Abstract
Aims: This study retrospectively compares the in-hospital outcomes for patients undergoing high-speed rotational atherectomy (HSRA) facilitated percutaneous coronary intervention (PCI) using either the radial or the femoral artery approach.
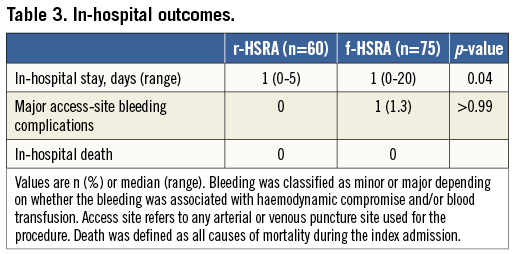
Methods and results: From September 2008 to February 2013, 135 consecutive patients (75 femoral, 60 radial) underwent HSRA in our centre. A comparison of in-hospital outcomes was performed. For the radial approach, a 7.5 Fr sheathless guiding catheter (SGC) was used. The sizing of the burrs deployed was similar (1.75 [0.75-2.00] vs. 1.75 [1.25-2.5] mm, p=0.68) with no difference in screening time (15.5 [12.2-19.5] vs. 19 [14-26] min, p=0.068), major access-site bleeding complications (0.0% vs. 1.3%, p>0.99) and procedural success (100% vs. 91%, p=0.22) in the radial and the femoral group, respectively. However, in-hospital stay [1 (0-5) vs. 1 (0-20) days, p=0.04] was slightly higher following the femoral approach. A temporary wire was placed in 10% of femoral patients. No in-hospital death was observed.
Conclusions: This study shows that the radial artery approach with the 7.5 Fr SGC is at least as safe and effective as the conventional femoral approach for performing HSRA-facilitated PCI.
Introduction
The radial artery (RA) is now the default route for vascular access in coronary angiography (CA) and percutaneous coronary intervention (PCI) because of its low rates of bleeding complications1,2 and the potential for early mobilisation3,4. High-speed rotational atherectomy (HSRA) enables treatment of heavily calcified atheroma, facilitating drug-eluting stent implantation and expansion5-7. However, the size of the RA limits the maximum dimensions of potential guide catheters to 6 Fr in most patients8. The restriction to a 6 Fr guide catheter system in turn limits the maximum size of rota burr to 1.75 mm, which can usually be delivered but will not allow sufficient contrast injection for CA. Therefore, many operators restrict their choice of rota burr to 1.25 mm when using a 6 Fr guide for safety reasons, and HSRA has continued to be performed using 7 Fr or 8 Fr guides via the femoral artery (FA).
Sheathless guiding catheter (SGC) systems allow the passage of large-bore catheters with smaller overall diameters at the arterial insertion site, as there is no need for a sheath9. These guides have an external diameter smaller than a sheath used for a 6 Fr guide catheter (2.49 mm vs. 2.70 mm, respectively) but a significantly larger internal lumen (2.06 mm vs. 1.78 mm, respectively). Using the 7.5 Fr, SGC system, complex PCI can be performed9,10. However, there are only limited data in small non-consecutive series of its use in HSRA11-14.
Avoiding femoral artery puncture in favour of the radial approach in patients known to have calcific coronary disease is a logical ideal but there are potential concerns over whether this is practical and realistic in these complex patient subsets that are likely to have tortuous rigid subclavian anatomies. In this study we sought to compare the in-hospital outcomes of patients undergoing HSRA-facilitated revascularisation deployed via either the radial or the femoral route.
Methods
STUDY POPULATION
From September 2008 to February 2013, 135 consecutive patients (75 femoral, 60 radial) who underwent HSRA in our centre were studied. The procedures were performed by operators fully trained in rotablation technique and with several years of interventional experience. Both elective and emergency cases were included. Patients who required primary PCI were excluded. A retrospective comparison of in-hospital outcomes has been performed.
PROCEDURE
ANTIPLATELET AND ANTICOAGULATION THERAPY
All patients in this study were preloaded with dual antiplatelet therapy and all received intravenous unfractionated heparin (70-100 U/kg). For procedures lasting longer than one hour, activated clotting time was measured, aiming for a target >300 s unless abciximab had been used. Use of the glycoprotein IIb/IIIa inhibitor abciximab or bivalirudin was determined by the operator.
GUIDING CATHETERS AND ADJUNCTIVE DEVICES
CA was performed according to the conventional approach. The decision to perform HSRA-PCI was taken at the operator’s discretion, following prior visualisation of a heavily calcified coronary lesion or failure to cross/dilate the lesion with a balloon catheter. In cases where HSRA was performed ad hoc following a diagnostic CA, the access site was not changed.
The 7.5 Fr SGC Eaucath (ASAHI Eaucath SGC; Vascular Perspectives Ltd., Manchester, UK) was the default strategy for all transradial procedures, whereas an 8 Fr GC was used in the femoral approach group. HSRA was performed using the Rotablator® rotational atherectomy system (Boston Scientific, Natick, MA, USA). The burr size was selected to reach a burr/vessel ratio approaching 0.5 with an intention to use only a single burr to ablate plaque and facilitate the passage of further devices. HSRA speed ranged between 140,000 and 180,000 rotations per minute. In our centre, HSRA is usually performed in conjunction with an intracoronary infusion of a “cocktail” containing verapamil, heparin, and nitroglycerine with burr runs <20 seconds in duration in order to avoid burr deceleration. The appropriate stent length for the target lesion was ≥4 mm longer than the lesion length to allow for coverage between healthy vessel segments, with adequate stent overlapping. Post-dilation was performed at the discretion of the treating physician. Elective temporary right ventricle (RV) pacing using the right femoral vein was performed in a limited number of right coronary cases.
In the radial group, the GC were removed immediately after the interventional procedures and haemostasis was obtained using an inflatable wrist band (TR-Band™; Terumo Corporation, Tokyo, Japan), whereas for femoral procedures haemostasis was achieved using a femoral artery closure device (Angio-Seal™ VIP; St. Jude Medical, St. Paul, MN, USA). Other adjuvant devices (e.g., intravascular ultrasound guidance, optical coherence tomography, pressure wires, distal filters) as well as stent implantation techniques and types, were left to the operator’s discretion. All patients provided written informed consent to the procedure and for their data to be analysed.
THE SHEATHLESS EAUCATH GUIDING CATHETER SYSTEM
The 7.5 Fr SGC Eaucath has no introducer sheath and its outer diameter (OD) is 2.49 mm smaller than the 2.70 mm of the 6 Fr introducer sheath. It provides an inner lumen of 0.081 inches and enables the performance of HSRA with burrs measuring 2 mm or less. In contrast to standard catheters that have a single layer of metallic braiding, the wall of this catheter is thicker, as it has an additional layer of braiding, which provides optimal torqueability and flexibility, and an outer hydrophilic coating present along the entire length of the GC9, which facilitates its smooth passage and reduces radial pain and spasm during catheter manipulation15,16.
As previously described17, catheter insertion involves initial radial cannulation using a standard 6 Fr sheath (Radifocus®; Terumo Medical Corp., Piscataway, NJ, USA) that is used to insert a standard J-tipped 150 cm 0.035 inch diameter exchange wire (Terumo Corp.). Normal saline (10 mL) with 250 μg of nitroglycerine was injected into the RA through the introducer sheath to prevent RA spasm18. The sheath was then exchanged for the SGC over the standard 150 cm J-tipped 0.035 inch wire. The type of SGC was selected at the operator’s discretion. The SGC was composed of two parts, a hydrophilic catheter and a central dilator9. The central dilator was inserted into the catheter and locked in place. The SGC with the central dilator was advanced along the 0.035 inch wire to the proximal ascending thoracic aorta. The central dilator and 0.035 inch wire were then removed. The ostium of the selected coronary artery was engaged by the GC and PCI was performed. The SGC has a slightly translucent tip and care is necessary with initial manipulation, particularly when left main (LM) disease has been documented. Occasionally, with this SGC design –especially the PB and SPB shapes– the initial engagement can be problematic and the guide can dislodge, pulling the guidewire out during deep inspiration. The risk of this may be diminished by waiting at least three or four minutes with the white introducer sheath inside the catheter prior to its introduction into the patient.
During the period of the study our routine practice evolved to use a conventional guidewire to cross the calcified lesion initially rather than attempt crossing with the rotawire. This initial wire is then exchanged using either an OTW balloon or dedicated CTO device. After successful rotablation the lesion is usually recrossed with a conventional wire and the rotawire left in place to confirm successful balloon expansion and then act as a “buddy wire” to facilitate initial stent placement.
STUDY DEFINITIONS AND ENDPOINTS
Procedural success was defined as the successful implantation of stent(s) with final Thrombolysis In Myocardial Infarction (TIMI) flow grade 3 and reduction of the lesion to <30% luminal diameter by visual angiographic assessment in the absence of complications despite the selection of the GC. Bleeding was classified as minor or major depending on whether the bleeding was associated with haemodynamic compromise and/or blood transfusion. Access site refers to any successful arterial or venous puncture site used for the procedure. Death was defined as all causes of mortality during the index admission. Dissections of coronary artery and aorta were defined as a disruption of an arterial wall resulting in splitting and separation of the intimal layers evaluated by CA during the procedure. Pseudoaneurysm was defined as the occurrence of a disruption and dilation of the arterial wall without identification of the arterial wall layers at the site of the catheter entry as demonstrated by arteriography or ultrasound. Arteriovenous fistula was defined as a connection between the access artery and the accompanying vein that was demonstrated by arteriography or ultrasound. RA occlusion was defined as absence of an RA pulse by clinical assessment. Stent thrombosis was defined as an acute coronary syndrome (ACS) with angiographic evidence of stent occlusion.
STATISTICAL ANALYSIS
Statistical analysis was performed using SPSS version 14.0 (SPSS Inc., Chicago, IL, USA). Data are expressed as mean±SD for continuous variables or as median (25th-75th percentile) or median (range) for non-continuous variables, and as absolute number and percentages for categorical variables.
Continuous variables which were normally distributed (after being checked using the Kolgomorov test) were compared using the Student’s t-test, while non-normally distributed variables were compared using the Mann-Whitney test.
Categorical variables were compared using χ2 test or Fisher’s exact test (if the expected number of patients was less than five). A p-value ≤0.05 was considered to indicate statistical significance.
Results
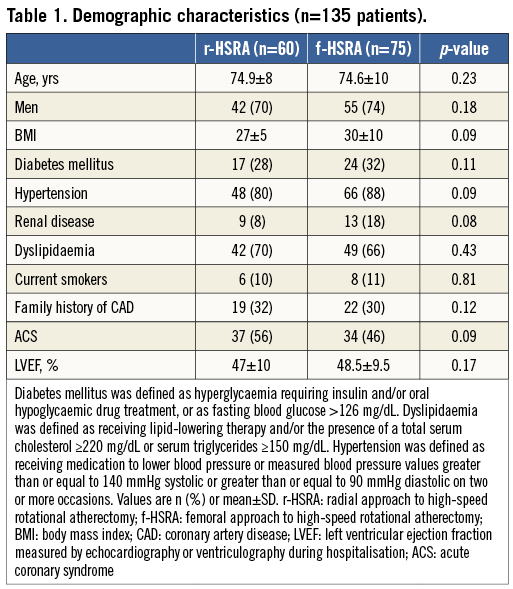
DEMOGRAPHIC CHARACTERISTICS
A total of 135 consecutive patients (75 femoral, 60 radial) who underwent HSRA were studied, which represents 1.8% of the 7,580 PCIs performed during the period of the study. Demographic characteristics are shown in Table 1. The patients in each group were well matched in terms of clinical characteristics. The majority of cases involved men and the mean age was nearly 75 years in both groups. Approximately half of the patients had an ACS in both radial and femoral groups.
TRENDS OF HSRA-FACILITATED AND NON-HSRA-FACILITATED PCIS VIA THE FEMORAL AND RADIAL ROUTES
From December 2011 there was a temporal trend at our institution for RA access to become the default approach for diagnostic CA and PCI during the course of the study period, whereas FA access was reserved for extremely small RA before the procedure (Figure 1).
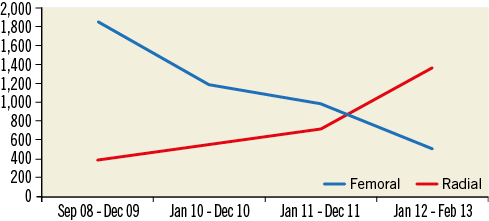
Figure 1. Non-rotablation PCIs via the femoral and radial routes over the last four and a half years. From December 2011 there was a temporal trend at our institution for RA access to become the default route for PCIs. During the latter period, femoral artery access was reserved only for failed RA access or palpation of an excessively small RA before the procedure.
In the HSRA group, during the first two years, we performed four transradial versus 49 transfemoral procedures, in the next two years 29 transradial versus 26 transfemoral procedures, and in the last six months all 27 procedures were performed via the radial approach (Figure 2).
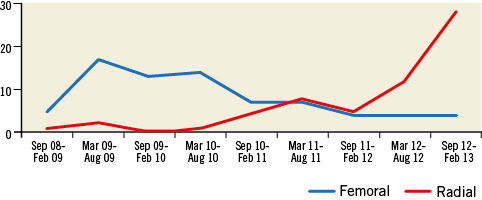
Figure 2. Trend in the use of HSRA via the femoral and radial routes over the last four and a half years in the overall data set. From October 2012 there was a temporal trend at our institution for RA access to become the default route for HSRA-facilitated PCI. During the latter period, femoral artery access was reserved only for failed RA access or palpation of an excessively small RA before the procedure.
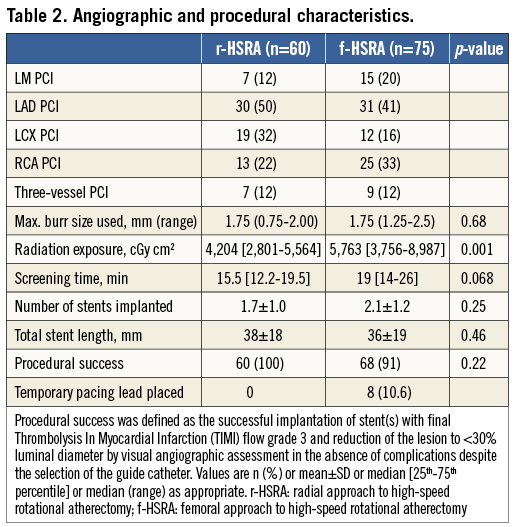
ANGIOGRAPHIC AND PROCEDURAL CHARACTERISTICS
Angiographic and procedural characteristics are shown in Table 2. There was a slightly higher prevalence of protected LM PCI in the femoral compared with the radial group (20% vs. 12%), whereas three-vessel PCI was well matched in both groups (12%). Burrs (1.75 [0.75-2.00] vs. 1.75 [1.25-2.5] mm, p=0.68) with one burr/procedure, screening time (15.5 [12.2-19.5] vs. 19 [14-26] min, p=0.068), total stent length (38±18 mm vs. 36±19 mm, p=0.46) and procedural success (100% vs. 91%, p=0.22) were similar in radial and femoral groups, respectively. The failed cases (n=7) following femoral approach were due to incomplete stenting of the target lesion (n=6) and failure to pass the rotawire (n=1): this case was successfully treated with rotablation five days later. Patient radiation exposure (PRE) (5,763 [3,756-8,987] vs. 4,204 [2,801-5,564] cGy cm2, p=0,001) was greater in the femoral than in the radial group, whereas a temporary transvenous pacing wire was placed only in the femoral group in 10% of patients.
IN-HOSPITAL OUTCOMES
In-hospital outcomes are shown in Table 3. Major access-site bleeding complications (0.0% vs. 1.3%, p>0.99) were similar in both groups, whereas in-hospital stay (1 [0-20] vs. 1 [0-5] days, p=0.04)was slightly increased in the femoral compared to the radial group. Finally, the incidence of in-hospital death was zero in both groups.
Discussion
This study demonstrates that RA access is a feasible, safe and effective way to perform HSRA for the treatment of heavily calcified coronary lesions. Use of an SGC allows the operator to have the advantages of the radial approach and still deploy burrs up to 2 mm in diameter without compromising procedural imaging and safety. We also demonstrated that, in this small series, radial HSRA is associated with a significantly reduced in-hospital stay compared to transfemoral access.
We have confirmed the feasibility of using transradial access for HSRA demonstrated in the only other published series19. We have also demonstrated a low access-site complication rate, and fewer bleeding complications compared with femoral access, as observed in other PCI settings20.
Procedural radiation exposure was significantly lower in the radial group and there was no increase in screening time during radial cases in this study despite the slightly increased complexity of using the SGC. There is no clear indication from our data to suggest that our patients treated using the radial approach had less severe disease than those treated with the femoral approach, as there were similar numbers of LAD, three-vessel and LM PCIs in both groups. These findings are comparable to the findings reported by Kuipers21 and Geijer22, where they reported that the procedural radiation exposure for those undergoing complex PCIs did not increase when using the radial access route. Similar results have recently been presented by a substudy of the RIVAL trial where high-volume centres have the lowest radiation dose irrespective of which access-site approach they use23. The procedures in the present study were performed at a high-volume centre by interventional cardiologists with extensive experience in performing procedures by both radial and femoral routes.
We demonstrated that femoral patients in this series had a trend towards higher BMI, and this may account for some of the differences in radiation exposure. However, as the series was consecutive, we also recognise that there is a continued learning curve for the rotablation procedure itself. The decision to exchange wires rather than use the rotawire initially together with other evolutions in our technique may magnify potential differences which are not truly attributable to the route of vascular access.
Therefore, whilst recognising that our results can only be applied to centres where procedures are performed by interventional cardiologists with sufficient experience, we can suggest that there appears to be no procedural disadvantage to the radial approach. It is not known to what extent the results can be applied to other centres where the radial route is used as a complementary technique to the femoral route, and where cardiologists are less experienced in performing procedures by the radial route24.
This study also confirms that changes in contemporary interventional practice, such as shorter burr runs and limited speeds, mean that slow flow and consequently life-threatening bradycardia are very unusual. Avoiding the use of a temporary RV wire reduces screening time and avoids the risks of right ventricular perforation and tamponade. It is now our policy to ensure we have atropine immediately available and an emergency transcutaneous pacing system on standby.
Limitations
Because of the retrospective nature of the study, small differences may exist between groups, which may affect the success of each approach if examined in a prospective randomised manner. The relatively small numbers in this study will have resulted in reduced power to detect significant differences.
We did not directly measure operator exposure but, as there is a linear relationship between patient and operator exposure, we are confident that the use of the transradial route did not increase operator exposure.
Conclusion
In summary, we have shown that RA access with the 7.5 Fr SGC is an extremely useful alternative to FA access for HSRA. In our opinion it should definitely be the default strategy in PCI centres with radial expertise, as this approach is associated with good procedural success, a low rate of complications and a reduced in-hospital stay.
| Impact on daily practice This study illustrates the use of RA access with the 7.5 Fr SGC as being an extremely useful alternative to femoral access for HSRA-PCI in complex calcified coronary lesions allowing stent delivery and complete expansion. |
Conflict of interest statement
A. Banning is partially funded by the NIHR Oxford Comprehensive Biomedical Research Centre and has received unrestricted research funding from Boston Scientific Corporation. The other authors have no conflicts of interest to declare.

