A 44-year-old man, a smoker with dyslipidaemia, underwent successful percutaneous coronary intervention (PCI) of a chronic total occlusion in the right coronary artery (RCA). The site of occlusion was very proximal. An attempt to cross the lesion was performed using an antegrade approach, during which dissection of the ostium occurred and the guidewire entered the false lumen. The ostial dissection was treated with stent implantation of a Xience, 3.5 x 18 mm (Abbott Vascular, Redwood City, CA, USA). The STAR technique with proximal antegrade subintimal dissection and distal re-entry into true lumen of the posterolateral (PL) branch was then performed1. The bifurcation lesion of PL/posterior descending branch, with significant disease, was treated using the mini-crush technique with implantation of Cypher (Cordis, Johnson & Johnson, Warren, NJ, USA) stents 2.75 x 23 mm and 3.0 x 28 mm, respectively. Three Cypher stents, 3.5 x 23 mm (1), 3.0 x 33 mm (2), and 3.0 x 33 mm (3), were implanted into the false lumen, from proximal to mid RCA with stent overlap, achieving full metal coverage of RCA (Figure 1, Panel A). Due to the complexity of the procedure, a follow-up was planned after eight months, at which the patient was asymptomatic. A coronary angiography showed a moderate restenosis at the site of overlapping stents 2 and 3 (Panel A, arrow) and an irregular profile of the outer border of the segment of overlapping stents 1 and 2, with evidence of saccular protrusions (Panel A, blue dotted line). Optical coherence tomography (OCT) was performed using a non-occlusive technique with 2 mm/sec pullback M2 machine (Image wire and Image system; LightLab Imaging Inc., Westford, MA, USA) and automated injection of iso-osmolar Visipaque medium contrast. OCT documented the presence of moderate neointimal hyperplasia (minimal lumen cross-sectional area of 4.3 mm2), along with abrupt disappearance of circumferential struts in cross sectional images and altered stent geometry (Panels B-E) suggestive of stent fracture, at the coronary segment corresponding to the angiographic restenosis2. It also detected the presence of diffuse strut malapposition with digit like elongations of the vessel wall (Panels F-G) at the site of angiographic saccular protrusions. Most malapposed struts did not present visible tissue coverage (Panels F-G). The patient was discharged with the recommendation to continue aspirin and clopidogrel indefinitely unless serious bleeding occurred. He remained asymptomatic at the 18 month follow-up.
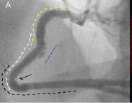
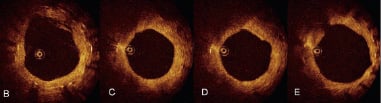
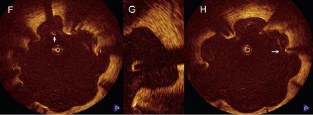
Figure 1. Panel A: Coronary angiogram at eight month follow-up shows moderate restenosis at the site of overlapping stents 2 and 3 (arrow) and an irregular profile of the outer border of the overlapping segment of stents 1 and 2, with evidence of saccular protrusions (blue dotted line). Yellow dotted line: stent 1 (Cypher 3.5 x 23 mm); white dotted line: stent 2 (Cypher 3.0 x 33 mm); black dotted line: stent 3 (Cypher 3.0 x 33 mm). Panels B-E: Optical coherence tomography cross section images, from distal (B) to proximal (E), corresponding to the restenotic segment shown in Panel A (arrow). Evidence of moderate neointimal hyperplasia (B-E), with a minimal lumen cross-sectional area of 4.3 mm2 (D). Abrupt disappearance of circumferential struts (from B to C,D) with altered stent geometry followed by reappearance of circumferential struts (E), suggestive of focal stent fracture. Panels F-H: Malapposed struts with multiple digit like elongations of the vessel wall corresponding to angiographic saccular protrusions (blue dotted line in Panel A). Arrows indicate examples of malapposed struts with no visible tissue coverage. Panel G: High power view of a detail in Panel F (arrow) showing a single malapposed strut with no visible tissue coverage.
Restenosis requiring repeat revascularisation occurs in approximately 50% of patients at angiographic follow-up after STAR technique. Stent fracture has been reported in cases of long stented segments, lesions at hinge points, and use of sirolimus-eluting stents, perhaps facilitated by the closed cell design and high strut thickness of such stent, and is associated with restenosis.3 Abnormal vessel remodelling is a pathological condition that may share similarities with coronary aneurysm formation after drug eluting stents. The presence of malapposed and uncovered struts may represent a substrate for late stent thrombosis.4 OCT allows the detection of these phenomena and may play a role in monitoring their evolution, with a serial assessment, at follow-up in such complex PCIs. However, whether OCT findings, such as strut malapposition and/or coverage, may be useful in clinical decision making (such as prolonging dual antiplatelet therapy) remains to be investigated in future studies.

