A 53-year-old woman with no cardiovascular risk factors was admitted for anterior ST-segment elevation myocardial infarction. Coronary angiography revealed an abrupt mid-left anterior descending (LAD) coronary artery occlusion (Figure 1A) and the absence of atheroma in other coronary arteries (Moving image 1, Moving image 2). Spontaneous coronary artery dissection (SCAD) was suspected, and percutaneous coronary intervention was performed because of ongoing ischaemia in a large myocardial area (Moving image 3). Intravascular ultrasound (IVUS) revealed an extensive intramural haematoma, with compression of the true lumen (TL) by the false lumen (FL) throughout the distal segment (Moving image 4), confirming a type 4 SCAD (occluded vessel) and showing a long subintimal passage of the guidewire with a very distal TL re-entry (Figure 1A1-Figure 1A3). The haematoma was manually aspirated, using a 6 Fr Eliminate catheter (Terumo) in order to reduce the compression of the TL. After the first aspiration, coronary flow was immediately restored to Thrombolysis In Myocardial Infarction (TIMI) grade 3 flow (Figure 1B, Moving image 5, Moving image 6) with normalisation of the electrocardiogram. Three aspiration passages across the lesion were performed. Optical coherence tomography (OCT) with a Dragonfly catheter (Abbott) was used to accurately assess the coronary arterial wall morphology and the effect of aspiration. OCT confirmed a proximal intramural haematoma transitioning into a double-lumen morphology and revealed several fenestrations between the false and true lumens with TL decompression (Figure 1B1-Figure 1B4). Several hypotheses for the reperfusion mechanism of the aspiration technique were discussed. The aspiration of the vessel’s subintimal space using an aspiration catheter involves the use of negative pressure and suction force, which can result in the formation of small openings, or fenestrations, in the intimal wall. These physical effects aid in removing approximately 1 millilitre of blood from the subintimal space, reducing compression of the true lumen. Both imaging and aspiration catheters can mechanically create two fenestrations at the subintimal entry and exit points of the guidewire. However, it is important to note that the blood aspirated from the subintimal space was free of thrombus, and the use of imaging catheters before and after the aspiration procedure did not have any effect on coronary flow. Fibromuscular dysplasia was confirmed through computed tomography angiography. The patient was symptom-free, and was discharged 5 days later on aspirin and a beta blocker with a preserved left ventricular ejection fraction. In this case, the aspiration-fenestration technique was an effective bailout revascularisation technique in an occlusive SCAD with failure to regain the true lumen proximally.
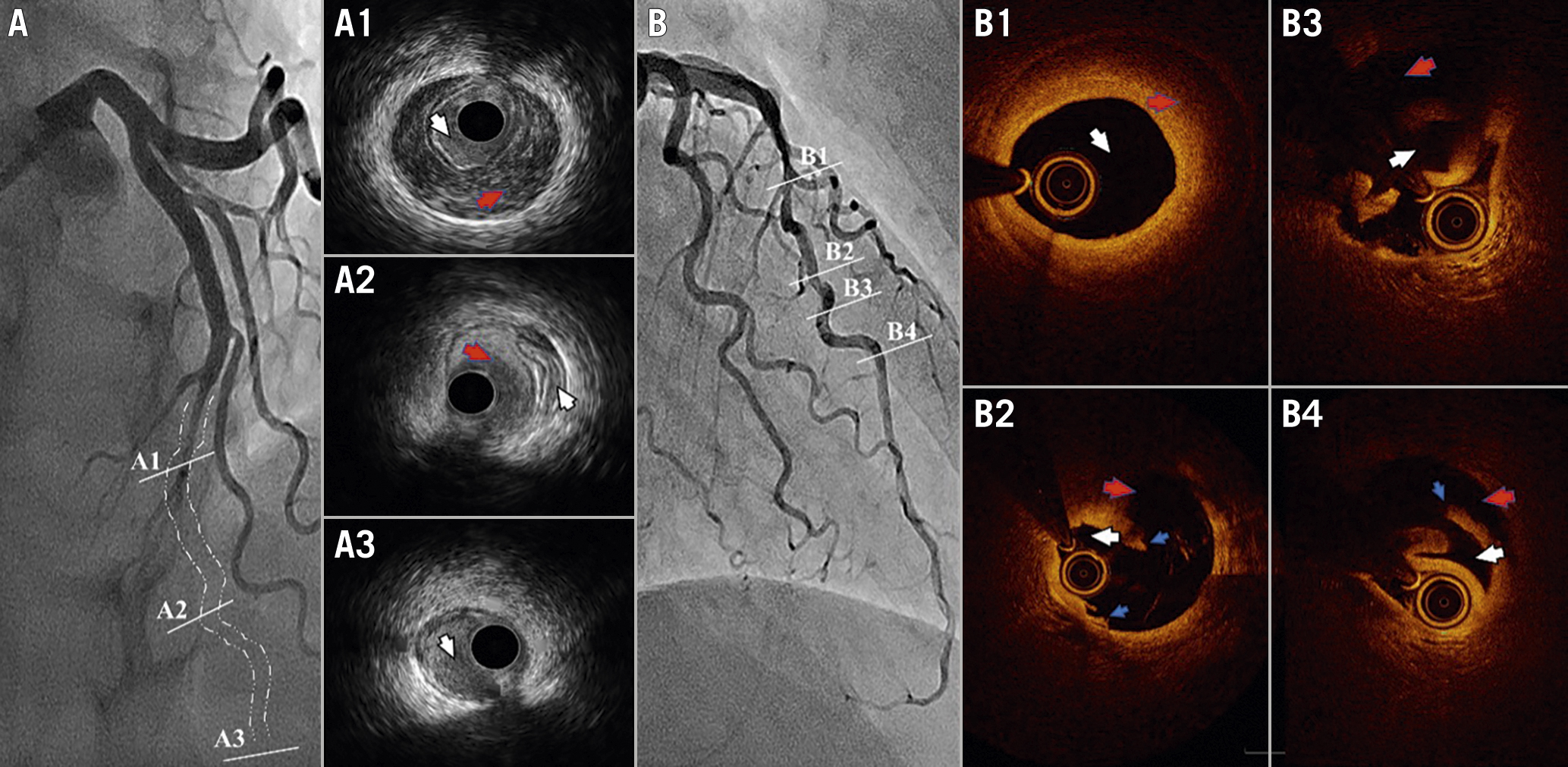
Figure 1. Spontaneous coronary artery dissection and aspiration technique. A) Initial coronary angiography shows an occlusion (white dotted line) in the middle of the LAD. The intravascular ultrasound shows the guidewire is proximally in the TL (A1, white arrow) without communication with the intramural haematoma (red arrow). Mid-vessel, the guidewire entered the subintimal space (A2, red arrow) and the intramural haematoma collapsed the TL (white arrow). Re-entry of the guidewire in the TL distally (A3, white arrow). B) Final coronary angiography revealed multiple radiolucent flaps with preservation of the septal arteries. Optical coherence tomography confirmed the presence of an intramural haematoma (B1, red arrow) followed by multiple intimo-medial fenestrations (B2 and B4, blue arrows) and the decompressed TL (B3, white arrow). LAD: left anterior descending artery; TL: true lumen.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Acute occlusion of the mid-left anterior descending coronary artery.
Moving image 2. No evidence of atheroma in other coronary arteries.
Moving image 3. Ongoing ischaemia in a large myocardial area on the ventriculogram.
Moving image 4. A large intramural haematoma compressed the true lumen throughout the distal segment.
Moving image 5. Multiple radiolucent flaps were identified in the final coronary angiography.
Moving image 6. The septal arteries remain preserved at the end of the procedure.