Introduction
Recent studies have reported a high rate of transradial access (TRA)-induced vascular injury which leads to chronic intimal thickening and is associated with radial artery spasm (RAS) and radial artery occlusion (RAO)1,2,3. This is likely to be caused by radial artery puncture, sheath introduction and sheath friction caused by radial artery inner diameter-sheath outer diameter (RAID/SOD) mismatch. However, using optical coherence tomography (OCT), post-procedural radial artery (RA) damage was also found in the proximal part of the RA, where the vessel has a larger diameter and RAID/SOD mismatch is less likely to be the cause of vascular damage. One of the possible mechanisms is intimal damage caused by the space between the guidewire and the catheter tip which shaves the vessel wall (“razor” effect) (Figure 1),4.
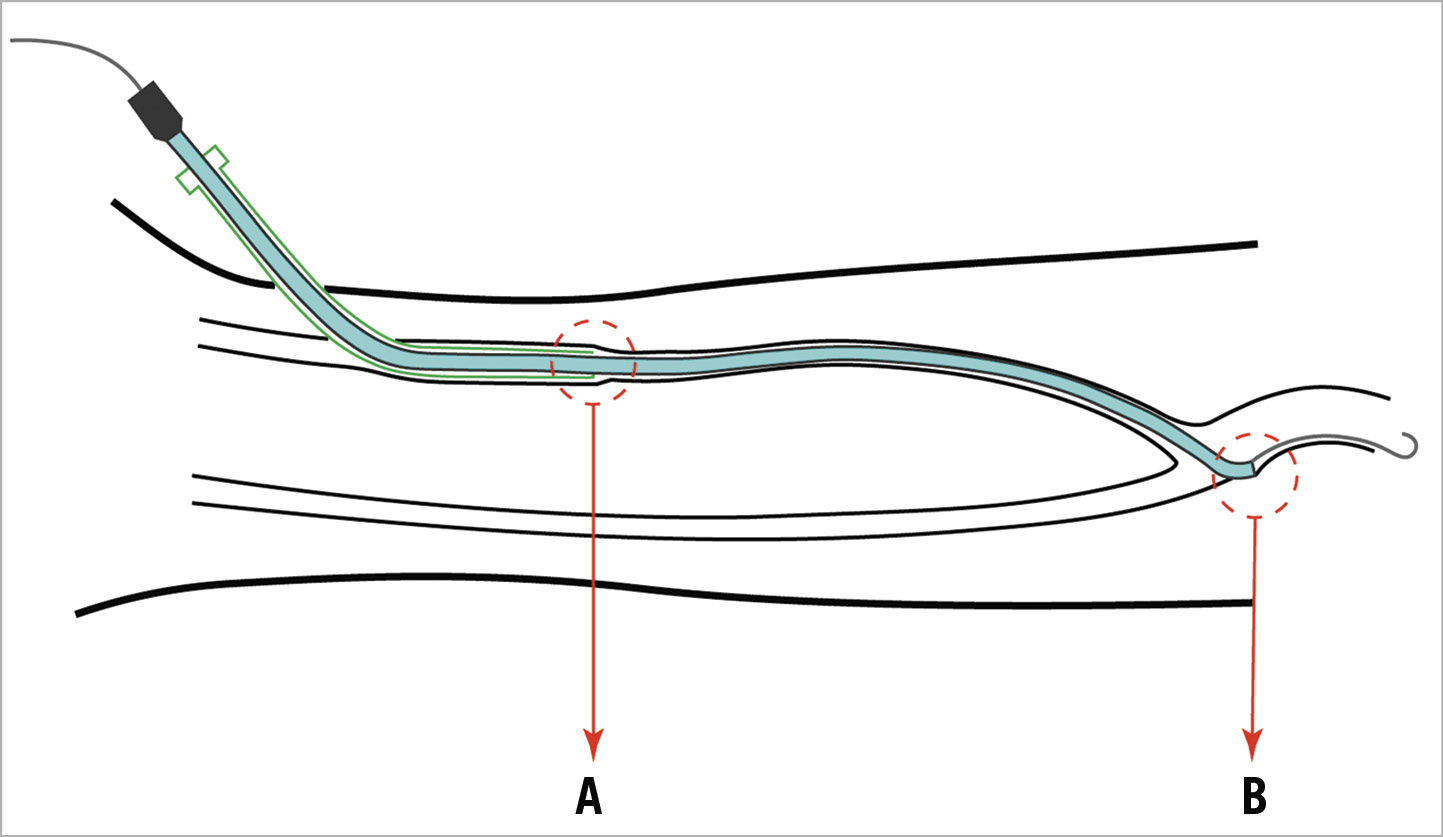
Figure 1. Mechanisms of radial artery injury caused by the transradial access. A) Oversized sheath outer diameter (SOD) compared to the radial artery internal diameter (RAID). B) Razor effect of the catheter tip edge. Green represents the sheath outer layer, light blue the guiding catheter and the grey line the guidewire.
A sheathless catheter introduction system may reduce both RAID/SOD mismatch and the razor effect by a smooth wire-to-catheter transition. To evaluate these two potential effects, we designed a trial to measure intimal and medial radial artery injury, comparing sheathless TRA (SLTRA) with the RAILWAY™ Sheathless Access System (Cordis, Cardinal Health, Milpitas, CA, USA) to conventional TRA (CTRA).
Methods
Details regarding the procedures, data collection and definitions are available in Supplementary Appendix 1 and Supplementary Figure 1-Supplementary Figure 3.
Results
A total of 597 patients were screened for the trial (Supplementary Figure 1), of whom 51 were enrolled. Two patients did not undergo OCT; one OCT was not analysable. The main reason not to include patients was logistic, and a maximum of one patient per day was enrolled due to time constraints in the cath lab. Baseline and procedural results are presented in Supplementary Table 1 and Supplementary Table 2.
ENDPOINTS
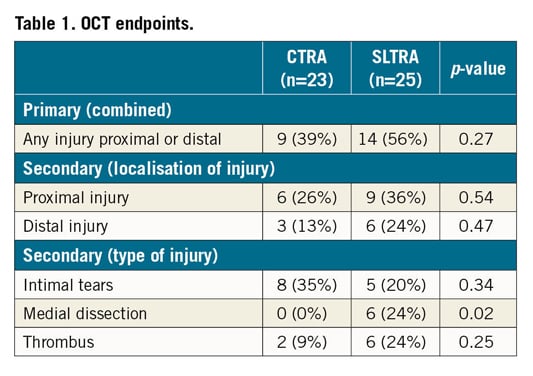
The occurrence of the predefined composite primary endpoint did not differ significantly between the CTRA and SLTRA groups (9 [35%] vs 14 [56%], respectively, p=0.27) (Table 1). The interobserver agreement of the primary endpoint was low (kappa 0.45), mainly driven by the component intimal tears (kappa 0.30). The agreement of the other endpoints medial dissection and thrombus was substantial (kappa 0.73 and 0.83, respectively). Secondary endpoints are shown in Supplementary Table 3.
Discussion
No reduction in vascular injury of the radial artery was shown using the RAILWAY Sheathless TRA System. Also, no reduction in other predefined endpoints was seen.
The frequency of vascular damage in the control group of our trial was in line with the results of two recent OCT studies3,5. In other trials, sheathless access reduced RAS6, probably as a result of a more favourable RAID/SOD ratio7. Although RAID/SOD mismatch was not present in our SLTRA group, there was no protective effect on distal or proximal RA injury measured by OCT. There were more medial dissections in the SLTRA group. Forward movements of the RAILWAY dilator system may induce medial damage during introduction of the guiding catheter (GC). Another cause may be the introduction of normal instead of hydrophilic coated GCs, as used in other SLTRA systems.
Contrary to other studies3,5, we found a low interobserver agreement when evaluating intimal tears (IT). OCT imaging of the intima is prone to false images, for example by suboptimal blood clearance. On the other hand, medial dissections and intraluminal thrombi are easily visible with OCT.
Our findings may have important consequences for the use of SLTRA in daily practice. SLTRA is feasible as an alternative access strategy and its procedural success rate is comparable to CTRA8,9. On the other hand, in our cohort the technique did not seem to reduce vascular damage. Therefore, SLTRA may not be appropriate as a standard access technique to prevent vascular injury, but it may be beneficial in selected patients, for example patients scheduled for procedures mandating large bore catheters or for populations with small radial arteries.
Limitations
One limitation of the trial is the lack of historical OCT data in patients undergoing SLTRA. Also, for logistic reasons, one patient a day was included, which might have introduced selection bias, although we have no data about the reasons for excluding patients. In addition, the study was not powered to detect any clinical endpoint. Moreover, the relationship between OCT-detected injury and clinical outcome is not known.
Conclusion
SLTRA is not related to reduced vascular injury when compared to CTRA, as evaluated by OCT imaging.
|
Impact on daily practice No preventive effect of the RAILWAY Sheathless Access System on radial artery injury was seen in this study. Adoption of a sheathless technique as a standard procedure for 6 Fr TRA does not seem appropriate. |
Funding
Research Foundation Bronovo Hospital, The Hague, the Netherlands.
Conflict of interest statement
R.J. van Geuns reports grants and personal fees from Abbott Vascular, outside the submitted work. N. van Royen reports grants from Abbott, Philips, and AstraZeneca, personal fees from Castor, Medtronic, Bayer, and Boston, and grants from Biotronik, outside the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.