Aortic annulus rupture is a rare, lethal complication of transcatheter aortic valve implantation (TAVI)1, which can develop into a left ventricular pseudoaneurysm2. Here we describe the percutaneous management of a patient in whom a left ventricular outflow tract (LVOT) pseudoaneurysm developed following TAVI.
A 79-year-old female with a history of hypertension, hyperlipidaemia, peripheral vascular disease, and lung adenocarcinoma presented with severe symptomatic calcific aortic stenosis (AS) (mean gradient 43 mmHg, aortic valve area 0.83 cm2). Due to the intermediate STS score of 3.45% and anticipated lung malignancy resection surgery, TAVI was recommended by the cardiac team. Chest computed tomography (CT) revealed an aortic annulus area of 5.1 cm2 with a perimeter of 83 mm, and an LVOT area of 3.35 cm2 with a perimeter of 69 mm. Based on these measurements, a 26 mm Edwards SAPIEN 3 bioprosthesis (Edwards Lifesciences, Irvine, CA, USA) that was 1.8% oversized at the aortic annulus and >30% oversized at the LVOT was implanted using a transfemoral approach (Moving image 1). Upon deployment of the valve, the patient became haemodynamically unstable due to annular rupture at the level of the LVOT complicated by acute tamponade (Moving image 2). Emergent pericardiocentesis was performed with drainage of 200 cc of blood. As the patient became haemodynamically stable, she was transferred to the CCU for monitoring.
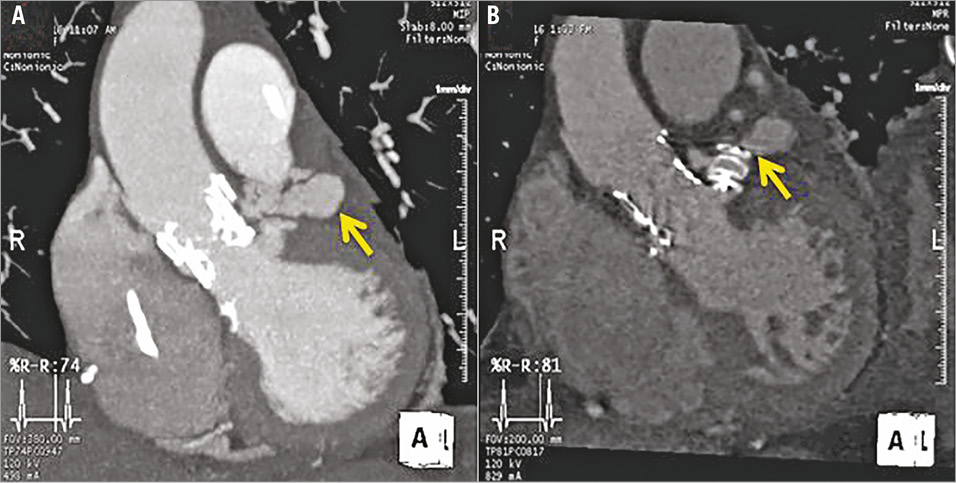
Next day, transoesophageal echocardiography (TEE) revealed a 32×15 mm LVOT pseudoaneurysm anterior to the left main extending laterally from the aortic root, following the course of the left anterior descending artery (Panel A, Moving image 3). A percutaneous approach was chosen based on high risk of open repair. After placement of a 6 Fr sheath in the right femoral artery, a left ventricular angiogram demonstrated persistent rupture of the LVOT below the newly placed valve. The neck of the pseudoaneurysm was successfully engaged with an Amplatz left (AL) 0.75 guide. A 12 mm AMPLATZER™ Vascular Plug II (St. Jude Medical, St. Paul, MN, USA) was deployed at the neck of the pseudoaneurysm and secured according to multiple tug tests (Moving image 4). TEE prior to discharge revealed a secure AMPLATZER plug and well-functioning aortic bioprosthesis. CT consistently showed reduction of the pseudoaneurysm to 19×15 mm with reduced contrast opacification (Panel B). A follow-up CT scan four weeks later showed a re-enlargement of the pseudoaneurysm to 41×18 mm, leading to an open heart aortic valve replacement (19 mm bovine Trifecta™ implant; St. Jude Medical) and pericardial bovine patch placement for complete closure of the pseudoaneurysm.
The failure of the percutaneous approach may be explained by the small size of the selected AMPLATZER plug, which provided only partial occlusion of the neck. Persistent flow into the pseudoaneurysm may have contributed to its re-enlargement. Open heart surgery for pseudoaneurysm closure in the TAVI population is especially challenging due to the high-risk nature of this patient population, and thus a percutaneous approach may be a feasible option3. Further development and refinement of percutaneous approaches are needed.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. A 26 mm Edwards SAPIEN 3 transcatheter aortic valve bioprosthesis was implanted using a transfemoral approach within the aortic annulus.
Moving image 2. Annular rupture complicated by acute tamponade upon deployment of the valve.
Moving image 3. A 32×15 mm LVOT pseudoaneurysm anterior to the left main extending laterally from the aortic root and following the course of the left anterior descending artery.
Moving image 4. Closure of pseudoaneurysm via percutaneous placement of a 12 mm AMPLATZER Vascular Plug II.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. A 26 mm Edwards SAPIEN 3 transcatheter aortic valve bioprosthesis was implanted using a transfemoral approach within the aortic annulus.
Moving image 2. Annular rupture complicated by acute tamponade upon deployment of the valve.
Moving image 3. A 32x15 mm LVOT pseudoaneurysm anterior to the left main extending laterally from the aortic root and following the course of the left anterior descending artery.
Moving image 4. Closure of pseudoaneurysm via percutaneous placement of a 12 mm AMPLATZER Vascular Plug II.