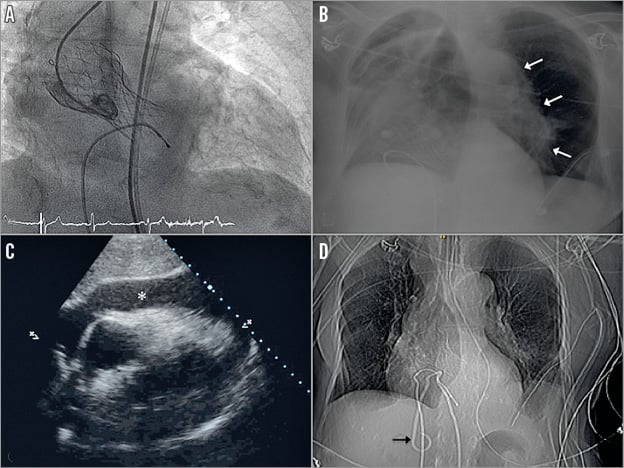
Transcatheter aortic valve implantation (TAVI) has emerged as a new therapeutic option for patients deemed too high-risk for surgery. A significant learning curve has been reported. Not only the implantation but also the subsequent management are crucial. We present an 83-year-old female with severe symptomatic aortic stenosis and a logistic EuroSCORE of 28%, who underwent successful transfemoral CoreValve® (Medtronic, Minneapolis, MN, USA) implantation (Panel A, Moving image 1, Moving image 2). One day after the procedure, she developed a third-degree atrioventricular block. A temporary pacemaker lead was inserted. The procedure was difficult and many intracardiac manipulations were needed. Four hours later, a complete loss of ventricular capture was observed, so she underwent an urgent repositioning. Once again it was difficult and the physician decided to use a subclavian vein access. Minutes later the patient developed symptomatic hypotension, sharp chest pain and dyspnoea. An anteroposterior chest X-ray showed a left pneumothorax with lung collapse (Panel B). Myocardial perforation was also suspected and a bedside echocardiography revealed a large pericardial effusion with signs of tamponade (Panel C). An emergent pericardiocentesis was performed; however, the patient did not improve as expected and a computed tomography scan was done. It showed the drainage catheter inadvertently inserted into the inferior vena cava (Panel D). Despite emergent radioscopically guided repositioning of the catheter, the patient died.
The growing experience with TAVI procedures has increased the implantation success rate and in-cathlab complications are reducing. However, procedure-related complication risks do not end after a successful implantation but rather continue during the post-implantation period. An experienced multidisciplinary team is essential.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Angiography of CoreValve position after successful implantation.
Moving image 2. Trivial aortic regurgitation after TAVI.
Supplementary data
To read the full content of this article, please download the PDF.
Angiography of CoreValve position after successful implantation.
Trivial aortic regurgitation after TAVI.