Abstract
Aims: We aimed to investigate whether thrombus aspiration could preserve the index of microcirculatory resistance (IMR) after primary percutaneous coronary intervention (PCI) in patients with ST-elevation myocardial infarction (STEMI).
Methods and results: Sixty-three patients with STEMI were randomised into two groups: primary PCI after thrombus aspiration (aspiration group, n=33) and primary PCI without thrombus aspiration (non-aspiration group, n=30). IMR was measured using a pressure-temperature sensor-tipped coronary wire. Echocardiography was performed at baseline and at six-month follow-up. No significant differences in baseline ejection fraction (EF, 47.3±8.5% vs. 49.5±7.8%, p=0.281) and baseline wall motion score index (WMSI, 1.45±0.31 vs. 1.37±0.27, p=0.299) were observed between the two groups. However, significant differences in IMR (23.5±10.2 U vs. 34.2±21.7 U, p=0.018), ∆EF (follow-up EF - baseline EF; 3.33±4.6% vs. 0.73±1.9%, p=0.005), and ∆WMSI (follow-up WMSI – baseline WMSI; -0.121±0.16 vs. -0.004±0.07, p=0.001) were observed between the two groups.
Conclusions: Thrombus aspiration as an adjunctive method to primary PCI for STEMI may preserve microvascular integrity and have beneficial effects on myocardial microcirculation.
Introduction
Despite achievement of normal coronary artery flow after primary percutaneous coronary intervention (PCI) in patients with ST-elevation myocardial infarction (STEMI), many do not achieve myocardial microvascular reperfusion and show poor clinical outcomes1-3. Distal thrombus embolisation or atheromatous debris during primary PCI may play an important role in cardiac microvascular damage4. Manual thrombus aspiration can preserve microvascular integrity and seems to improve clinical outcomes after PCI for STEMI5-7. The index of microcirculatory resistance (IMR) measured using a pressure-temperature sensor-tipped guidewire is a novel measure of microvascular function. IMR has been validated in animal models and tested in stable patients8-10. In a recent study, IMR was found to be a good predictor of microvascular damage and provided a quantitative assessment of microvascular function after STEMI11,12. The purpose of this study was to investigate whether manual thrombus aspiration can preserve IMR after primary PCI in patients with STEMI.
Methods
PATIENTS
Sixty-three (n=63) patients were admitted with STEMI and had undergone primary PCI. Patients were randomly assigned either for manual thrombus aspiration before PCI or for conventional PCI. To remove the potential effect of operator bias, randomisation was performed on a 1:1 ratio by web-based allocation method according to age, gender and diabetes before diagnostic coronary angiography. The inclusion criteria were as follows: 1) age >18 years, 2) chest pain for >30 minutes, 3) first STEMI within 12 hours from the onset of symptoms, and 4) ST-segment elevation of >0.1 mV in two or more contiguous leads on the electrocardiogram. Patients were excluded if they had cardiogenic shock, a history of previous myocardial infarction, and contraindications to adenosine. The study was approved by Inha University Hospital’s institutional review board, and written informed consent was obtained from each patient.
STUDY PROTOCOL AND PROCEDURE
All patients were pretreated immediately before the primary PCI with aspirin (loading dose of 300 mg followed by 100 mg per day), clopidogrel (loading dose of 600 mg followed by 75 mg per day), and intravenous heparin. In the aspiration group, the thrombus was aspirated from >2 passages across the lesion using an Export Aspiration catheter (Medtronic, Inc., Minneapolis, MN, USA) before stenting. All inserted stents were zotarolimus-eluting stents (Endeavor Resolute and Resolute Integrity; Medtronic, Inc.). Abciximab was not administered. Standard therapies after PCI included nitrates, ß-blockers, statins, and angiotensin-converting enzyme inhibitors or angiotensin-II receptor blockers according to current guidelines13.
PHYSIOLOGICAL ASSESSMENT
After successful stenting of the culprit lesion, a coronary pressure-temperature sensor-tipped coronary wire (St. Jude Medical, Inc., St. Paul, MN, USA) was positioned in the distal two-thirds of the culprit artery. The position of the microsensor was carefully maintained throughout the procedure. Adenosine was continuously infused (>180 µg/min) via an intracoronary microcatheter to induce maximal hyperaemia14. Incremental doses of 180, 210, 240, 270, 300 µg/min of adenosine were administered and we were sure that maximal hyperaemia was achieved since there was no further decrease in fractional flow reserve and distal coronary pressure. Mean hyperaemic transit time was determined by averaging the transit times after three bolus injections of 3 ml room temperature saline through the guide catheter as previously described in the literature15. We defined IMR as the distal coronary pressure multiplied by the mean hyperaemic transit time (mmHg×s, or units)8.
ANGIOGRAPHY
Pre- and post-procedural thrombolysis in myocardial infarction (TIMI) grade and TIMI myocardial perfusion grade (TMPG) were assessed in the infarct-related artery (IRA)16. Collateral circulation was quantified into grades, as described by Rentrop et al17. The image findings were reviewed by two experienced interventional cardiologists who were unaware of the IMR results.
ECHOCARDIOGRAPHIC ANALYSIS
A baseline transthoracic echocardiogram was obtained at admission, and follow-up echocardiography was performed six months after the acute event. An ejection fraction (EF) was calculated using the modified Simpson’s method. Regional wall motion abnormality (RWMA) was scored according to the recommendations of the American Society of Echocardiography, and a wall motion score index (WMSI) was calculated by the sum of the score of all segments divided by the total number of segments18. The change in WMSI was calculated by subtracting the follow-up WMSI from the baseline WMSI.
BLOOD SAMPLES
Blood samples were obtained to measure creatine kinase (CK) and CK-myocardial band (CK-MB) levels before and after PCI. Peak CK and CK-MB levels were defined as the highest CK and CK-MB values measured, respectively.
CORONARY RISK FACTORS
Coronary risk factors were defined as follows: hypertension (a history of hypertension, systolic blood pressure of ≥140 mmHg, and/or diastolic blood pressure of ≥90 mmHg); diabetes mellitus (a history or presence of diabetes, a fasting plasma glucose concentration of ≥126 mg/dl, and/or a glycosylated haemoglobin level of ≥6.5% during hospitalisation); and dyslipidaemia (a history of dyslipidaemia and/or total cholesterol level ≥200 mg/dl, low-density lipoprotein cholesterol level ≥140 mg/dl, high-density lipoprotein cholesterol level <40 mg/dl, and/or triglyceride level ≥150 mg/dl).
STATISTICAL ANALYSES
Values are presented as mean±standard deviation (mean±SD). Mean values were compared using the Student’s t-test. A p-value of less than 0.05 was considered statistically significant. Statistical analysis was performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA).
Results
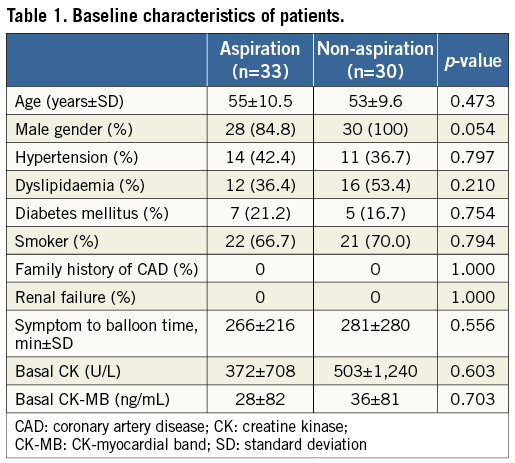
BASELINE CHARACTERISTICS
Sixty-three patients with STEMI were enrolled. The patients’ baseline characteristics are shown in Table 1. The differences in the baseline characteristics between the two groups were not significant.
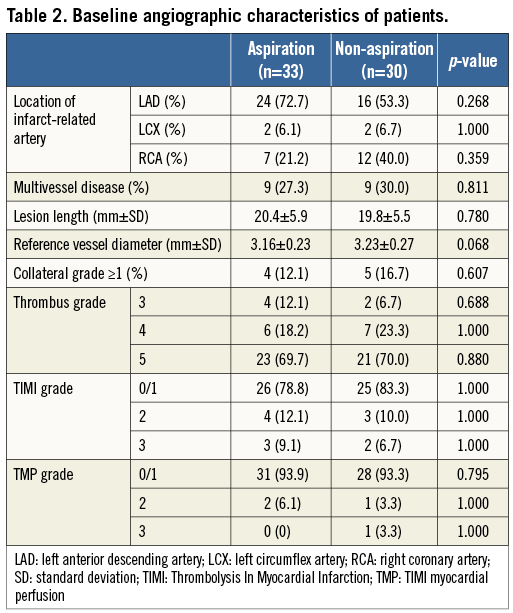
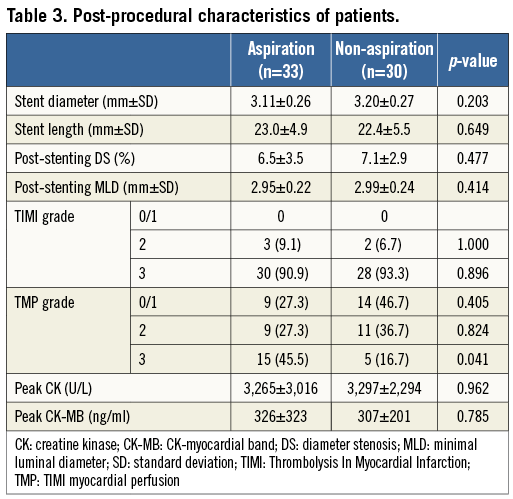
ANGIOGRAPHIC AND PERIPROCEDURAL FINDINGS
The baseline angiographic characteristics shown in Table 2 did not show significant differences between the two groups. The post-procedural angiographic characteristics and cardiac enzymes shown in Table 3 did not show any significant differences between the groups. However, the rate of post-PCI TMPG 3 was higher in the aspiration group than in the non-aspiration group (45.5% vs. 16.7%, p=0.041) (Table 3). The intraobserver and the interobserver variability of post-PCI TMPG were measured and kappa values were 0.773 and 0.707, respectively.
PHYSIOLOGIC AND ECHOCARDIOGRAPHIC FINDINGS
Echocardiographic findings are shown in Table 4. No significant differences in baseline EF (47.3±8.5% vs. 49.5±7.8%, p=0.281), baseline WMSI (1.45±0.31 vs. 1.37±0.27, p=0.299), follow-up EF (50.6±8.7% vs. 50.3±7.2%, p=0.856), and follow-up WMSI (1.33±0.30 vs. 1.36±0.28, p=0.600) were observed between the two groups. However, there were significant differences in ∆EF (follow-up EF - baseline EF; 3.33±4.6% vs. 0.73±1.9%, p=0.005), ∆WMSI (follow-up WMSI - baseline WMSI; –0.121±0.16 vs. –0.004±0.07, p=0.001). The mean IMR of 63 patients after primary PCI was 28.6 U. The IMR in the aspiration group was significantly lower than in the non-aspiration group (23.5±10.2 U vs. 34.2±21.7 U, p=0.018; Figure 1). The correlation coefficients of the intraobserver and the interobserver variability on follow-up EF were 0.915 and 0.905, respectively. Also, the correlation coefficients of the intraobserver and the interobserver variability on follow-up WMSI were 0.929 and 0.917, respectively.
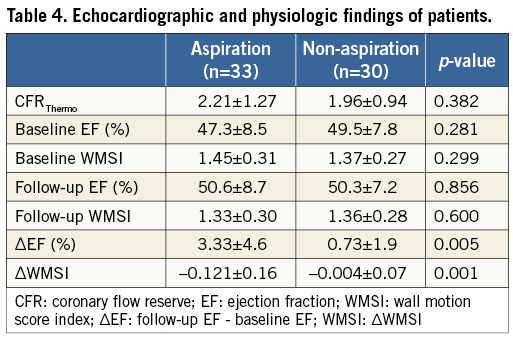
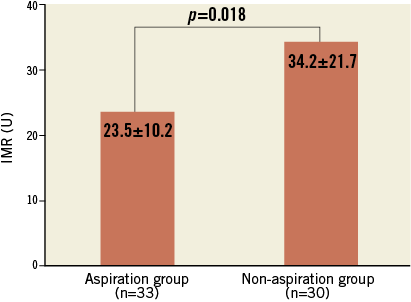
Figure 1. Comparison of the IMR between the two groups. The IMR in the aspiration group is significantly lower than that in the non-aspiration group.
Discussion
Previous studies have demonstrated that manual thrombus aspiration improves myocardial reperfusion and preserves microvascular integrity in acute myocardial infarction (AMI)5,7,19. To our knowledge, this is the first report evaluating the effect of manual thrombus aspiration to preserve IMR during primary PCI.
In patients with AMI, TMPG-based impaired perfusion of the myocardium on coronary angiography is related to a high mortality risk16. The present study, however, showed higher frequency of TMPG 3 after manual thrombus aspiration compared with conventional PCI in patients with STEMI. Thrombus aspiration is known to reduce thrombotic complications associated with the distal embolisation. Therefore, less distal embolisation may improve myocardial perfusion and left ventricular function19-21. In addition, it is well known that intracoronary thrombi are mixtures of white clots composed of platelets and red clots composed of fibrin and red blood cells19. Because currently used antiplatelet agents target white clots, thrombus aspiration is a valuable adjunct method during primary PCI. A large thrombus burden has been associated with stent thrombosis and poor outcomes at clinical follow-up22. Thrombus aspiration could improve myocardial reperfusion and decrease the size of infarcts, which is probably related to a protective effect of thrombus aspiration on microvascular damage7. Lipiecke et al reported that thrombus aspiration as an adjunctive therapy in high-risk patients with AMI did not decrease infarct size and did not have any effect on left ventricular function23. However, in our study, at six-month follow-up, EF increased by 3.33% in the aspiration group and by 0.73% in the non-aspiration group, while WMSI decreased by 0.121 in the aspiration group and by 0.004 in the non-aspiration group.
Manual thrombus aspiration has some benefits, such as similar time of fluoroscopy, similar door-to-balloon time, and a very low rate of device-related complications19. IMR correlates very well with microvascular resistance and presents microcirculatory function without being influenced by the presence of an epicardial coronary artery stenosis9. Further, IMR is a better predictor of microvascular damage and is a reliable early on-site determinant of myocardial viability and left ventricular recovery after primary PCI for AMI patients11,24. Previous studies have reported that the optimal cut-off value of the IMR for left ventricular recovery ranges from 32 to 33 U11,24. Lim et al reported that the mean IMR was 34 U in anterior AMI patients, and those patients were treated by conventional PCI24. In our study, the mean IMR was 34.2 U in the non-aspiration group, whereas the mean IMR was 23.5 U in the aspiration group. These results suggest that microvascular damage can be reduced by using manual thrombus aspiration in primary PCI.
Fearon et al reported that the IMR measured after primary PCI predicted left ventricular function as assessed by measuring a wall motion score from echocardiography at three-month follow-up. In our study, IMR in the aspiration group was lower than that in the non-aspiration group: the left ventricular function measured via EF and WMSI from echocardiography at the six-month follow-up was significantly improved in the aspiration group. Although our results did not show clinical differences between the two groups, the lower IMR value in the aspiration group possibly reflects recovery of left ventricular function5,7.
In this study, abciximab was not administered. Many studies have shown that abciximab administration reduces the occurrence of major adverse cardiac events and improves LV function and perfusion at the microvascular level compared with conventional PCI in patients with AMI25. Up until now, the synergic effect of thrombus aspiration and abciximab administration was not known in primary PCI at the microvascular level, so further studies are needed.
Limitations
First, the small sample size was a limitation in this study. Second, our study has limited power to evaluate the effect of thrombus aspiration on clinical outcomes because of the limited number of samples. Third, the clinical significance of a lower level IMR in the aspiration group has not been proven because no significant clinical differences were observed between the two groups. Fourth, the IMR in the left anterior descending artery may be different from that in the right coronary artery (RCA), but this finding does not have a significant impact when assessing IMR in STEMI patients. Fifth, because patients with cardiogenic shock were excluded, this study cannot represent all variations of STEMI. Therefore, an increased number of patients in a future randomised study would make sure that this important difference is levelled out.
Conclusions
IMR is a simple quantitative technique for assessing microvascular dysfunction in primary PCI. Compared with conventional PCI, manual thrombus aspiration as an adjunctive method to primary PCI for STEMI may preserve microvascular integrity and have beneficial effects on myocardial microcirculation.
|
Conflict of interest statement
The authors have no conflicts of interest to declare.