Multiple large randomised trials including more than 18,000 patients comparing transradial vs. transfemoral access for coronary intervention have shown that transradial access improves outcomes including major vascular complications, bleeding and mortality1-3. The largest trial, the MATRIX trial (Minimizing Adverse Haemorrhagic Events by TRansradial Access Site and Systemic Implementation of angioX, N=8,404) showed a reduction in all-cause mortality with transradial compared to transfemoral access1. However, some operators have been reluctant to use transradial access in complex percutaneous coronary intervention (PCI) such as left main due to the need for larger bore access and increased guide support.
In this issue of EuroIntervention, Chen and colleagues present the observational analysis of radial vs. femoral access in the EXCEL (Evaluation of XIENCE Versus Coronary Artery Bypass Surgery for Effectiveness of Left Main Revascularization) trial4.
The EXCEL trial randomised 1,905 patients with left main disease to either PCI or coronary artery bypass graft (CABG) surgery. This analysis included 931 patients, of whom only 248 (26.6%) underwent transradial access vs. 683 (73.4%) who underwent transfemoral access for left main PCI.
Patients with transradial access were more likely to be treated in Canada and Europe, to have 6 Fr instead of 7 Fr procedures and to receive heparin instead of bivalirudin for their procedures. While the SYNTAX score was not different, operators performing transradial procedures were more likely to use a provisional one-stent strategy instead of a two-stent strategy, and less likely to use haemodynamic support with similar rates of procedural complications and procedural success.
The rate of death, myocardial infarction (MI) or stroke was not different between transradial and transfemoral left main PCI (15.7% vs. 14.8%, p=0.72) at three years. The rate of Thrombolysis In Myocardial Infarction (TIMI) major, minor or minimal bleeding was 4.8% with radial access vs. 8.8% with femoral access, p=0.05. For Bleeding Academic Research Consortium (BARC) 3-5 major bleeding, the rates were 0.8% with radial access vs. 2.8% with femoral access, p=0.07. Using propensity-adjusted models, there was no significant difference in either ischaemic or bleeding events. The authors conclude that either access site approach is fine for left main PCI.
Should observational data outweigh large-scale randomised trials?
It is common that observational analyses are published after large-scale randomised trials and differ in their findings. It is important that clinicians understand the biases in observational data and avoid being swayed against the results of rigorous randomised trials. It is likely that patients who received transradial procedures were different; they were recruited at different centres and had procedures carried out by different operators.
Observational data are important when there are insufficient data from randomised trials. There were few left main PCI procedures in the randomised trials and, as such, safety data for the transradial approach for complex left main procedures are important. This analysis from the EXCEL trial supports the concept that LM PCI is as safe using the transradial approach as it is using the transfemoral approach. Two of the largest randomised trials have shown that expertise is important with transradial intervention, such that expertise is probably also important to make transradial PCI of the left main safe1,5. Finally, another observational analysis of 853 patients from the Coronary Bifurcation Registry showed similar ischaemic outcomes with transradial and transfemoral LM PCI6.
One of the major limitations of transradial access is the small diameter of the radial artery. However, techniques have evolved to allow larger bore guide catheters using the sheathless technique in order to permit complex PCI from the radial artery7. It is of note that, despite this, many radial operators still prefer to stick to a 6 Fr guiding catheter and adopt a single stenting technique, as shown by this analysis. While it cannot be ruled out that simpler bifurcation anatomies were tackled via the radial instead of the femoral access, it remains intriguing to hypothesise that radial operators may elect to approach similarly complex coronary artery disease with a less complex PCI armamentarium.
Finally, one of the most important limitations of the EXCEL analysis is that it was underpowered to detect differences in bleeding between transradial and transfemoral PCI. Figure 1 illustrates the effect on BARC 3-5 bleeding in the EXCEL trial and MATRIX trial, showing a very consistent directional effect in both trials. If a study only has 50% power to detect a difference, then it is like flipping a coin that the trial will show a significant difference if a difference exists.
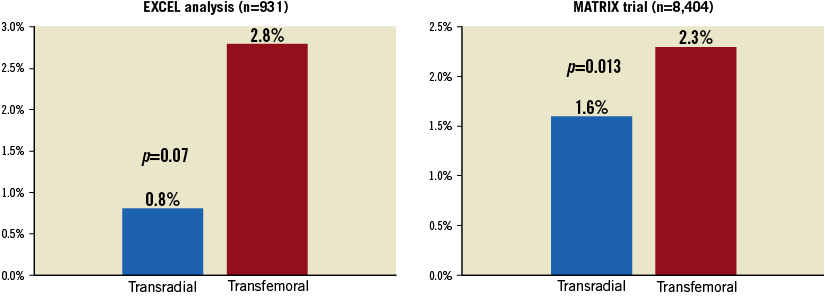
Figure 1. Major bleeding (BARC 3 or 5) from the EXCEL trial and the MATRIX trial.
Practice is changing with transradial access rising globally. The fact that the use of radial access was not even mentioned or reported across the multiple SYNTAX trial substudies suggests that a true minority of PCI patients received radial access in this pivotal trial, if any. The rates of transradial access are still lower in the USA than in the rest of the world, but transradial access is rapidly growing in the USA. In conclusion, in operators with radial expertise, transradial left main PCI is safe and effective. Finally, based on the totality of the data, transradial is likely to reduce bleeding complications compared to transfemoral left main PCI and, unlike in EXCEL, may allow shorter hospitalisation or even same-day discharge procedures, which may ultimately further minimise PCI-related costs and improve patient satisfaction.
Conflict of interest statement
S. Jolly has received grant support from Boston Scientific. M. Valgimigli has received grant support from Terumo, The Medicines Company, Abbott and Medicure.