Abstract
Aims: To assess the safety and efficacy of a novel sheathless (SH) 6.5 Fr (French) hydrophilic-coated guiding catheter (GC) compared to the standard 5 Fr GCs in transradial coronary interventions (TRI).
Methods and results: Patients undergoing TRI with 6.5 Fr SH or 5 Fr GCs were included. Baseline characteristics and in-hospital outcomes were recorded. Primary endpoints were procedural success and presence of radial pulse at discharge. Secondary endpoints were successful GC support, in-hospital adverse events, access-site complications, procedural duration and contrast load. There were 269 patients with 146 procedures in each group. The SH GC group had more non-ST elevation MI, in-stent restenosis, high-risk and bifurcation lesions. Procedural success in both arms was 95.2%. One patient in each group (0.7%) experienced radial artery occlusion (RAO) after TRI, without clinical sequelae. One access-site haematoma and one minor stroke occurred in the 5 Fr group (none in the SH group, both p=ns). Mean procedure time (52±21 vs. 45±21 minutes, p=0.004) and contrast load (160±45 ml vs. 140±45 ml, p=0.003) were greater in the SH group.
Conclusions: Both 6.5 Fr SH GCs and 5 Fr GCs achieved high procedural TRI success with low RAO rates. The SH GC eliminated the disadvantages of the 5 Fr GC whilst maintaining the advantage of low RAO rates, and may become the GC of choice in TRI.
Introduction
Transradial coronary intervention (TRI) is being increasingly performed. The transradial approach has been shown to result in reduced local access complication rates and major adverse cardiac events, although procedural success rate was slightly lower1,2. TRI has a steeper learning curve however, and many operators still prefer the transfemoral approach. Further uptake of TRI is also limited by procedural failures due to radial artery spasm (RAS) and radial artery occlusion (RAO) that can occur in up to 8%3 and between 3-10%4,5 respectively, with standard 6 Fr guiding catheters.
The 5 Fr guiding catheters (GC) as compared to the 6 Fr GCs reduce patient discomfort, radial artery spasm and the rate of RAO during TRI6,7, although there is a need to crossover to the 6 Fr GCs in a small proportion of cases8. This miniaturisation of GCs, with 4 Fr GCs recently reported9, has been termed “slender TRI”. The main disadvantages of the 5 Fr (or smaller) GCs are the smaller inner diameter limiting its usage in complex PCI, and less back-up support during TRI.
Recently, a novel sheathless (SH) hydrophilic coated GC (Eaucath GC) with an inner diameter equivalent to a standard 6 Fr GC and an outer diameter slightly larger than a conventional 4 Fr sheath (virtual 4 Fr GC) was introduced by Asahi, Tokyo, Japan (Figure 1). This SH GC theoretically maintains the advantage of the 5 Fr GC’s smaller profile, but eliminates disadvantages such as an inability to perform complex PCI as well as the reduction of guide support.

Figure 1. Left: inner dilator (white), sheathless hydrophilic coated guiding catheter (black). Middle: sheathless guiding catheter with the inner dilator within (distal end). Right: sheathless guiding catheter with the inner dilator seen within (proximal end).
The aims of this study were to evaluate the safety and efficacy of a novel sheathless system compared to the 5 Fr GC in patients undergoing TRI in a single centre.
Methods
Patient population and data collection
Patients undergoing TRI between November 2008 and September 2010 at our institution were studied. Patients were included if use of a 5 Fr or the SH system was planned. Baseline demographics and characteristics, the size/shape of GCs, anatomical and procedural characteristics (including fluoroscopy/procedural duration and contrast load), procedural success and in-hospital adverse cardiac events were recorded.
Procedures were carried out by two interventional cardiologists (PC, VL) experienced in TRI. The choice of GC was determined by clinical and anatomical features as well as by operator preference. Initially, the 5 Fr systems were the default GCs of choice; after the introduction of the sheathless 6 Fr GCs, this system was used exclusively after a brief transition period. Our institutional review board approved this study.
Procedure
After local anaesthesia, radial artery access was obtained with a 5 Fr sheath, and a “cocktail” of verapamil, heparin and nitroglycerine were administered. This “cocktail” was given regardless of whether the PCI was performed with a 5 Fr or SH system.
If a 5 Fr GC was selected, it was advanced through the 5 Fr sheath and passed to the coronary ostium using standard technique. Upon completion of TRI, the 5 Fr GC and sheath were removed and a compression bandage was applied.
The SH system does not require a sheath introducer during PCI. The catheter has a hydrophilic coating along its entire length, and has a removable central dilator that extends beyond the distal catheter tip to facilitate catheter insertion into the radial artery over a standard J- or Glide- wire (Figure 1). Multiple GC shapes are available including Judkins left and right (JL, JR), Amplatz left (AL), Hockey stick (HS), and back-up left curves (PB, SPB, SC) (Figure 2). The inner diameter of this GC is 1.79 mm (0.070 inches), similar to the standard 6 Fr GC, and the outer diameter is 2.16 mm, which is smaller than the 2.29 mm outer diameter of a 5 Fr sheath and slightly larger than the 2.0 mm outer diameter of a 4 Fr sheath (Figure 3). Compared to conventional GCs, these SH catheters are thicker walled (to increase kink resistance) due to an extra layer of wire braiding and the hydrophilic coating.

Figure 2. Various sheathless guiding catheter curves.

Figure 3. Comparison of the outer diameters of various sheath sizes and the sheathless guiding catheter.
The SH system was delivered using a different technique. After radial access with a 5 Fr introducer sheath and administration of the “cocktail”, the 5 Fr sheath was removed over a standard J-tip steel guidewire or Glidewire, and the SH system with its dedicated inner dilator was advanced over the wire as a single assembly to the ascending aorta. The inner dilator was removed while still in the ascending aorta and the SH catheter was then further advanced over the wire to the aortic root and manoeuvred to the coronary ostium. Subsequent PCI procedures were performed according to operator preference.
After the procedure, the SH catheter was disengaged and the inner dilator and guidewire were reintroduced into the catheter to straighten the distal tip. This assembly was then removed as a single unit and a compression bandage was applied.
Endpoints
The primary endpoints of the study were procedural success and presence of palpable radial artery pulse at discharge. Procedural success was defined as successful radial puncture, GC cannulation, residual stenosis of less than 30% and absence of major procedural complications (i.e., death, emergency bypass surgery or sustained coronary occlusion).
The secondary endpoints were successful GC engagement and adequate support (without having to change to a GC of a different size or switch to the transfemoral route); major in-hospital adverse events (myocardial infarction, stroke, target vessel revascularisation and death), local access site complications, fluoroscopy/procedural duration and contrast load.
Statistical analysis
Data are expressed as mean ± standard deviation for continuous variables and as absolute and relative frequencies for categorical variables. Categorical variables were compared using the Pearson’s Chi-square analysis or the Fisher’s exact test. The Student’s T test was used to compare continuous variables of normal distribution and the Mann-Whitney U test was used to compare continuous variables of abnormal distribution between groups. A p value of <0.05 was considered statistically significant, with all reported p value two-tailed. Statistical analyses were performed using SPSS version 16.0 (SPSS Inc., Chicago, IL, USA). All authors have read and agree to the manuscript as written.
Results
Patients and procedural characteristics
Two hundred sixty-nine patients (mean age 57.3 ± 10.7 years, range 33 to 84) underwent 288 procedures. There were 146 attempts in the SH group with four crossovers to the 5 Fr group; there were 146 attempts in the 5 Fr group, including the four crossovers from the SH group. Baseline characteristics are shown in Table 1. There were no significant differences between the two groups, except for more patients with non-ST elevation MI in the SH group.
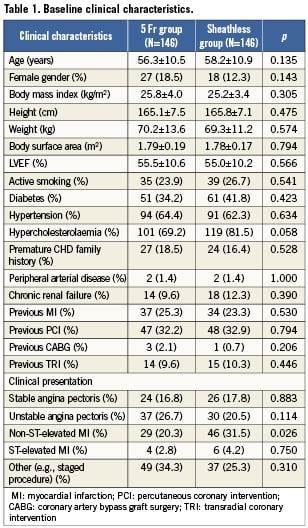
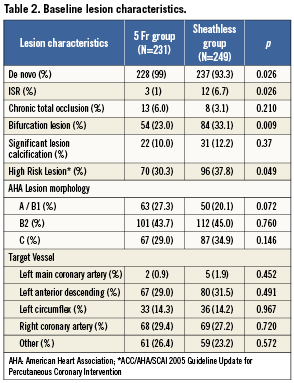
Baseline lesion characteristics are shown in Table 2. There were significantly more in-stent restenosis, high-risk and bifurcation lesions in the SH group as compared to the 5 Fr group.
Procedural success in both arms was 95.2% (Table 3). In the SH group, four cases were switched to 5 Fr GCs due to tortuous innominate/right subclavian arteries resulting in engagement failure, and in three cases, the procedures were unsuccessful due to failure to recanalise chronic total occlusions (CTO). All procedural failures due to inability to engage the SH GC were in the first one-third of the cases. In the 5 Fr group, three cases crossed over to the transfemoral route (one due to radial artery spasm, and two because of extreme kinking of the right subclavian artery), three cases crossed over to 6 Fr GCs (due to inadequate backup support), and one case was due to failed CTO recanalisation.
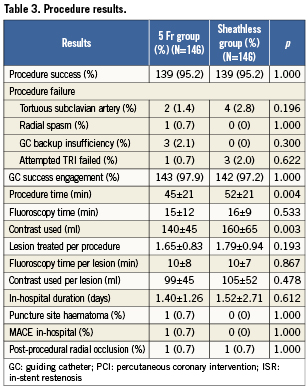
One patient in the SH arm (0.7%) experienced radial spasm (during diagnostic angiography) and subsequent loss of pulse after TRI. Duplex ultrasound of this patient revealed a radial artery diameter of only 1.7 mm. One patient in the 5 Fr arm (0.7%) had asymptomatic artery occlusion. Both patients had no clinical sequelae. There was one access site haematoma in the 5 Fr group versus none in the SH group (p=ns). There was one in-hospital adverse event (minor stroke) in the 5 Fr arm (none in the SH arm, p=ns). One case of non-flow limiting guide-induced left main artery dissection occurred in the SH group, likely due to usage of too large a curve (PB 4.0 instead of PB 3.5). Intravascular ultrasound showed a limited dissection flap within a large 5.5 mm diameter left main artery. No intervention was required, in-hospital course was uncomplicated and repeat angiography at six weeks showed complete healing.
The mean procedure time was longer in the SH group as compared to the 5 Fr group (52±21 vs 45±21 min, p=0.004), and total contrast load was greater in the SH group (160±45 ml vs 140±45 ml, p=0.003).
Discussion
TRI is increasingly performed, with the standard 6 Fr GCs employed by most centres and operators. However, Saito et al demonstrated that, based on the radial artery inner diameter, only 72.6% of female and 85.7% of male Asian patients can physically accept the 6 Fr sheath10.
The ratio between the radial artery to sheath diameter has been shown to be an important predictor of reduction of radial artery flow after TRI, and radial occlusion rates are significantly lower if the ratio of radial artery inner diameter/sheath outer diameter is equal to or greater than 1.010. Thus, smaller diameter GCs and sheaths (termed “slender TRI”) would be expected to reduce radial artery spasm and radial artery occlusion rates.
Previous studies demonstrated the feasibility of performing TRI using 5 Fr GCs without significant differences in the procedural success rates as compared to standard 6 Fr GCs6-8. Use of 5 Fr GCs resulted in less patient discomfort and a 1% radial artery occlusion rate (as compared to 6% with 6 Fr GCs)6,7. These advantages of the 5 Fr GCs are however, offset by its limited usage in complex PCI (kissing-balloon technique in bifurcation lesions, use of a cutting balloon, rotablator atherectomy, mechanical thrombectomy, certain intravascular ultrasound devices, or when stents >4.0 mm are required), and inadequate guide support during the PCI procedure8. Previous studies demonstrated that in 3-5% of cases, a crossover from 5 Fr to 6 Fr GCs was required due to insufficient backup support11,12. Our experience was similar with three cases (2%) requiring a switch from 5 Fr to 6 Fr GCs due to poor backup support whereas none occurred in the SH arm.
In this study, the SH system with its 6.5 Fr inner lumen enabled more complex PCI to be performed (such as kissing balloon inflations for bifurcation lesions, rotational atherectomy use of thrombectomy catheters and intravascular ultrasound), yet achieving an efficacy similar to the 5 Fr GCs, and with a very low radial artery occlusion rate (0.7% in both groups).
Noteworthy is the fact that the only radial artery spasm and occlusion in the SH group occurred in the first one-third of the experience and the patient had a very small calibre radial artery (1.7 mm). In over 300 cases using this novel GC, this is the only radial occlusion we have experienced (unpublished data). The very low radial occlusion rate in both groups is likely due to the fact that in 85-90% and 90-95% of patients, the outer diameter of 5 Fr sheaths (2.3 mm) and SH GCs (2.16 mm) respectively, do not exceed the radial artery inner diameter10. This downsizing (as an introducer sheath is not required) is perhaps the most significant advantage of the SH system. The outer diameter of the SH catheter at the distal end of the radial artery is less than that of the 5 Fr introducer sheaths, and it is at this segment where the radial artery size is the smallest and where spasm and occlusion most likely occur. Also, the entire SH catheter is hydrophilic coated, and use of hydrophilic coated catheters or sheaths during TRI has been shown to reduce radial artery spasm13,14. Our results are consistent with an earlier single centre report of 100 cases using the SH system where the radial artery occlusion rate was 2%15.
As an introducer sheath is not required for the SH system, direct motion transmission from the radial access site to the guide tip at the coronary ostium may occur. This, together with the hydrophilic coating, may cause the system to be less stable or slip more easily as compared to the usual 5 Fr or 6 Fr GCs advanced through introducer sheaths. Some have reportedly used dressings to secure the catheter at the wrist15, although this has not been performed at our centre. Excessive motion or slippage does not seem to be a major problem for most of the SH curves; however, in our experience, there is a tendency for the JR curves (for the right coronary artery) to “anticlock” out of the ostium after engagement, most likely due to reversal of stored torque. This is usually resolved by keeping a “clockwise” torque on the SH catheter until the guidewire has been advanced into the artery.
In this study, there was no significant difference in procedural success between the two groups. The procedural success rate of 95.2% in the SH group was achieved despite having more complex lesions (bifurcations and high-risk lesions) and with ACC/AHA type B2 and C lesions comprising 80% of all lesions. Although patients requiring more complex PCI, such as the kissing balloon technique or rotational atherectomy, would have been excluded from the 5 Fr group (selection bias), the clinical characteristics between the two groups were mostly similar, allowing for some comparisons to be made.
Most of the procedural failures (four of seven) in the SH group were due to extreme tortuosity of the subclavian/innominate artery with GC engagement failure, all of which occurred during the first one-third of our experience with the SH GCs. This illustrates that there is a definite learning curve with this novel GC, even for the experienced transradialists. Partly contributing to the engagement failure was also the fact that early in the experience, limited SH curves were available, particularly for the left coronary artery. As guide support is better with a 6.5 Fr system, no procedural failures in the SH group were due to inadequate support compared to the three procedural failures in the 5 Fr group.
The guide induced left main artery dissection that occurred in the SH group was likely to be due to selection of too large a curve (PB4.0 instead of PB3.5) resulting in excessive manipulation and deep intubation. There were concerns with the tip stiffness of earlier SH catheters which resulted in coronary ostia dissection; however, this issue has been resolved with more recent SH catheters15. One important aspect to note for users of the SH system is to remove or re-insert the central dilator of the SH catheter in the ascending aorta well away from the coronary ostia in order to avoid inadvertent dissection by the stiff tapered central dilator tip.
The proportion of the CTO lesions and significantly calcified lesions were similar in the two groups. The SH arm, however, had a significantly higher incidence of bifurcation and in-stent restenosis (ISR) lesions. The greater case complexities and learning curve may explain the longer procedural times and greater contrast volumes for the SH GC group. It was also likely that when 5 Fr GCs were our default guide catheters of choice in the early phase of this study, the 5 Fr GCs were not selected if the kissing balloon technique for bifurcation lesions or use of a cutting balloon was intended, and standard 6 Fr GCs were used for such cases due to the need for a larger inner lumen; hence procedural times would be expected to be shorter. This novel SH system thus allows performance of PCI that can be achieved with standard 6 Fr GCs, but without the need for a 6 Fr sheath, which has higher rates of radial artery spasm and occlusion.
Study limitations
This was a single centre retrospective study with its inherent limitations, including selection bias. The presence of radial pulse was a clinical assessment, and routine imaging for example with ultrasound, was not employed. Though accurate, we cannot rule out the possibility that in some patients with occluded radial arteries, the pulse would still be palpable due to strong collateral circulation. This possibility was however, minimised by palpating for the pulse proximal to the puncture site. The procedures were performed by interventionalists experienced with the transradial technique and results may not apply to centres or operators without such experience. Furthermore, due to the unique and unfamiliar shapes of the SH GCs for left coronary cannulation, there is a steeper learning curve as compared to using conventional GCs, which may be particularly pronounced for less experienced transradialists; thus the SH system might be better utilised by more experienced TRI operators.
Conclusion
This study was the first to evaluate the feasibility and efficacy of a novel 6.5 Fr sheathless hydrophilic coated guiding catheter as compared to the standard 5 Fr guiding catheter in TRI. Both the 6.5 Fr sheathless system and the 5 Fr guiders were shown to be effective platforms for the majority of TRI cases. The novel sheathless system however, eliminated the disadvantages of the 5 Fr GC whilst maintaining the advantage of very low radial artery spasm and occlusion rates, and may become the GC of choice in “slender” TRI.
Conflict of interest statement
The authors have no conflict of interest to declare.

