A 56-year-old woman, active smoker with no other cardiovascular risk factors was admitted to hospital to undergo elective angioplasty on the proximal circumflex artery. A bioresorbable scaffold BVS 3.0×18mm was implanted. Post-implantation IVUS showed a residual coronary dissection at the distal edge of the scaffold (online Figure). In addition, OCT was performed showing an intimal flap reaching the first frame proximal to the take-off of the side branch distal to the scaffold (Figure1). The dissection was left untreated due to the lack of angiographic evidence of intimal flap and TIMI flow grade 3.1
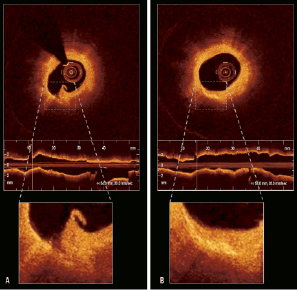
Figure 1. OCT performed after the procedure revealed a coronary dissection (Panel A). At six months follow-up, there was no evidence of dissection but an area of high reflectivity exactly in the same region according to the position of the side branch used as landmark (Panel B).
After six months, coronary angiogram, IVUS-VH and OCT were repeated showing a complete healing of the dissection, however by OCT there was a clearly defined region of high reflectivity (Figure1). We hypothesise that this increase in reflectivity could be related to a local increase in fibrotic tissue and inflammatory cells2 as a result of the wound healing process and should be considered as an intimal scar. There have been previous reports in the IVUS era describing the fate of edge dissections3. However, this is one of the first observations using OCT. The high sensitivity of this technology allows us to observe the mechanisms of repair of the dissection and could be used in longitudinal studies to observe the evolution over time of residual non-obstructive dissections. The study of these complications may have important clinical implications, in order to define which of these dissections deserve further treatment during the index procedure according to the follow-up findings.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Figure. After the procedure IVUS clearly identified a dissection at the distal edge of the scaffold but no evidence of dissection could be found at the angiogram (middle panels). At six month follow-up there was no angiographic and no IVUS evidence of dissection and virtual histology did not show any remarkable change in plaque composition (right panels).
Moving image 1. Oct run portraying the dissection post procedure.
Moving image 2. Oct run at six months with no evidence of dissection.

