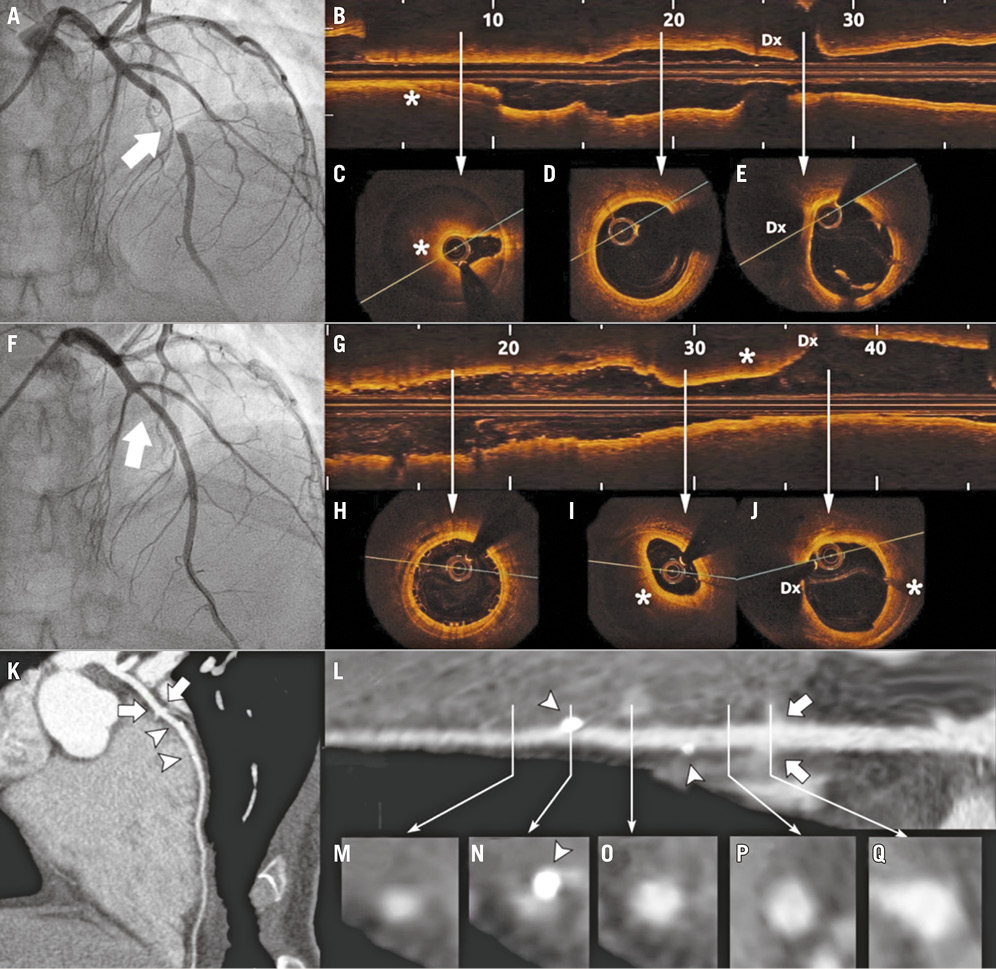
A 34-year-old lady with no cardiovascular risk factors presented with an anterior non-ST-elevation myocardial infarction. Angiography showed a severe stenosis in the mid-LAD with TIMI 1 flow and no images of double lumen (Panel A, Moving image 1). To clarify the underlying pathology, optical coherence tomography (Panel B, Moving image 2) was performed demonstrating the presence of an intramural haematoma compressing the intima with critical luminal narrowing (Panel C, asterisk), and more proximally an apparently normal artery (Panel D, Panel E, Dx: diagonal branch). No “entry door” was visible by OCT. Given the compromised flow, the LAD was treated with a bioresorbable scaffold (BRS) (Absorb™; Abbott Vascular, Santa Clara, CA, USA) (3×18 mm). Coronary flow was restored with a good result in the scaffolded segment (Panel F-Panel H). A new moderate stenosis was generated (arrow in Panel F) by proximal displacement of the haematoma (* in Panel G, Panel I, Panel J, Moving image 3, Moving image 4). The flow in the LAD was TIMI 3 and the patient was asymptomatic so no additional interventions were performed in order to avoid further propagation of the dissection.
At follow-up, the patient remained symptom-free taking dual antiplatelet therapy for one year. Forty months post procedure she complained of atypical chest pain. A coronary CT scan was performed showing a normal LAD with no trace of the BRS except for the two radiopaque markers (Panel K-Panel O, arrowheads showing proximal and distal markers of the scaffold) and complete resolution of the proximal intramural haematoma that was initially left untreated (Panel K, Panel L, Panel P, Panel Q, arrows indicating diagonal and septal).
Spontaneous coronary artery dissection is usually managed conservatively given its natural history of spontaneous healing1. In cases where coronary flow is compromised, BRS are an interesting option to restore flow acutely without the disadvantages of a permanent metallic prosthesis2. However, no evidence about the long-term result of BRS in this setting has been reported until now . The present case illustrates a good anatomical result demonstrated with CT scan more than three years after BRS implantation in a young woman with spontaneous coronary artery dissection.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Baseline angiogram showing a severe stenosis in the mid-LAD with TIMI 1 flow.
Moving image 2. Baseline OCT showing intramural haematoma compressing the intima with critical luminal narrowing.
Moving image 3. Angiogram after scaffold implantation: good result in the scaffolded segment with a new moderate stenosis proximally.
Moving image 4. OCT after scaffold implantation: good result in the scaffolded segment and a new moderate stenosis by proximal propagation of the haematoma until the diagonal branch.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Baseline angiogram showing a severe stenosis in the mid-LAD with TIMI 1 flow.
Moving image 2. Baseline OCT showing intramural haematoma compressing the intima with critical luminal narrowing.
Moving image 3. Angiogram after scaffold implantation: good result in the scaffolded segment with a new moderate stenosis proximally.
Moving image 4. OCT after scaffold implantation: good result in the scaffolded segment and a new moderate stenosis by proximal propagation of the haematoma until the diagonal branch.