A 58-year-old lady presented with atypical chest pain, anterior ECG changes and troponin elevation. Coronary angiography, via the radial artery, delineated unobstructed right and circumflex coronaries but ectasia and delayed contrast clearance within the mid-LAD, suggestive of spontaneous coronary dissection (Figure1). An OCT study was undertaken to confirm the diagnosis. Vessel tortuosity prevented passage of the OCT catheter to the mid vessel despite aggressive guide intubation. OCT evaluation of the proximal LAD, using a pump-assisted contrast flush (20ml contrast injection at 3ml/sec [300 psi]) , revealed no significant arterial pathology. However, on catheter withdrawal an extensive proximal-vessel dissection was evident. The patient remained haemodynamically stable and the dissection was sealed with two stents extending from left main to proximal LAD, with OCT-guided optimisation.
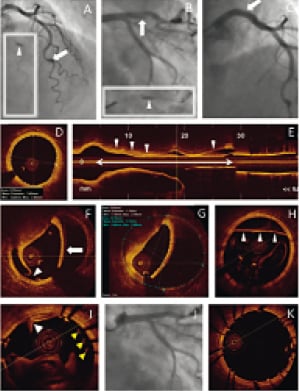
Figure 1. PanelA: Diagnostic angiogram demonstrating mid-LAD ectasia (white block arrow) with late clearance of contrast (inset arrow) suggestive of spontaneous coronary dissection. PanelB: Angiogram, acquired immediately post-OCT acquisition, delineating an iatrogenic dissection (white block arrow) within the proximal LAD with contrast filling of the false lumen (inset arrow). PanelC: Cranial view demonstrating extension of the dissection back into the left main stem (white block arrow). PanelD: Cross-sectional OCT image of reference vessel (prox. LAD mean diameter 3.45mm) PanelE: OCT longitudinal section demonstrating the extent of the dissection – from catheter tip to proximal LAD (double headed white arrow), with a blood-filled false lumen on the superior surface (white arrow heads). PanelF: OCT cross-section demonstrating intimal disruption (white arrow head) and dehiscence of the intima and upper media from the vessel wall (white block arrow) PanelG: OCT cross-section with automated measurements of true lumen area (2.63 mm2) and the true vessel area (10.76mm2 – consistent with PanelD reference area). PanelH: Cross-sectional OCT image of the left main stem demonstrating extension of the intimal dissection (block arrow heads). PanelI: OCT acquisition, following stenting of the LAD with 3.5×23mm Multilink stent (Abbott Vascular, Santa Clara, CA, USA), with evidence of intimal disruption with blood spanning the true and false lumens (white block arrow head) and stent strut malapposition (yellow block arrow heads). PanelJ: Final angiographic result following deployment of an overlapping stent within the LMS (4.0×15 Multilink stent) and post-dilatation to high pressure with 3.5 and 4.0 non-compliant balloons in the LAD and LMS, respectively. PanelK: Final OCT acquisition confirming appropriate stent sizing, strut apposition and minimisation of vessel trauma.
The exquisite images, generated with OCT, facilitate safe and accurate delineation of arterial pathology and optimisation of stenting procedures.1 However, it is important to recognise that imaging techniques are associated with potential risks. The PROSPECT trial reported a 1.6% rate of procedural complicationd.2
OCT image quality remains dependent on the clearance of blood from the vessel lumen. Appropriate guide catheter selection, co-axial coronary intubation and an effective flush technique are critically important for safe and effective OCT image acquisition.
Conflict of interest statement
The authors have no conflicts of interest to declare.

