach for a patient population with documented STEMI undergoing PCI, (2) clinical outcomes available: major adverse cardiac events (MACE), mortality, major bleeding, procedure time, fluoroscopy time, hospital stay, or access site crossover. Studies with a lack of outcome data, case reports, or duplicate reports were excluded from the analysis. Final inclusion of studies was based on the agreement of both reviewers. Two reviewers (J-SJ and K-IC) extracted relevant information from the articles including patient characteristics, study design, publication year, sample size, sheath size, primary outcome, and duration of follow-up.
Endpoints
The co-primary endpoints of this meta-analysis were (1) MACE, that is, death, recurrent MI, emergency PCI, or coronary artery bypass graft surgery, and stroke, (2) mortality, and (3) major bleeding. Secondary endpoints included hospital stay, fluoroscopic time, door-to-balloon time, procedure time, and access site crossover. Death was defined as in-hospital death or death at available follow-up from any cause. Major bleeding was defined as one of the following: fatal bleeding, intracranial haemorrhage or bleeding associated with a ≥3 g/dL haemoglobin drop or requiring transfusion or requiring surgery. For trials where the composite definition was not available, either transfusion rates or proportion of bleeding events associated with a ≥3 g/dL haemoglobin drop were substituted for major bleeding. Access site crossover was defined as need to puncture a second arterial access site.
Data synthesis and analysis
Continuous data were expressed as mean (SD) and weighted mean difference (WMD). The data from various studies were pooled and expressed as pooled WMD with 95% confidence interval (CI). We used odds ratio (OR) with 95% CI to express dichotomous data. The pooled effects were calculated using fixed-effects model (Mantel-Haenszel method) or random effects models (Dersimonian and Laird method). Where no significant statistical heterogeneity was identified, the fixed effects estimate was used preferentially as the summary measure. All p-values were 2-tailed, with statistical significance set at 0.05. To assess the effect of individual studies on the summary estimate of effect, we did an influence analysis, in which the pooled estimates were recalculated omitting one study at a time.
We assessed statistical heterogeneity between trials with I2 statistic, which is derived from Cochran’s Q and the degree of freedom [100×(Q–df)/Q)]9. I2 values greater than 25%, 50%, and 75% were considered evidence of low, moderate, and severe statistical heterogeneity, respectively. The likelihood of publication bias was assessed graphically by generating a funnel plot for the combined endpoint of MACE and mathematically by means of Egger’s test (p for significant asymmetry <0.1)10. For specific evaluation of the presence and extent of publication bias, we used trim-and-fill method according to Duval and Tweedie11, which imputes missing studies in the funnel plot based on symmetry assumptions.
Subgroup analysis was performed to assess the potential effect of study design (randomised versus non-randomised). All statistical analyses were performed using the Review Manager version 5.1 (The Nordic Cochrane Center, Copenhagen, Denmark) and MIX version 2.0 (BiostatXL, Sunnyvale, CA, USA).
Results
A total of 119 publications between January 2001 and October 2011 were screened. Duplicate reports, review publications, and studies that did not meet the inclusion criteria were excluded. Of the remaining 24 trials, three studies with unavailable clinical outcome data were excluded. Subsequently, 21 papers were included into the final analysis (Figure 1).
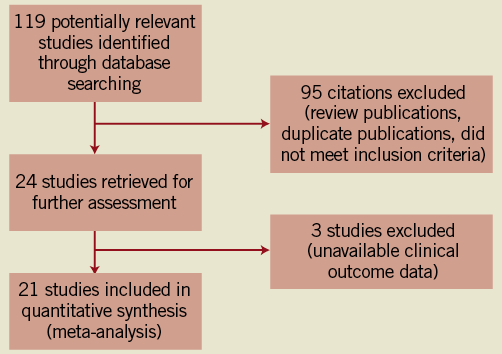
Figure 1. Trial flow chart for study inclusion.
The characteristics of included studies, the baseline demographics, and overview of the predefined endpoints of the study populations are presented in Table 1. Of the 8,534 patients in the final analysis, transradial approach was used in 3,594 patients whereas transfemoral approach was used in 4,940 patients. Eight studies were randomised trials that compared safety and efficacy of transradial versus transfemoral PCI8,12-18. The other 13 reports were registry studies with matched cohorts or consecutive patients19-31. The time frame for clinical outcome was varied across the included studies. All included studies reported data on the in-hospital follow-up, apart from seven studies8,13,15,16,21,23,27 in which follow-up data were recorded for 30 days, in one for nine months12, and in one for one year29.
Primary endpoints
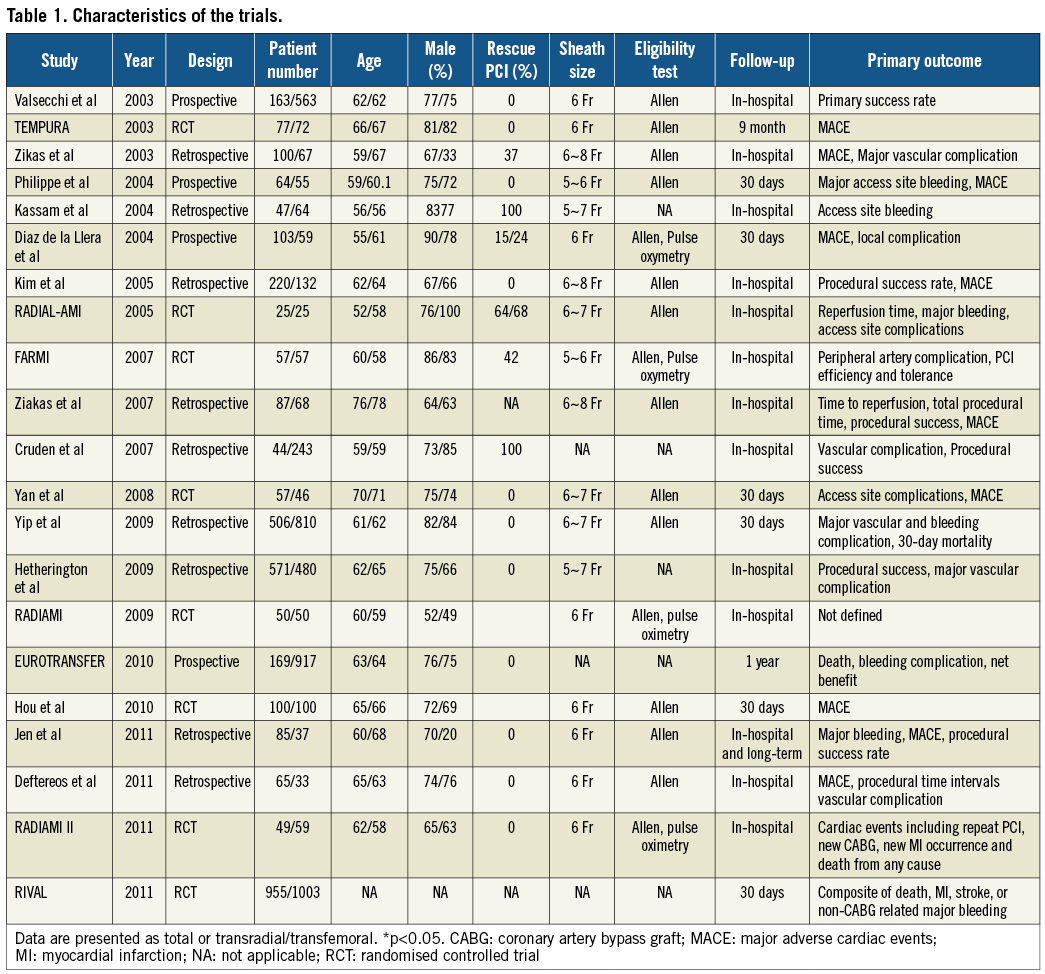
The MACE endpoint was reported in 20 of the trials (n=7,318). Overall, 106 among 3,188 patients in the transradial group developed MACE compared with 259 patients among 4,130 patients in the transfemoral group. Meta-analysis of these data demonstrated an OR of 0.56 (95% CI 0.44-0.72, p<0.001) for MACE in favour of the transradial group (Figure 2). There was no evidence of heterogeneity among the included studies (heterogeneity χ2=9.42, I2=0%, p=0.97). Subgroup analysis showed that MACE was significantly lower with transradial group regardless of the study design.
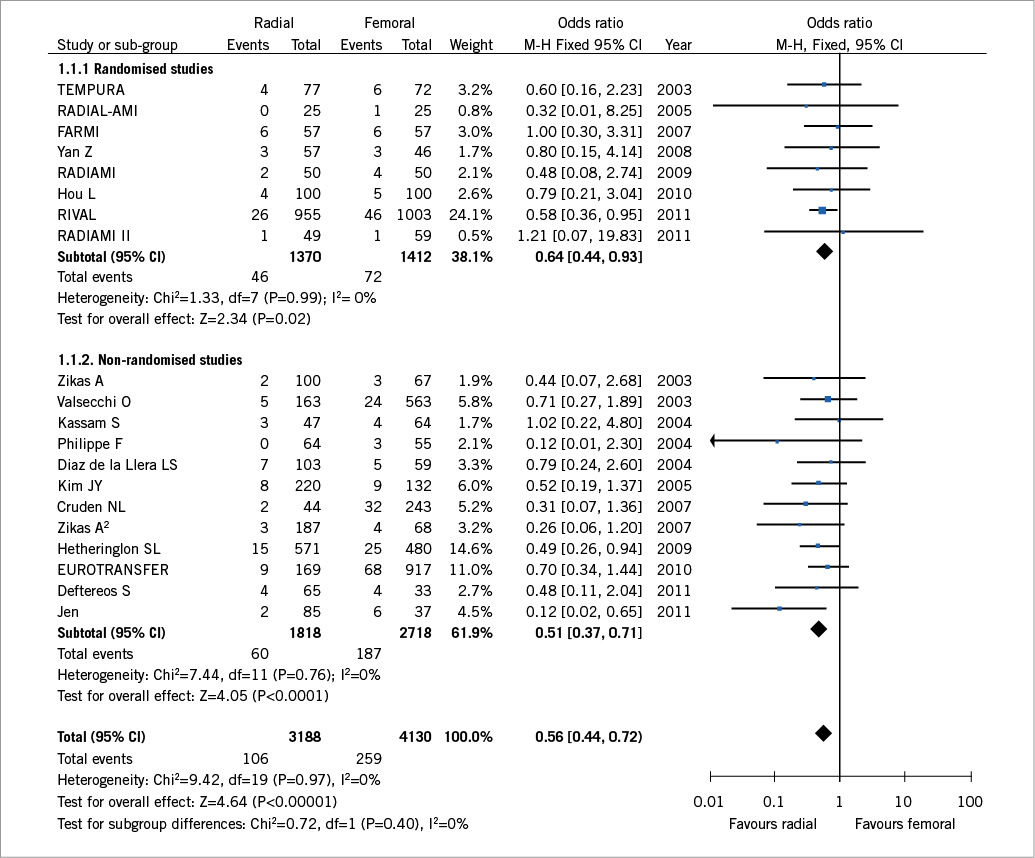
Figure 2. Forest plot of odds ratios comparing major adverse cardiac events in the transradial versus the transfemoral access sites stratified by study design. Size of data markers indicates the weight of the study.
The cumulative analysis of the included studies further supports the conclusion. Figure 3 depicts the summary ORs of all trials published up to a time point in a chronological order. None of the studies influenced the results to an extent that the conclusion would have changes: The sensitivity analysis of the risk of MACE with transradial approach after exclusion of one study at a time yielded effect sizes similar in magnitude and direction to the overall estimates. However, after exclusion of the RIVAL study8 from the dataset of randomised trials and repeating the analysis disclosed no statistically significant difference between transradial and transfemoral intervention (OR 0.73, 95% CI 0.40–1.33, p=0.31).
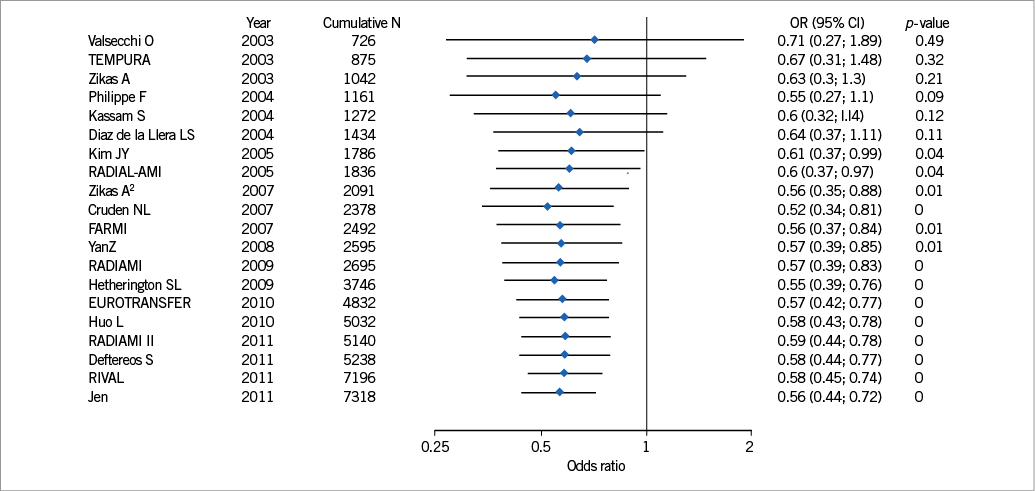
Figure 3. Cumulative analysis of major adverse cardiac events. This figure illustrates the time-course of the odds ratio when performing a meta-analysis after each new study in a chronological order.
A total of 79 among 3,594 deaths occurred in the transradial group and 202 of 4,940 in the transfemoral group. The transradial approach was associated with a significantly reduced incidence of death compared to patients with transfemoral approach (OR 0.55, 95% CI 0.42–0.72, p<0.001, Figure 4). Heterogeneity was not observed across the studies (heterogeneity χ2=8.37, I2=0%, p=0.97) and data were assessed by the fixed-effects model. Similarly, after exclusion of the RIVAL study8 from the dataset of randomised trials and repeating the analysis failed to demonstrate a statistically significant benefit of the transradial over the transfemoral approach (OR 0.70, 95% CI 0.35–1.38, p=0.30).
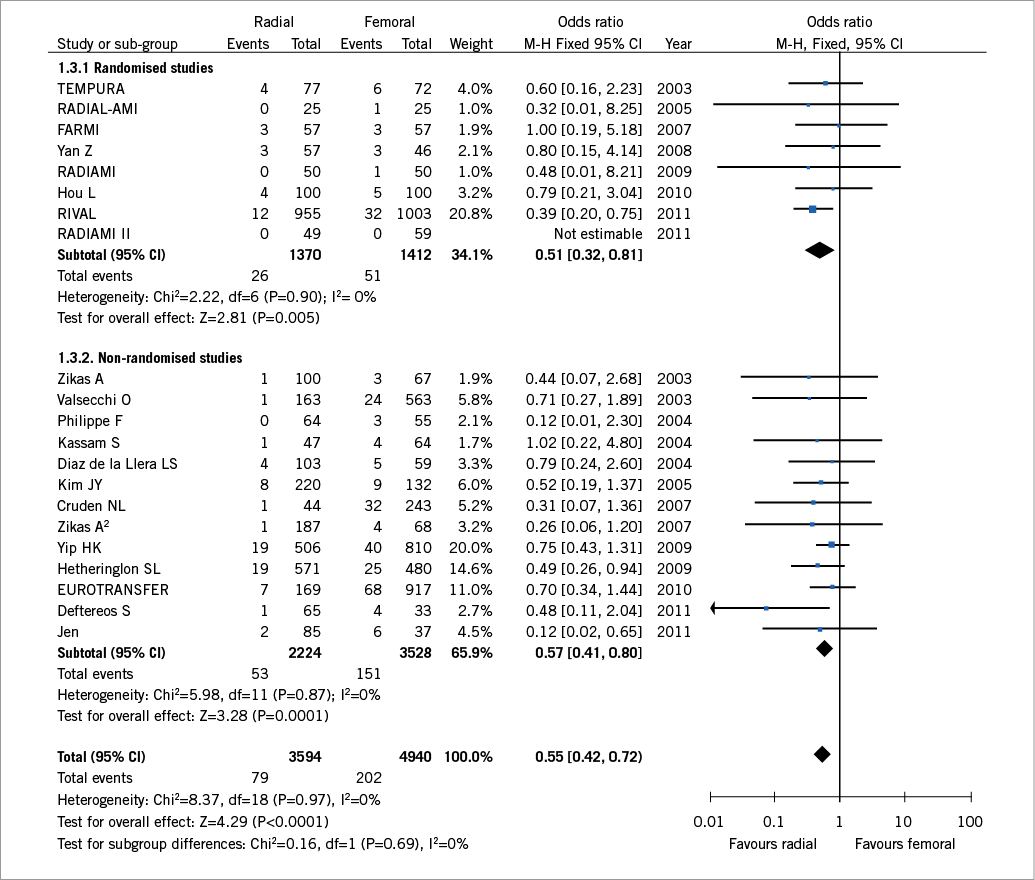
Figure 4. Forest plot of odds ratios comparing mortality in the transradial versus the transfemoral access sites stratified by study design. Size of data markers indicates the weight of the study.
Eleven total major bleeding occurred among the 3,694 patients with transradial approach and 118 in the 5,040 patients with transfemoral approach. Transradial approach was associated with a significantly reduced incidence of major bleeding compared to patients with transfemoral approach (OR 0.32, 95% CI 0.22–0.48, p=0.007, Figure 5). No heterogeneity between studies was detected (heterogeneity χ2=18.25, I2=0%, p=0.83). Stratified analysis by the study design suggested lower odds of major bleeding with transradial approach in non-randomised studies (OR 0.20, 95% CI 0.11–0.35, p<0.001) compared with randomised trials which failed to show significant benefit of transradial approach (OR 0.61, 95% CI 0.35–1.08, p=0.09).
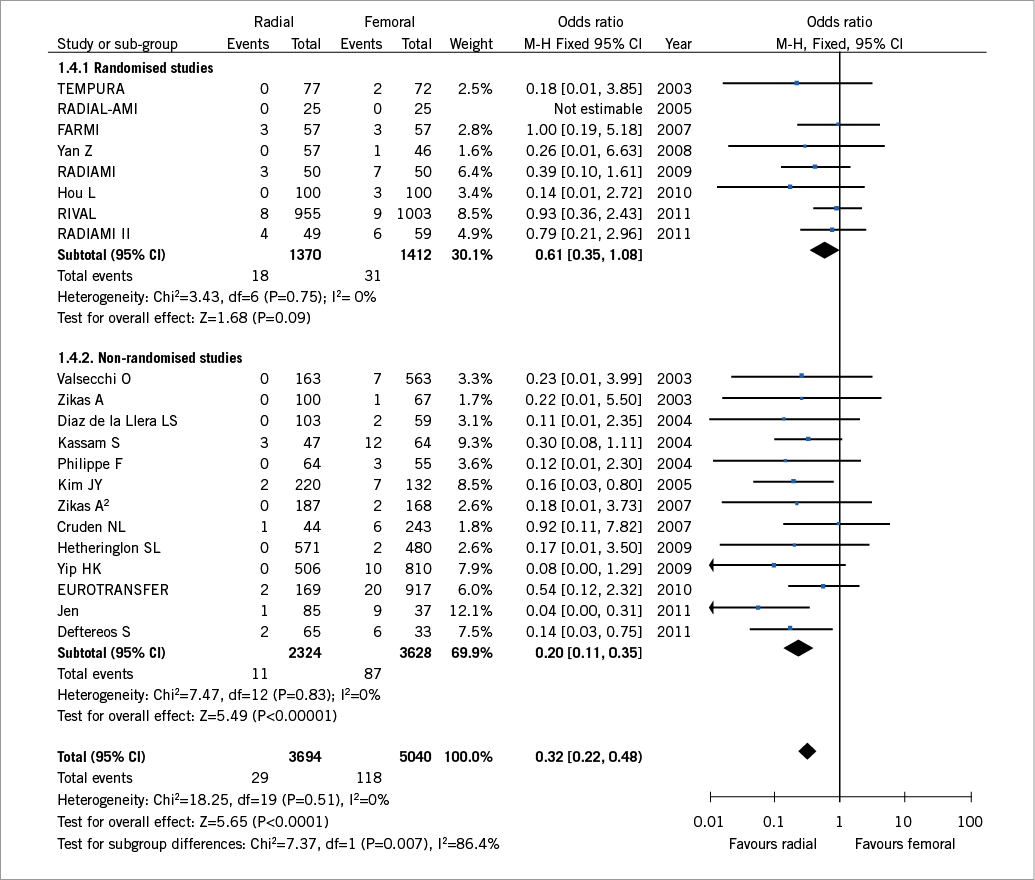
Figure 5. Forest plot of odds ratios comparing major bleeding outcomes in the transradial versus the transfemoral access sites stratified by study design. Size of data markers indicates the weight of the study.
Secondary endpoints
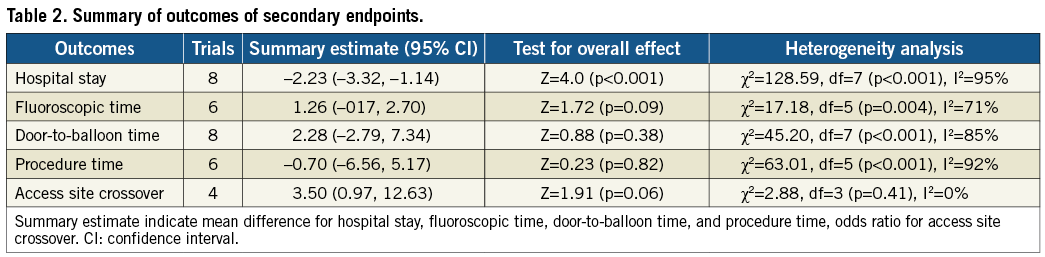
There was a shorter hospital length of stay with transradial approach with a WMD of 2.23 days (95% CI 3.32-1.14, p<0.001) compared to transfemoral approach. There were no significant differences in fluoroscopic time, door-to-balloon time, and procedure time between the two access routes. The rate of access site crossover was tended to be higher with transradial compared with transfemoral access (Table 2).
Publication bias
Assessment of publication bias using odds ratio of MACE of the included studies demonstrates a symmetric funnel plot with no evidence of publication bias (Figure 6), confirmed by means of a negative Egger’s regression-based test (p=0.31). The trim-and-fill method indicated that two missing studies were needed to achieve a symmetrical funnel plot.
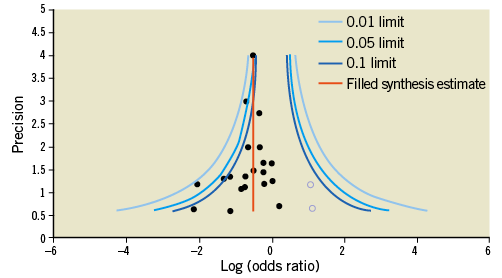
Figure 6. Funnel plot of included studies for major adverse cardiac events data suggesting the absence of publication bias demonstrated by a symmetric funnel plot. The trim-and-fill method was used to calculate the true centre of the funnel (indicated by the vertical line). The black circle indicates the original confidence intervals of the log odds ratio; the empty circle indicates the corresponding value when the additional imputed study is also considered.
Discussion
In the present meta-analysis of twenty-one studies consisting of 8,534 patients, we found that adoption of transradial route for primary PCI in patients with STEMI is associated with a 44% reduction in the risk of MACE and a 45% reduction in the risk of mortality in comparison with transfemoral approach. This is in agreement with a previous meta-analysis of randomised and observational studies including 3,324 patients with STEMI32, which demonstrated a 46% reduction in mortality with transradial approach. In addition, transradial approach reduced major bleeding compared to transfemoral approach without significant differences in fluoroscopic time, door-to-balloon time, and procedure time. There was a lower hospital length of stay with transradial approach compared to transfemoral approach. However, the rate of access site crossover was tended to be higher with transradial access compared with transfemoral access.
The RIVAL trial8 provides a contemporary comparison of the radial versus femoral access and contributed to the substantial proportion of the present data analysed. The findings of better outcomes in the STEMI subgroups of RIVAL study are consistent with previous small randomised trials and large observational studies. Recently, results of the Radial versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome (RIFLE STEACS) trial33 were presented at annual meeting of Transcatheter Cardiovascular Therapeutics. Romagnoli et al showed that transradial access was associated with a significantly reduced incidence of net adverse clinical events (21.0% s. 13.6%, p=0.003), bleeding event (12.2% vs. 7.8%, p=0.026), and cardiac death (5.2% vs. 9.2%, p=0.02) compared with transfemoral group with similar incidence of MI, target lesion revascularisation or stroke.
Major bleeding has deleterious impact on clinical outcomes after primary PCI in patients with STEMI34,35. In a report from the ACUITY trial, in which 56% of patients with acute coronary syndromes underwent PCI, bleeding was stronger than nonfatal MI as a predictor of 30-day death4. In addition, there is evidence that less bleeding may be associated with fewer adverse events36,37. In a meta-analysis by Jolly et al2, transradial access was associated with a 73% reduction in the incidence of major bleeding compared with transradial access, while there was also a trend toward fewer adverse cardiovascular events with transradial access. Results of our study correspond with those of earlier studies which reported that reduced incidence of major bleeding with transradial approach is associated with reduced rates of adverse clinical events. However, stratified analysis of our results by the study design failed to demonstrate significantly decreased incidence of major bleeding with transradial access in randomised trials (OR 0.61, 95% CI 0.35-1.08, p=0.09).
Despite the growing evidence of reduction in mortality and major bleeding episodes with the transradial access, technical difficulties, higher failure rate, increased radiation exposure, and significant learning curve associated with this technique preclude most interventional cardiologists to start primary PCI via radial route. In our meta-analysis, the rate of access site crossover tended to be higher with the transradial compared with transfemoral access. Furthermore, crossover rates in the transfemoral group might be underestimated because many cardiologists regard the femoral artery as a fall-back option against possible failure of radial puncture.
MACE among patients undergoing either the transradial or transfemoral approach has been previously reported in several trials and meta-analyses. In the Harmonizing Outcomes with Revascularization and Stents in Acute Myocardial Infarction (HORIZONS-AMI) trial, transradial compared to transfemoral access was associated with significantly lower 30-day and 1-year rates of MACE and major bleeding in patients with STEMI treated with primary PCI and contemporary anticoagulation regimens38. Jolly et al2 reported a trend toward a reduced incidence of MACE among patients undergoing transradial PCI and two other studies reported a significantly lower rate of MACE in transradial group compared with transfemoral group32,39. Although the RIVAL study8 contributed 66% of all patients, Mamas et al39 reported 38% lower incidence of MACE in transradial group suggesting an overall benefit of transradial over transfemoral approach. They pooled nine randomised controlled trials without significant heterogeneity and there was no evidence of publication bias. Results of the present study correspond with the results of previous meta-analysis. However, analyses of 13 registry studies and eight randomised trials from the present work, including >8,000 patients, further support the safety and efficacy of transradial access for STEMI patients with an OR of 0.56 for MACE in favour of the transradial group compared with the transfemoral group without significant heterogeneity or evidence of publication bias. However, exclusion of the RIVAL study8 from the dataset of randomised trials could not consistently demonstrate significant benefit of transradial approach over transfemoral approach in terms of MACE and mortality.
Meanwhile, we further analysed secondary endpoints of hospital stay, fluoroscopic time, door-to-balloon time, and procedure time to compare actual benefit or hazard associated with access site. Early mobilisation of the patients improves compliance and reduces the cost of PCI40. There was a shorter hospital length of stay with transradial access in our analysis with a WMD of 2.23 days (p<0.001) compared to transfemoral access. The result of our study is in agreement with previous studies. Dirksen et al41 reported that most patients could be discharged within four days without increased rates of adverse events following primary PCI with transradial stent implantation under glycoprotein IIb/IIIa blockade with tirofiban in the setting of STEMI. No significant differences in door-to-balloon time and procedure time between transradial and transfemoral group may have been caused by a progressive improvement in access devices, technical skills, and catheterisation laboratory facilities for transradial intervention since its introduction in the setting of primary PCI.
Study limitations
The present study has several limitations to be addressed. First, the systematic reviews have inherent limitations, and the results obtained with meta-analyses should be analysed accordingly. Because event rates in observational studies and randomised controlled trials were computed and pooled together without exploiting multivariable adjustment and unadjusted risk estimates were provided by 13 observational studies included in our meta-analysis, there might be selection and performance biases. Thus, we tried to overcome these limitations by influence analysis with recalculating the pooled estimates after exclusion of one study at a time, cumulative analysis performing a meta-analysis after each new study in a chronological order, and sensitivity analysis according to the randomisation. Second, some results of our meta-analysis have significant heterogeneities, which is frequent in meta-analyses performed on global data. Third, definition of endpoints was different across the included studies. Fourth, we could not have access to patient-level data to further propensity analysis or stratified analysis to better define differences between the treatment groups. Finally, included trials are of short duration and they are not adequately powered to measure clinical outcomes such as death and recurrent MI.
Conclusions
In this meta-analysis of twenty-one studies including 8,534 patients with STEMI, we observed a significantly reduced incidence of mortality, major bleeding, and MACE when primary PCI is done via transradial route. There is an urgent need for a clinical trial in view of the potential for transradial route to reduce clinical outcomes. Furthermore, a meta-analysis cannot be a substitute for a large, adequately powered, randomised controlled trial. Nevertheless, this meta-analysis adds to the growing body of literature evidence that transradial PCI might be beneficial in terms of major bleeding and mortality among STEMI patients undergoing primary PCI.
Acknowledgements
This work was supported by a grant from Inje University, 2011.
Conflict of interest
The authors have no conflicts of interest to declare.

