Abstract
Aims: The aim of this study was to compare the performance of the Tiger-II with Judkins 3.5L/4R catheters in coronary angiography (CAG) via the transradial approach (TRA).
Methods and results: Consecutive patients undergoing non-urgent CAG via the right TRA were randomised to either the Tiger-II (Terumo) or Judkins (3.5L/4R; Medtronic) 5 Fr catheters; 320 patients in each group were randomised. Catheter or access site change was required in 57 (17.8%) vs. 68 (21.3%) patients allocated to the Tiger-II and Judkins group, respectively (p=0.3). The study’s primary endpoint of contrast volume (ml) used until completion of CAG was lower for Tiger-II vs. Judkins group: 66.8 (54.0-82.0) vs. 73.4 (60.0-94.1), p<0.001. Angiography, fluoroscopy time (min) and severe spasm rate were also significantly lower for Tiger-II vs. Judkins group: 5.52 (4.17-7.32) vs. 6.85 (5.15-9.63), p<0.00, 2.01 (1.32-3.13) vs. 2.24 (1.50-3.50), p=0.01 and 6 (2.8%) vs. 39 (12.2%), p<0.001, respectively. The Tiger-II catheter obtained better opacification grade for the right coronary artery (RCA): 4.0 (4.0-4.0) vs. 4.0 (3.0-4.0), p=0.02, but slightly compromised opacification of the left anterior descending (LAD) and left circumflex (LCX) arteries compared with the Judkins group: 3.75 (3.0-4.0) vs. 4.0 (3.5-4.0), p<0.001, and 3.78 (3.6-4.0) vs. 4.0 (3.6-4.0), p<0.001, respectively.
Conclusions: The Tiger-II was found superior to the Judkins 3.5L/4R regarding contrast volume use, procedural and fluoroscopy time, spasm rate and RCA imaging, and inferior regarding LAD and LCX imaging. ClinicalTrials.gov Identifier: NCT03042845
Abbreviations
ACS: acute coronary syndrome
CAG: coronary angiography
ITT: intention-to-treat
LAD: left anterior descending artery
LCX: left circumflex artery
mITT: modified intention-to-treat
PCI: percutaneous coronary intervention
PP: per protocol
RCA: right coronary artery
TRA: transradial approach
Introduction
Carrying out diagnostic coronary angiography (CAG) via the right radial artery is now common practice1-5. The transradial approach (TRA) exhibits clinical benefit in terms of safety and efficacy over transfemoral access, as it has been shown to reduce mortality, major adverse cardiovascular events and major bleeding in patients with acute coronary syndrome (ACS) undergoing percutaneous coronary intervention (PCI)6,7.
Judkins catheters – initially designed for coronary catheterisation via the femoral artery – and the Tiger catheter – designed for transradial use – are in descending order the most frequently used catheters for TRA worldwide8, but no specific recommendation on catheter selection is given and their use remains at the operator’s discretion9.
Evidence on the comparative performance of the left/right Judkins and Tiger catheters in patients undergoing diagnostic CAG via the right radial artery is scarce. In a retrospective study of 273 patients, the Tiger catheter has been associated with higher contrast volume, fluoroscopy time and need for catheter change compared to the Judkins catheters10. Kim et al performed the first randomised comparison between these catheters in 160 patients showing shorter fluoroscopy time with Tiger use, with only a pre-specified number of angiographic views being taken into account11. In a more recent randomised study by Chen et al involving 110 patients, the Tiger catheter resulted in a shorter fluoroscopy time and no difference in contrast volume used compared with Judkins catheters, with endpoints being measured up to the need for catheter change12. However, both these randomised studies were limited by a relatively small sample size and the lack of an intention-to-treat design.
The purpose of this study was to compare the use of Tiger vs. Judkins catheters as a default strategy in patients undergoing non-urgent CAG through the TRA. The use of a catheter demonstrating superiority in terms of contrast volume used, temporal and radiative features, would be beneficial, especially in high-volume catheterisation laboratories.
Methods
This was a prospective, two-centre, randomised study of parallel design, designed to assess the performance of the Tiger-II (5 Fr; Terumo Interventional Systems, Somerset, NJ, USA) vs. Judkins (5 Fr, 3.5L/4R; Medtronic, Minneapolis, MN, USA) in CAG via the right TRA.
Consecutive patients undergoing non-urgent CAG were randomised after successful cannulation of the right radial artery in a 1:1 ratio to the use of either left/right Judkins (JL3.5/JR4) catheters or the Tiger-II catheter. Computer-generated random numbers were used for randomisation, stratified by centre. Participating centres used the right TRA as a default strategy and all operators were either highly experienced (>1,000 angiograms overall) or qualified (≥80 procedures a year) in TRA and in the use of both Judkins and Tiger-II catheters5,9. All patients received 50 IU/kg or a 5,000 IU bolus of heparin and 200 μg of nitroglycerine intra-arterially.
Patients were excluded if they presented with an indication for urgent CAG (ST-elevation myocardial infarction or non-ST-elevation myocardial infarction with an indication for CAG within two hours), haemodynamic instability, non-palpable right coronary artery, negative Allen test, prior coronary artery bypass grafting, dialysis or known severe renal impairment (creatinine clearance <30 ml/min). Patients were also excluded in case of non-availability of either study catheter or qualified operator as previously described.
Operators were encouraged to obtain at least four standard views to image the left coronary artery (LCA) and two standard views for the right coronary artery (RCA); however, the final number of views was at the operator’s discretion. Angiographic image quality was assessed by offline review of all angiograms – loaded to RadiAnt DICOM viewer, version 3.4.2.13370 (Medixant, Poznan, Poland) by two experienced operators (I.X. and P.D.).
ENDPOINTS
The primary objective of the study was to investigate the hypothesis of the superiority of the Tiger-II catheter vs. Judkins 3.5L/4R catheters in terms of contrast volume used (including leftover contrast) for completion of CAG. The study’s primary endpoint was contrast volume (in ml) used until completion of CAG in an intention-to-treat (ITT) analysis.
The study’s secondary endpoints were duration of CAG (min), fluoroscopy time (min) and dose area product (DAP: cGy*cm2) between groups. Other study endpoints involved coronary opacification, catheter contact with the coronary ostium, catheter stability within coronary ostium scores and excessive ostium engagement between groups.
All endpoints were measured from the entrance of the first angiographic catheter into the sheath to the removal of the last angiographic catheter from the sheath upon completion of the diagnostic CAG. Primary analysis was based on the ITT principle: assessment was continued in case of need for catheter or access site change until CAG completion. A per-protocol (PP) analysis (assessment only in cases without catheter failure) was also performed. When the decision was made to perform left ventriculography, aortography or other diagnostic assessment or to proceed to ad hoc PCI, the study was stopped and the outcomes were measured only up to that point.
In angiographic image quality analyses, all angiographic views were evaluated and mean scores were calculated for each case. Results are presented by ITT and PP analysis. A modified ITT (mITT) analysis was also used to express catheter failure: angiographic views until coronary angiogram completion were assessed excluding views not obtained by the right TRA and the originally allocated catheter. (Figure 1).
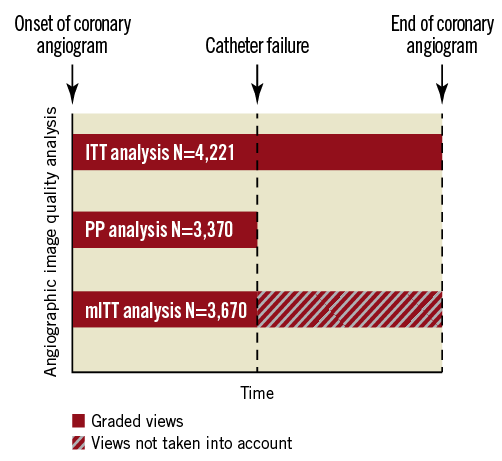
Figure 1. Angiographic image quality analysis description in case of catheter failure. ITT: intention-to-treat; mITT: modified intention-to-treat; PP: per-protocol
DEFINITIONS
Catheter failure was defined as the need for study catheter change and/or access site change for completion of CAG. Spasm was graded as mild (causing well tolerated local pain), moderate (severe pain but the handling of catheters remains satisfactory) or severe (leading to catheter failure). Details on angiographic image quality grading are provided in the Supplementary Appendix. Angiography time was defined as the interval from the insertion of the first diagnostic coronary catheter in the sheath until the exit of the last diagnostic catheter from the sheath. Fluoroscopy time was defined as the cumulative duration of fluoroscopy during angiography time.
SAMPLE SIZE CALCULATION
Based on published data12, we hypothesised that Tiger catheter use would lead to an absolute decrease of at least 5 ml in contrast volume use compared with Judkins catheters (48 and 53 ml for Tiger and Judkins catheters, respectively, with estimated standard deviation of 17 for both). With a two-sided alpha of 0.05, group sample sizes of at least 316 and 316 patients would achieve 95% power to detect this difference.
STATISTICAL ANALYSIS
Categorical data (compared with Fisher’s exact test) are presented as frequencies and group percentages. Continuous data with normal distribution (compared with the Student’s t-test) are presented as means±standard deviation (SD). Continuous data with skewed distribution are presented as medians (first to third quartile) and compared with the Mann-Whitney U test. The Kolmogorov-Smirnov test was used to assess data normality. Inter-observer and intra-observer agreement was performed by calculating an intraclass correlation coefficient (ICC) using a two-way mixed-effects model for absolute agreement, in 40 randomly selected cases. All tests were two-tailed and statistical significance was considered for p-values <0.05. Analyses were performed using SPSS for Windows, Version 16.0 (SPSS Inc., Chicago, IL, USA) and GraphPad Prism v.5 (GraphPad Software, Inc., La Jolla, CA, USA).
The study was conducted according to the Declaration of Helsinki. All patients participating in the study gave written informed consent. The study was approved by the authorised local ethics committee in clinical research. The study is registered on ClinicalTrials.gov (NCT03042845).
Results
Between October 2016 and May 2017, 320 and 320 patients were randomised to the Tiger and Judkins groups, respectively (Figure 2). Patients’ demographic and clinical characteristics (Table 1) did not differ significantly between groups.

Figure 2. Study flow chart. CABG: coronary artery bypass grafting; ITT: intention-to-treat; PCI: percutaneous coronary intervention; PP: per-protocol

There were no procedural complications in either group. The overall observed catheter failure rate was 19.5% and did not differ significantly between groups (p=0.3) (Table 2). Reasons for catheter failure in descending order were severe spasm (36.8%), right subclavian/aortic arch tortuosity (31.2%), radial/brachial tortuosity (25.6%) and coronary anatomy (6.4%). Spasm was more frequently observed in the Judkins vs. the Tiger group (p for trend <0.001).

The study’s primary endpoint of contrast volume (ml) was lower for the Tiger vs. the Judkins group: 66.8 (54.0-82.0) vs. 73.4 (60.0-94.1), p<0.001 (Table 3, Figure 3). Angiography and fluoroscopy time (min) were also significantly lower for the Tiger vs. the Judkins group: 5.52 (4.17-7.32) vs. 6.85 (5.15-9.63), p<0.001, and 2.01 (1.32-3.13) vs. 2.24 (1.50-3.50), p=0.01, respectively, while DAP did not differ significantly between groups. In PP analysis, differences in contrast volume and angiography time remained statistically significant between groups in favour of the Tiger catheter (Table 3, Figure 3).

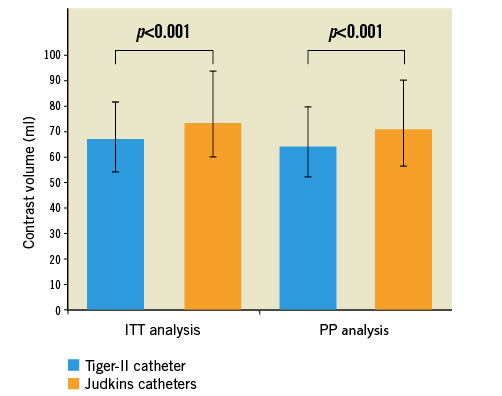
Figure 3. Contrast volume (ml) between Tiger-II and Judkins catheters in the ITT and PP population. Bars represent median and error bars interquartile range. ITT: intention-to-treat; PP: per-protocol
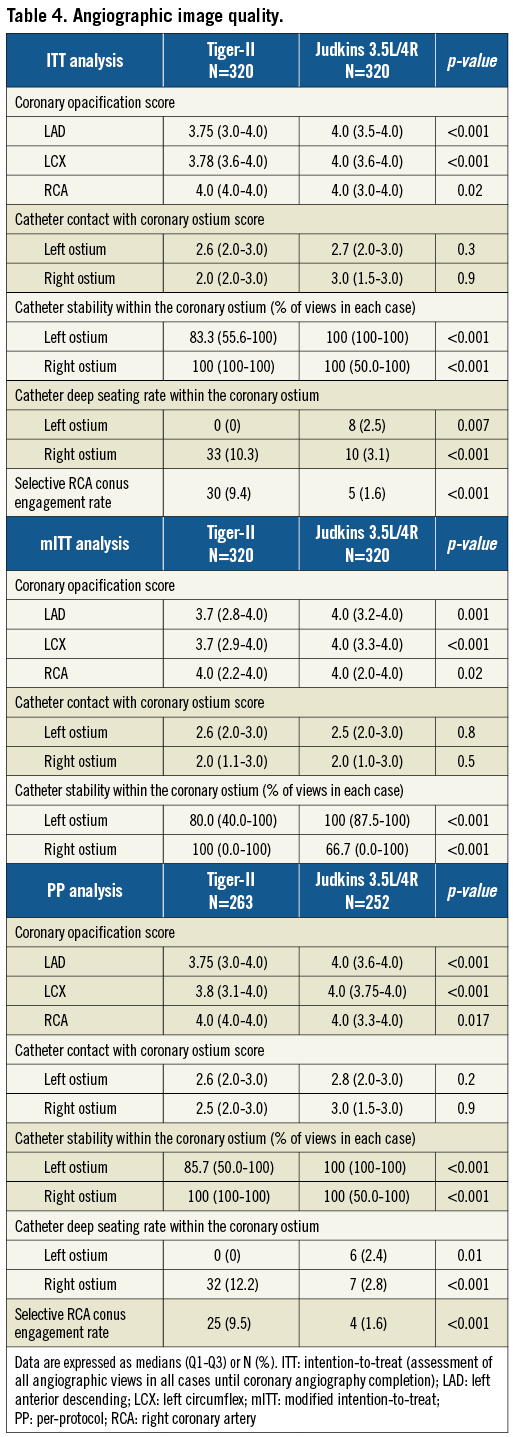
High inter- and intra-observer agreement was observed for opacification, catheter contact and catheter stability grading (Supplementary Table 1). In the ITT, mITT and PP analyses, Judkins catheters obtained a higher opacification score for the LCA compared with the Tiger catheter, with the latter achieving better opacification for the RCA (Table 4). Additionally, higher stability rates were obtained by Judkins and Tiger catheters within the left and right ostium, respectively, in all analyses. Catheter contact scores with either coronary ostium did not differ significantly between groups. However, coaxial contact in all angiographic views within the left ostium did not differ significantly between the Tiger-II and Judkins catheters (43.8% vs. 45.9%, p=0.6), but there was a tendency towards less frequent coaxial contact with the right ostium with the Tiger-II catheter (46.6% vs. 54.4%, p=0.058). Moreover, the rate of excessive engagement within the left and right coronary ostia was higher for the Judkins 3.5L and Tiger-II catheter (0.0% vs. 2.5%, p=0.007, and 10.3% vs. 3.1%, p<0.001), respectively, while selective RCA conus engagement was more frequently observed with the Tiger-II catheter (9.4% vs. 1.6%, p<0.001). The same pattern of results was observed in our PP population.
Discussion
Our results confirmed the study’s primary hypothesis of superiority of the Tiger catheter as a default strategy compared with Judkins catheters, with respect to contrast volume used. Tiger catheter use has been associated with a relative reduction of 9% in median contrast volume. The observed decrease was consistent in the “ideal” subgroup of patients without need for catheter and/or access site change. Reduction in contrast volume may be of particular importance in high-volume catheterisation laboratories, leading to significant cost savings. Chen et al first compared contrast volume used for transradial CAG between Tiger and Judkins catheters; although there was a slight trend towards lower contrast volume with Tiger catheter use, the difference was not proven significant, probably due to smaller sample size12. In a retrospective analysis, the Tiger catheter was associated with higher contrast volume use compared with Judkins catheters; however, the study was by design prone to selection biases and no statistical adjustment was used10.
We also found that Tiger use was associated with significantly shorter angiography time compared with Judkins catheters, in both ITT and PP analyses, in accordance with Kim et al11. This could probably result in time saving and cost containment. Tiger use was associated with a 19.4% relative reduction in median procedural duration. In addition, procedural duration has been reported as an independent predictor of radial artery occlusion (RAO)13,14. Therefore, it could be hypothesised that Tiger use might have a beneficial effect on the RAO rate via shortening procedural length.
The Tiger catheter, in accordance with previous studies, has also been associated with shorter fluoroscopy time compared with Judkins catheters11,12. Decreased fluoroscopy time may be of particular importance to high-volume operators performing multiple procedures per day. In our study, Tiger catheter use resulted in a relative reduction in median fluoroscopy time of 10.3% compared with Judkins catheters. Radiation dose as measured by DAP did not differ significantly between groups, a finding explained by the fact that DAP is largely dependent on cine-angiography time (being predominantly affected by the number of angiographic views acquired, which did not differ between groups) and to a much smaller extent on fluoroscopy time15.
The overall catheter failure rate was 19.5% and it did not differ significantly between groups. Kim et al also reported a similar catheter failure rate between Tiger and Judkins catheters, although overall it was lower (8.1%) compared with our results11. Our study’s catheter failure rate may reflect everyday clinical practice in high-volume centres, where each procedure needs to be completed within a certain time frame and therefore catheter change could be more easily decided, while Langer et al in a single-arm observational study reported a 33.2% catheter failure rate with Tiger catheter use among experienced radialists16.
Spasm was less frequent in the Tiger group, potentially due to less need for catheter exchange compared with the Judkins group, which underlines the importance of the one-catheter concept in reducing arterial irritation and injury. Among previous randomised studies, Chen et al reported an overall 5.5% severe spasm rate, which – in contrast to our results – did not differ significantly between groups, while Kim et al demonstrated that patients in the Judkins group experienced more pain11,12. In accordance with our results, Turan et al and Erden et al in randomised comparisons between a single-catheter approach (Judkins 3.5L and reshaped Jacky catheter [Terumo], respectively) and a two-catheter approach (Judkins 3.5L/4R), in patients undergoing CAG through the TRA, reported a higher spasm rate in the two-catheter groups (22.3 vs. 12.6%, p=0.067, and 21.7% vs. 11.3%, p=0.005, respectively)17,18.
We found that in all analyses Judkins catheters resulted in better angiographic opacification of the LCA while Tiger achieved superior opacification of the RCA. In the study by Kim et al, Tiger catheter use also led to a higher angiographic score for the RCA, but no significant difference emerged for the LCA between the two groups, which could be attributed to a smaller sample size compared with our study11.
Differences in opacification were mainly driven by corresponding better stability rates within the left main and right coronary ostia observed in all analyses (ITT, mITT and PP) with Judkins and Tiger catheters, respectively, a finding in line with Kim et al11. In a registry-based study, Langer et al found a higher stability rate within the right ostium for the 5 Fr Tiger catheter compared with 5 Fr Judkins catheters but no difference regarding the left ostium; however, comparisons were unadjusted and included only patients without need for catheter change19. The higher instability rate observed in the Tiger within the left ostium could potentially be lessened by adopting a modest contrast injection rate11.
There was a tendency towards less frequent coaxial contact with the right ostium in all angiographic views with the Tiger-II catheter, which also showed higher rates of deep engagement within the right ostium and more frequent selective engagement of the RCA conus, in accordance with Kim et al11. In a report on iatrogenic coronary dissections, a left Amplatz guiding catheter has been implicated in catheter-induced right coronary dissection, while concerns have been raised regarding non-coaxial cannulation and associated ostial dissection risk with one-concept radial-dedicated catheters9,20.
Limitations
Our study was not designed to assess clinical outcome, thus rendering any association between excessive ostial seating or selective conal engagement and procedural complications solely hypothesis-generating. Deep ostial seating rates could be even higher than reported, as vessel length could have been underestimated due to foreshortening in a 2D display. Differences in the studied catheters’ coated materials might have influenced spasm and catheter failure rates. Randomisation was not stratified by operator, and therefore differences in operator proficiency with the study catheters might have influenced the study results; however, no difference was observed in the catheter allocation rate and in the catheter failure rate between observers (Supplementary Table 2, Supplementary Figure 1). The total amount of contrast used (including leftovers) was studied and therefore no assumption can be made regarding contrast volume received by the patient. Contrast medium was delivered using a power injector and manual stopcock-manifold injection system in centre 1 and centre 2, respectively; however, randomisation was stratified by centre.
Conclusions
Tiger-II was found superior to Judkins 3.5L/4R catheters regarding contrast volume use, procedural and fluoroscopy time, spasm rate and RCA imaging, and inferior regarding LAD and LCX imaging. High-volume cathlabs and patients at increased risk of spasm may benefit from Tiger-II use. However, better LCA imaging remains an advantage for the Judkins 3.5L catheter.
| Impact on daily practice Tiger-II was found superior to Judkins 3.5L/4R catheters in reducing contrast volume and procedural time needed in patients undergoing coronary angiography via the right TRA. Therefore, high-volume centres and operators might benefit from Tiger-II use in terms of time and cost saving. The Tiger-II catheter also demonstrated lower fluoroscopic time compared with Judkins 3.5L/4R catheters; although the absolute difference in the median duration of fluoroscopy between groups – which corresponds to one case – was 0.23 minutes, the cumulative benefit of fluoroscopy saving may be of clinical importance to high-volume centres and operators performing multiple procedures per week via the TRA, especially in the light of the fact that fluoroscopy time remains slightly longer with the transradial than with the transfemoral approach15,21. Spasm was less frequently observed in the Tiger-II group; hence, patients at increased risk of spasm (diabetics, women, those with lower body mass index, those at younger age, those with impaired preprocedural radial flow-mediated dilatation, multiple punctures or painful cannulation) might benefit from Tiger-II use22-24. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Supplementary Appendix. Angiographic image quality grading.
Supplementary Table 1. Intraclass correlation coefficient for inter- and intra-observer agreement.
Supplementary Table 2. Allocation to study catheters by operator.
Supplementary Figure 1. Catheter failure rate by operator in the Tiger-II, Judkins 3.5L/4R groups and in the overall population.
To read the full content of this article, please download the PDF.