- coronary dissection
- percutaneous coronary intervention
- coronary occlusion
Abstract
Aims: Iatrogenic occlusive coronary dissection (IOCD) is a rare but high-risk complication of percutaneous coronary intervention (PCI) with limited data on options for management. The aim of this study was to describe a novel approach to the treatment of IOCD in order to gain access to the true coronary lumen. This technique may be feasible in cases in which conventional methods of PCI have failed.
Methods and results: We performed a retrospective analysis of 11 patients with PCI complicated by IOCD. In all cases, IOCD was treated using the contrast-guided subintimal tracking and re-entry “rescue” (STAR-R) procedure. Angiographic success with TIMI 3 flow was achieved in all patients and stent implantation was performed in 81.8% (n=9). At clinical follow-up (mean 186±79 days), target lesion revascularisation was required in 9% (n=1), with target vessel revascularisation in 27.3% (n=3), and a major adverse cardiac event rate of 27.3% (n=3). Angiographic follow-up was obtained in 81.8% (n=9) with a restenosis rate of 11% (n=1).
Conclusions: The STAR-R procedure is a feasible option for the treatment of IOCD following failure of conventional techniques of treatment.
Abbreviations
IOCD iatrogenic occlusive coronary dissection
PCI percutaneous coronary intervention
NHLBI National Heart Lung and Blood Institute
CABG coronary artery bypass graft surgery
STAR-R subintimal tracking and re-entry “rescue” procedure
OTW over-the-wire balloon
MI myocardial infarction
MACE major adverse cardiac event
TVR target vessel revascularisation
TLR target lesion revascularisation
Introduction
Iatrogenic occlusive coronary dissection (IOCD) is defined as the sudden occlusion of a target coronary vessel or the adjacent segment of a vessel during or following percutaneous coronary intervention (PCI). IOCD is classified as a type F dissection according to National Heart Lung and Blood Institute (NHLBI) classification system1. Occlusive dissections occur with variable frequency in the angioplasty era ranging from 5% to 8%2-4. Since the advent of intracoronary stents the frequency of IOCD is now less than 1%5,6. This complication can frequently result in haemodynamic instability3,7 requiring urgent treatment. The primary goal is to obtain access to the distal lumen with a guidewire allowing stent implantation in order to restore coronary flow or coronary artery bypass graft surgery (CABG) if PCI techniques fail. There is no standardised technique for restoring vessel patency; therefore treatment is left to the experience of individual operators resulting in a high incidence of failure of revascularisation with PCI and the need for subsequent urgent CABG. Given the limited available data in this field, the aim of this report was to describe our experience in this setting and to describe a novel approach to the treatment of this condition.
Methods
Patients
We performed a retrospective cohort analysis of all consecutive patients with PCI complicated by an IOCD in our institution between January 2005 and November 2009. The indications for PCI were symptomatic myocardial ischaemia or evidence of reversible myocardial ischaemia as assessed by perfusion or stress testing.
Management of IOCD: the contrast-guided subintimal tracking and re-entry “rescue” (STAR-R) procedure
IOCD were visualised following contrast injection from the guiding catheter. Following failure of initial attempts using conventional floppy wires to negotiate the dissection with the intent of finding the distal true lumen, the operator opted for a different strategy with a more steerable wire: an intermediate or a Miracle 3 (Abbott Vascular, Santa Clara, CA, USA) wire mounted on a microcatheter or an over-the-wire (OTW) balloon was advanced to the level of the proximal end of the dissected segment in order to engage the dissection plane. After removing the wire, a contrast injection was performed with the aim of driving the dissection plane distally in order to create a tubular dissection; i.e., a dissection with a linear morphology consistent with the vessel outline (Figure1)8. Contrast injection was then used in an attempt to create a connection between the false and the true lumen, without the use of guidewires (“hydrodynamic recanalisation”). In cases in which contrast injection did not reveal the true distal lumen, a hydrophilic wire (Whisper or Pilot; Guidant, Abbott Vascular, Santa Clara, CA, USA ) with the tip of the wire shaped into an “umbrella handle” configuration was used to extend the subintimal dissection distally and re-enter the true lumen (“mechanical recanalisation”), Figures2 and 3. It should be noted that the procedure to regain entry into the true lumen using the STAR-R technique should be stopped if attempts are unsuccessful in the presence of progressive haemodynamic instability, or if the STAR procedure results in a large guidewire loop in a distal branch which increases the risk of coronary perforation. Figure4 illustrates the use of the contrast-guided STAR-R technique.

Figure 1. Example of angiographic morphology of a tubular coronary dissection.
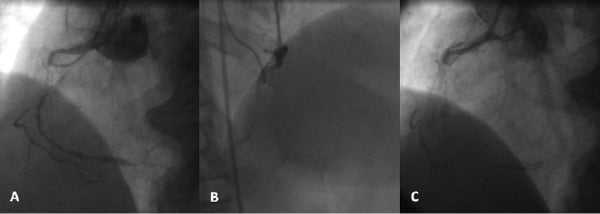
Figure 2. A) Pre-intervention angiographic image of diffusely diseased right coronary artery with proximal subtotal occlusion. B) Iatrogenic occlusive coronary dissection caused by intubation of guiding catheter. C) Re-entry into the true distal lumen using STAR-R technique with guide wire shaped in “umbrella-handle” configuration.
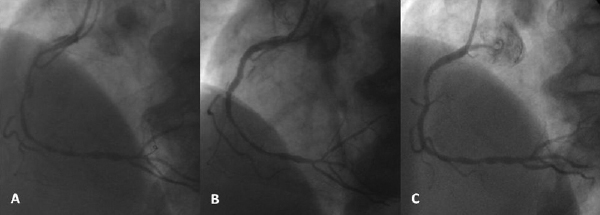
Figure 3. A) Right coronary artery following predilation proximally with compliant balloon. B) Final appearance following stent implantation within proximal segment of right coronary artery. C) Follow-up appearance of right coronary artery six months following index procedure.
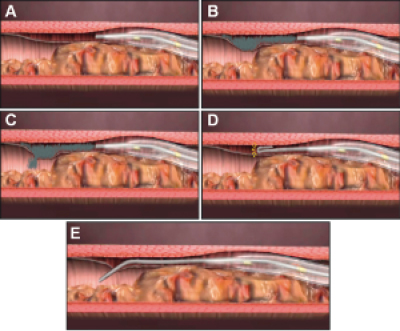
Figure 4. A) Over-the-wire balloon inserted into the dissection plane. B) Contrast injection into the dissection plane in order to create a tubular dissection. C) Contrast injection creates a connection between false and true lumen (“hydrodynamic recanalisation”). D) In case of failure of “hydrodynamic recanalisation” the guidewire can be advanced with an umbrella handle configuration to create “mechanical recanalisation” (yellow arrows show the distribution of force over a large area of guidewire to reduce the risk of perforation.) E) Wire is easily advanced from false to true lumen.
Procedural and clinical outcome definitions
Angiographic success was defined as flow restoration after IOCD with resultant TIMI flow grade3. Myocardial infarction (MI) was defined as an elevation of creatine kinase–MB >3 times the upper limit of normal and divided into Q-wave MI or non-Q-wave MI if new pathological Q-waves in the electrocardiogram were present or absent respectively. Creatinine kinase (CK) was routinely measured after PCI in all patients at our institution and CK-MB was obtained only if total CK is >2 times the upper limit of normal. Procedural success was defined as angiographic success without in-hospital major adverse cardiac events (MACE). MACE was a composite of death, MI, or the need for target vessel revascularisation (TVR) with either PCI or CABG.
Results
From our database we identified 11 patients with IOCD that had occurred during PCI. Baseline clinical characteristics are reported in Table1. In 9% of patients (n=1), the IOCD was related to inappropriate handling of the guiding catheter, and in 54.5% of patients (n=6) dissection occurred due to a secondary inadvertent subintimal passage of the guidewire. The right coronary artery was involved in the majority of cases (n=3, 27.2%). The morphology of the IOCD was of tubular type in all cases8. Lesion and procedural characteristics are reported in Table2.
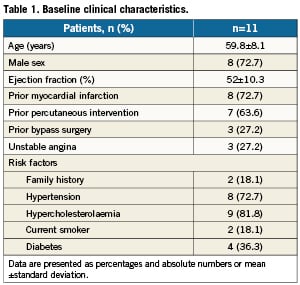
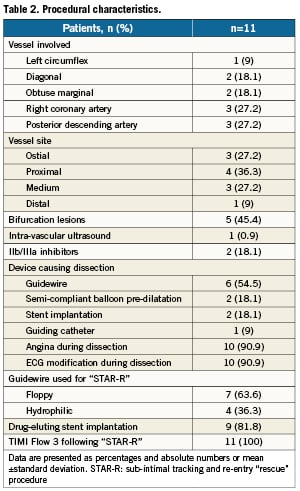
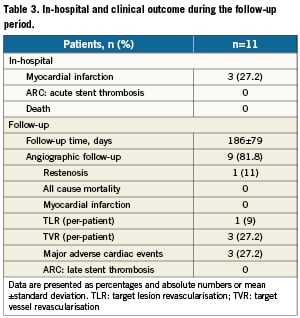
Angiographic success was achieved in 100% (n=11) of patients and a drug eluting stent (DES) was implanted in 81.8% of cases (n=9). In-hospital MI occurred in three patients (27.2%). There were no in-hospital deaths and no cases required urgent CABG surgery. At clinical follow-up (mean 186±79 days), target lesion revascularisation (TLR) occurred in one patient (9%) with TVR in three patients (27.3%) with a MACE rate of 27.3% (n=3). Angiographic follow-up was obtained in 81.8% (n=9) with a restenosis rate of 11% (n=1). In-hospital and long-term outcomes are presented in Table3.
Discussion
In this study we describe an alternative method of treatment for IOCD that occur during PCI and that can be used in the case of failure of conventional manoeuvres. While IOCD occurs infrequently, it is widely recognised as a high-risk complication of PCI. The main findings of this study are: 1) the contrast-guided STAR-R procedure is a feasible option for vessel recanalisation following IOCD; 2) clinical outcomes following the contrast-guided STAR-R procedure are favourable.
Despite the success and progress of PCI, abrupt vessel closure caused by an IOCD is an infrequent but potentially life-threatening complication9. IOCD results from extensive disruption of the medial layer following instrumentation of the vessel leading to the presence of obstructive dissection flaps. IOCD can frequently lead to major complications in terms of death, MI, and emergency CABG10. The aetiology of IOCD has been recognised as predominantly linked to inappropriate handling of the guiding catheter11-13 or subintimal passage of the guidewire14.
Multiple studies in the pre-stent era identified risk factors for the development of coronary artery dissection. Angiographic predictors include calcified lesions15, eccentric lesions, long lesions, complex lesion morphology (ACC/AHA type B or C) and vessel tortuosity16. Patients with acute myocardial infarction or unstable angina have evidence of coronary dissection in as many as 28% of cases, which despite prolonged balloon inflation, predisposes to subsequent subacute thrombosis4. A balloon to artery ratio >1.2 also predisposes to dissection16. In addition, the use of both left and right Amplatz guide catheters appears to lead to a higher rate of coronary dissection, mainly due to “deep and aggressive seating” during engagement of the coronary ostium17.
Although emergency CABG is effective in the setting of IOCD, it is a time-consuming procedure that carries the risk of irreversible, extensive myocardial damage. Percutaneous intervention of IOCD has emerged as an alternative treatment. Stenting remains the most important mechanism for treating this complication as an alternative to emergency CABG once access to the true lumen of the vessel is gained. However, some cases of IOCD are very difficult to treat due to difficulty in positioning a guidewire in the true lumen. Inability to reach the true lumen of a vessel can preclude subsequent stent implantation and restoration of flow. Given that IOCD usually results in haemodynamic instability, these problems can exacerbate an already high risk clinical situation.
Limited data exist with regards to the optimum interventional treatment options following IOCD; this, along with technical difficulties in obtaining re-entry into the true lumen, has meant this event is often managed surgically. We have extrapolated the experience we have gained from treating high volumes of patients with CTO using the STAR technique8,18 into the development of anovel approach to recanalisation of a vessel in the event of IOCD: the contrast-guided STAR-R procedure. This has led to high success rates when using the STAR-R technique in the setting of IOCD in order to restore vessel patency rapidly and to reduce the incidence of potential MACE. The use of this technique leads to successful re-entry into the true lumen in the majority of cases.
Adequate stenting of the dissection remains the most important aim of the treatment of coronary dissection complicated by abrupt vessel closure in order to minimise the extent of ischaemic complications. The operator should seek to contain and cover the distal extent of the dissection as soon as possible with a stent in order to prevent further extension of the dissection flap and reduce the myocardial ischaemia time. In this study, the STAR-R technique was only used in IOCD within the circumflex, obtuse marginal, diagonal, right coronary artery and posterior descending arteries; it was notably not used in the left anterior descending artery. However, in the scenario of IOCD of the left anterior descending artery, the use of the STAR-R technique should be considered with caution and only in the absence of any other method of rapid revascularisation of the threatened territory of myocardium. Of note this method can be associated with the loss of side branches from the main artery and may lead to significant ischaemia when applied to the left anterior descending artery. The operator must therefore apply a risk-benefit analysis comparing the potential risk of ischaemia from loss of side branches versus that of complete myocardial infarction due to loss of the main vessel. The use of the contrast-guided STAR-R procedure can be considered in order to facilitate rapid access to the true lumen of a coronary vessel following failure of conventional methods. However, attempts to wire the true lumen must be carefully limited and in the event of failure, with significant residual myocardial ischaemia, urgent bypass surgery must be considered (Figure5).
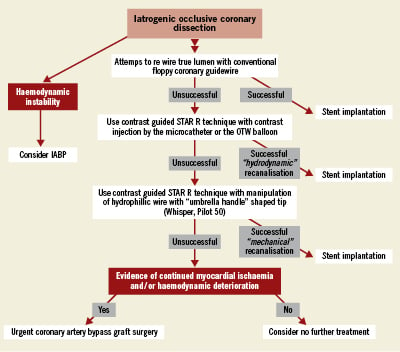
Figure 5. Flow chart illustrating our proposed treatment for the treatment of iatrogenic occlusive coronary dissection based on our experience.
Conclusion
The contrast-guided STAR-R procedure can be considered as afeasible technique for the treatment of coronary dissection complicated by abrupt vessel closure in cases in which conventional PCI methods for re-entering the distal true coronary lumen have failed. The use of this technique allows rapid and successful re-entry into the true lumen in the majority of cases, thereby facilitating stent deployment and leading to haemodynamic stabilisation of apotentially life-threatening complication.
Conflicts of interest statement
The authors have no conflicts of interest to declare.