CASE SUMMARY
BACKGROUND: A 53-year-old man presented with unstable angina and was found to have an occluded right coronary artery (RCA). A dissection of the aortic sinus of Valsalva (ASV) resulted from the retrograde extension of a dissection of the RCA by an angioplasty guidewire.
INVESTIGATION: Diagnostic angiography, laboratory test, electrocardiography, echocardiography
DIAGNOSIS: Iatrogenic dissection of the ASV from the retrograde extension of a dissection of the RCA, leading to total occlusion, by an angioplasty guidewire.
TREATMENT: Medical therapy at discharge and during follow-up; laboratory test; electrocardiography; echocardiography; stenting of the occluded RCA with spontaneous re-appearance of distal blood flow two weeks later.
KEYWORDS: sinus of Valsalva dissection, coronary angioplasty, coronary stenting
PRESENTATION OF THE CASE
A 53-year-old man, a 20-cigarettes-per-day smoker, presented to the emergency department because of a new onset of episodic exertional dizziness and chest pain associated with cold sweating over the previous month. He was not obese and on no medications, had no medical history and no family history of cardiac disease. There was no specific abnormality upon physical examination and he had normal blood pressure.
An electrocardiogram (ECG) showed sinus rhythm, negative T waves in the inferior leads and flattened T-waves in leads V1 to V4. An echocardiography showed a normal ejection fraction and hypokinesis of the posterior/inferior wall. He was diagnosed as having unstable angina. Coronary angiography revealed a 70% lumen narrowing at the mid-left anterior descending coronary artery (LAD) (Figure 1A and Moving image 1) and a subtotal occlusion in the proximal, mildly calcified RCA, with distal blood flow of thrombolysis in myocardial infarction (TIMI) grade 1 (Figure 1B and Moving image 1). The distal RCA was well-opacified and collateralised from the left coronary artery.
Ventriculography revealed mild localised hypokinesis of the inferior wall, with an ejection fraction of 65%. Coronary angioplasty of the occluded RCA was attempted via the right femoral artery using a 6 Fr arterial sheath. The RCA was cannulated with a 6 Fr Judkins right 4 cm curved guiding catheter (JR4; Cordis Corp., Miami, FL, USA). Fifteen minutes into the procedure, during the application of a 0.014 inch Miracle 3 wire (Asahi Neo’s; Asahi Intecc Co. Ltd; Aichi, Japan), a crescent-shaped dye retention appeared in the aortic wall on the right aortic sinus of Valsalva (ASV), after contrast medium injection (1 mL) (Figure 1C and Moving image 2). Another gentle manual injection of contrast medium revealed total occlusion of the RCA and retrograde progression of the dissection of the proximal RCA extending into the right ASV through the intracoronary entry point (Figure 1D and Moving image 3). The patient had no complaints and was haemodynamically stable at this point. Coronary angiography after 15 minutes of observation revealed total occlusion of the RCA, with no further extension of dissection. The patient refused to have coronary artery bypass surgery despite understanding the risk of medical management. Serum cardiac enzymes including creatine kinase (CK), CK-MB, and troponin I, taken six hours after the percutaneous coronary intervention (PCI), were within the normal range, 129 U/l, 2.3 ng/ml, and 0.03 ng/ml, respectively. The ECG revealed no ST elevations.
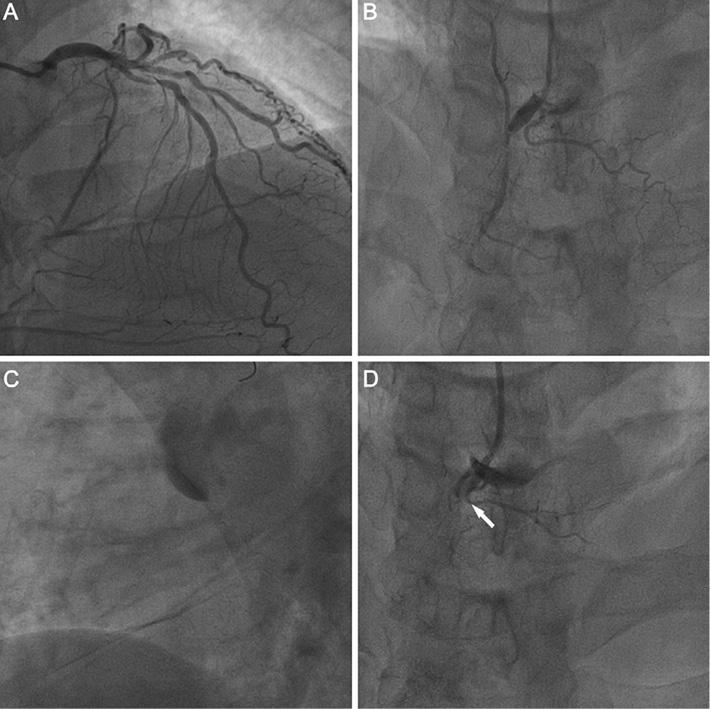
Figure 1. Angiogram in the cranial view: A and B) 70% lumen narrowing at the mid-left anterior descending coronary artery and near-total occlusion of the proximal right coronary artery with a distal blood flow of TIMI (thrombolysis in myocardial infarction) grade 1 and well-collateralised from the left coronary artery; C) crescent-shaped dye retention in the aortic wall in the right aortic sinus of Valsalva (ASV) after a contrast medium injection; D) retrograde extension of the coronary dissection into the right ASV, resulting in total occlusion at the proximal segment. Arrow shows the entry port from the blood stream.
How would I treat?
THE INVITED EXPERTS’ OPINION
In patients with multivessel disease presenting with unstable angina and dynamic ST changes, it is important to find the culprit lesion responsible for the acute clinical situation. In these clinical scenarios treating the true lesion provides for a successful outcome, with rapid recovery from symptoms and less complications.
In this case, although coronary angiography reported a 70% luminal narrowing at the mid-left anterior descending coronary artery (LAD), the image of the LAD shows more severe stenosis (>80%) before the septal branches and a total occlusion in the proximal, mildly calcified right coronary artery (RCA), with distal blood flow of thrombolysis in myocardial infarction (TIMI) grade 1. However, the distal RCA was both well-opacified and collateralised from the left coronary artery, more likely due to a chronic total occlusion (CTO) of the RCA. For these reasons, the inferior wall of the myocardium is also very dependent on blood supply from the LAD instead of the RCA.
In our opinion, in this particular case, the culprit lesion that is responsible for the recent increase in angina and symptoms is the LAD and treatment of the LAD should be the priority in this acute clinical setting in order to see symptom recovery. In stable clinical settings, however, We would start percutaneous coronary intervention (PCI) from the RCA, the most severe lesion. We would do this because, if not successful, PCI of a CTO RCA could not be performed, and we would choose surgery as the proper treatment option in this case to ensure total revascularisation without performing PCI of the LAD.
In this particular case shows a right coronary artery ostial dissection propagating to the ascending aorta during PCI of the complex RCA occlusion. After observing the iatrogenic aortic dissection (IAD) with failed treatment of CTO RCA lesions, the conservative strategy with a close follow-up will be the more correct approach in this case. The immediate management of an impending death situation is the stabilisation of the patient in the cathlab with the correction of the coagulation cascade using protamine. The size of the dissection should then be followed closely, and any evidence observed using either TEE or transthoracic echocardiography of cardiac tamponade will be of great importance.
Many of the reported cases of right coronary artery dissection extending into the aorta are likely to be secondary to catheter manipulation and injection with a deep catheter engagement1,2.
The wire was not kept in the RCA lumen while dissection was diagnosed. Therefore, in order to avoid further enlargement of the IAD and haematoma, it would not be an advisable strategy to rewire the RCA and attempt to implant a stent into the ostium of the RCA for limiting the aortic dissection. Furthermore, in this case, retrograde blood supply from the LAD to the distal RCA is protecting the myocardium from acute severe ischaemia with ST changes seen on ECG.
Transfer to the intensive care unit (ICU) should be accomplished immediately. Then the patient will be managed conservatively (ECG, clopidogrel, aspirin, other medication and enzymes controls such as are done for routine PCI) with a “wait-and-watch” strategy by performing serial multislice cardiac tomography (MSCT) or TEE to evaluate the amount of blood collection in the aorta as well as the existence of pericardial effusion.
The incidence of IAD is between 0.02% and 0.05% during percutaneous coronary interventions and is mostly related to the RCA ostium. Emergency surgical repair should only be proposed for the life threatening expansion of the intramural haematoma and uncontrolled dissection in repetitive imaging despite close medical follow-up3.
If the clinical and haemodynamic findings of the patient are stable and without any negative findings in the follow-up CT imaging, full healing of the aorta and absorption of the haematoma could occur. Although, mortality in iatrogenic aortic dissection is as high as that of spontaneous dissections (up to 35%) and have a higher incidence of concomitant myocardial infarction4,5, the type of dissection in this case fulfils the criteria for limited dissections. Fortunately haemodynamic compromise was not observed6-8.
Repeat intervention to the RCA will carry a high risk of PCI failure as well as repetitive life-threatening IAD. It is for these reasons that this patient should be considered as a candidate for cardiac surgery. Cardiac MSCT is crucial to evaluate both the aorta and coronary arteries before surgery.
Conflict of interest statement
The authors have no conflicts of interest to declare.
How would I treat?
THE INVITED EXPERT’S OPINION
Iatrogenic occlusive coronary dissection (IOCD) is a rare (<1%) but high-risk complication of percutaneous coronary intervention (PCI), the association with an aortic dissection is still more infrequent and could be life-threatening. Most frequently, the right coronary artery is seen to be involved, and more rarely the left anterior descending or the left main. In fact, while there is no established recommendation for treating this complication, very often the interventionalist will attempt to deliver a stent to fully cover the ostium of the culprit lesion.
Many risk factors for the development of coronary artery dissections have been identified such as unusual lesions (calcified, eccentric, long, tortuous) and, more often, the use of both left and right Amplatz guide catheters which can create an intimal tear during engagement in the coronary ostium. The extension to the ascending aorta could be due to an intimal lesion with retrograde progression, but is also probably linked to an individual aorta tissue abnormality.
Concerning the treatment itself in this case, it depends on the immediate clinical situation and its evolution using repeat angiography, CT scan, echocardiography and IVUS, all of which could be useful in order to seal the entry port and break down the dissection route. This strategy can be used to ensure complete coverage of the coronary dissection and precise placement of the stent in order to fully cover the ostium of the culprit lesion1. Recently, Carlino et al2 has proposed a novel strategy successfully using contrast-guided subintimal tracking and a re-entry “rescue” (STAR-R) procedure.
When there is an acute coronary closure complicated by an ischaemic and/or haemodynamic instability, it is recommended to reopen urgently the artery by stenting or CABG in case of failure. The STAR-R procedure2 could be proposed to restore the coronary flow when the conventional interventional techniques have failed.
In the case of cardiogenic shock due to the complication of an aortic dissection, emergency surgery should be considered. While the mortality for this procedure remains high, it is seen to be life-saving3.
If the patient is stable without any ischaemic episodes, and if the aortic dissection is limited, a conservative strategy could be considered under repeat assessment (angiography, CT etc...)4 in a clinical environment with cardio-surgical facilities. It is here, in this type of situation, that the heart team can discuss the best treatment option based on the evolution of clinical and imaging observations and data.
Finally, in this particular case presented by the authors, the patient remained stable without any ischaemic event or aortic complication so we can say that, definitively, there is no indication for emergency surgery, however, the coronary ostium tear needs to be closed by PCI in order to avoid further dissection extension.
Conflict of interest statement
The author has no conflict of interest to declare.
How did I treat?
ACTUAL TREATMENT AND MANAGEMENT OF CASE
Although asymptomatic during observation in the coronary care unit, transthoracic echocardiography was performed daily and revealed no evidence of pericardial effusion or extension of the aortic dissection. The patient was discharged on a medical regimen of aspirin 100 mg, bisoprolol 5 mg and clopidogrel 75 mg once daily. During follow-up he complained only of occasional exertional angina with no significant change of ECG. Repeat coronary angiography two weeks after discharge revealed 70% lumen narrowing at the mid-LAD, sealing off of the dissection and subtotal occlusion in the proximal RCA with restoration of distal flow TIMI grade 1 (Figure 2A and Moving image 4).
A 0.014-in Miracle 3 wire was used for RCA angioplasty (Figure 2B and Moving image 4). An excellent result was obtained after elective implantation of one stent in mid-LAD and two stents in RCA (Titan2®; HEXACATH, Paris, France: 3.0×19 mm, 3.5×28 mm and 3.5×16 mm, respectively) (Figure 2C and Moving image 5). The patient did well on medical therapy during a 6-month follow-up.
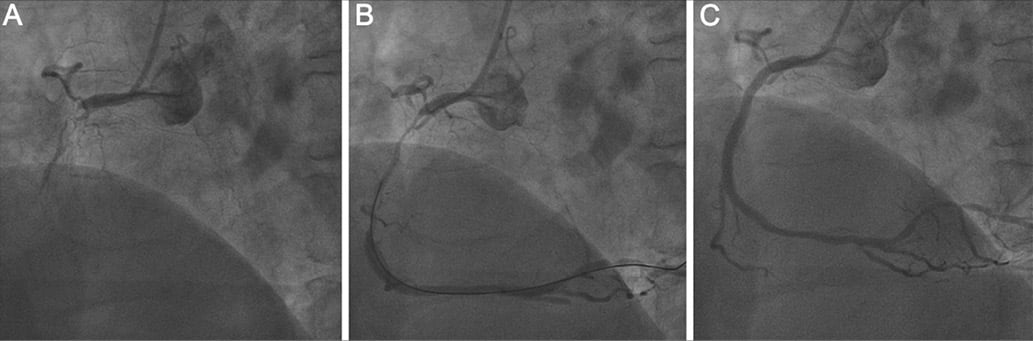
Figure 2. Angiogram in the left anterior oblique view two weeks after the complication: A) near-total occlusion in the proximal right coronary artery and spontaneous regression of the retrograde dissection, with reappearance of distal blood flow of TIMI (thrombolysis in myocardial infarction) grade 1; B) Successful passage of the guidewire and restoration of distal blood flow following balloon dilatation; C) Final angiographic result showing antegrade flow of TIMI grade 3 after stent deployment.
Discussion
While iatrogenic aortic dissection is a well-recognised complication of PCI1, coronary dissection with retrograde extension to the aortic root is exceedingly rare and potentially life-threatening, with a reported incidence of 0.02%2-4. Data completed at our hospital from October 2008 through July 2011 revealed the incidence of retrograde dissection of the ASV was 1 in 1348 (0.07%) PCIs.
There are previous reports of 18 cases of retrograde dissection to the ASV complicating PCIs2,4-8 (Table 1). Of the 18 cases, 17 (94%) were related to RCA procedures, among which JR4 guides were being used at the time of the dissection in 12 (71%) cases. The exact mechanism of the predisposition of RCA to retrograde dissection is not clearly understood, but probably because the haemodynamic force vector is directed to the right side convexity of the ascending aorta. The calcification of the RCA in our patient has been suggested to be a risk factor6. Furthermore, the left main coronary artery has both a larger size and more spiral smooth muscle cells with abundant elastic fibres than the RCA, which may protect it from guide catheter trauma6,9. Although the exact mechanism responsible for this complication remains unknown, contrast injection may cause an existing dissection to progress6. Relatively aggressive attempts to reinsert a cannula into a proximal coronary occlusion may also promote a subintimal passage of the guidewire. Retrograde progression of the dissection could be facilitated by a tethering effect induced by the occlusive lesion on the vessel layer10. Other potential risk factors, such as calcification in the aortic roots, old age >60 years and hypertension, have been proposed as playing an important role in the appropriateness of dissection6.
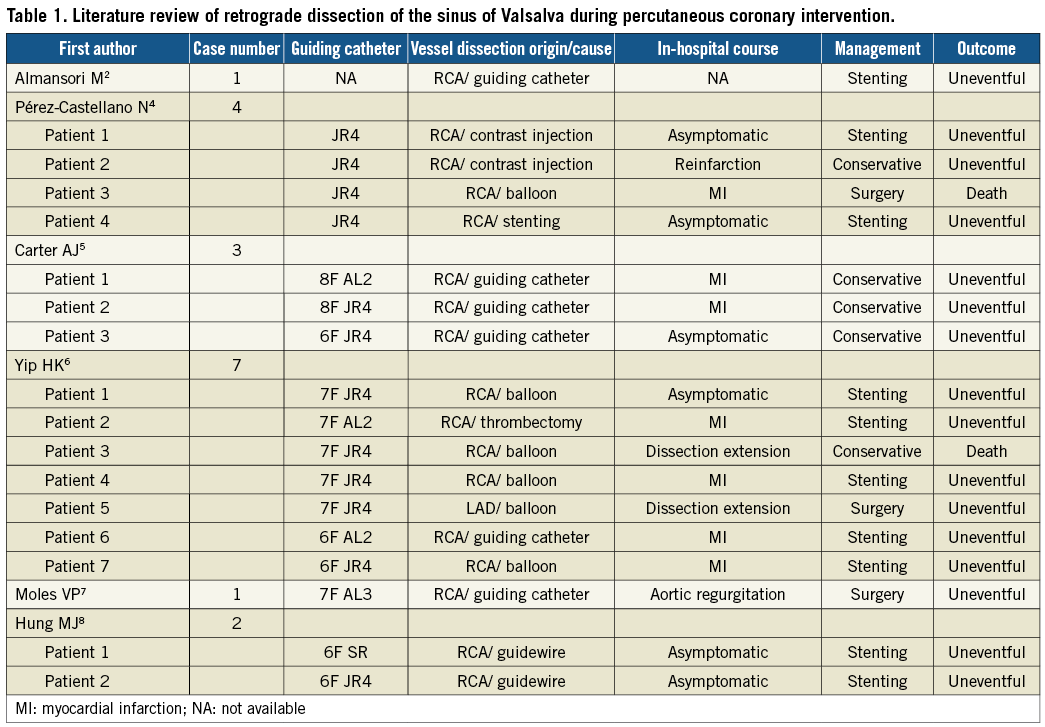
Treatment options regarding management of this iatrogenic and potentially life-threatening complication include conservative management, coronary stenting and emergency or elective bypass surgery. The conservative management strategy is suitable for stable patients without evidence of extension or significant myocardial ischaemia because these tend to resolve spontaneously in the first month3. Although coronary stenting as soon as possible is suggested to treat patients with limited aortic involvement, and can stabilise the patient’s condition and act as a bridge for surgical intervention6,10, when dissection of the ASV occurs, stenting of the proximal segment is questionable. On one hand, sealing of the coronary dissection might protect the coronary artery from occlusion and the aorta from additional dissection, but on the other hand the trauma of stenting might extend the aortic dissection4. Consistent with a previous report, the outcome of our patient also implies that the reassuring information provided by sequential transthoracic or transoesophageal studies to define the characteristics and to exclude its subsequent extension appears invaluable in stable patients8,10.
Our case demonstrates that localised retrograde dissection of the ASV during PCI may be asymptomatic and result from guidewire trauma. Sealing of the coronary entry door may occur spontaneously in two weeks if there is no evidence of extension. Excluding dissection progression with close transthoracic echocardiographic surveillance appears to be a reasonable conservative strategy for stable patients, and repeat PCI can be safely performed later.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Coronary angiogram showing mid-LAD stenosis and near-total occlusion of the proximal RCA with the well-collateralised distal RCA from the left coronary artery.
Moving image 2. Crescent-shaped dye retention in the aortic wall in the right aortic sinus of Valsalva.
Moving image 3. Retrograde extension of the right coronary dissection into the right aortic sinus of Valsalva, resulting in total occlusion at the proximal segment.
Moving image 4. Near-total occlusion in the proximal RCA and spontaneous regression of the retrograde dissection with reappearance of distal TIMI 1 flow. Restoration of distal blood flow following successful passage of the guidewire and balloon dilatation.
Moving image 5. Final angiographic result showing antegrade flow of TIMI grade 3 after 2 stents deployment at proximal and mid-distal RCA.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1.
Moving image 2.
Moving image 3.
Moving image 4.
Moving image 5.

