Abstract
Aims: Although the benefit of concomitant thrombus aspiration (TA) in primary percutaneous coronary intervention (PPCI) treatment of acute ST-segment elevation myocardial infarction (STEMI) has been demonstrated, very little information is available on its safety as a lone revascularisation technique in this setting. We present our experience in a cohort of patients with STEMI treated only with TA, without concomitant interventional devices.
Methods and results: In 28 patients with STEMI, PPCI was performed using only TA on the grounds of an excellent angiographic result and in order to avoid the potential risks associated with balloon dilatation or stenting. The patients were younger than in the overall PPCI population (n=1,737) at our institution (52±18 vs. 63±14 years, p<0.001), with a history of atrial fibrillation in six (21%), cocaine abuse in three (11%) and mechanical cardiac valves in two (7%). Twenty-eight patients (89%) presented STEMI with Killip class I, two (7%) with cardiogenic shock, and two (7%) with sudden cardiac death. A significant reduction in TIMI thrombus grade (5 [4-5] to 1 [0-1.75], p<0.001) and coronary stenosis percentage (%) (87.2±21.3 to 11.3±0.9, p<0.001) as well as an increase in final TIMI flow (0 [0-2] to 3 [3-3], p<0.001) and minimum luminal diameter (mm) (0.89±1.01 to 2.42±0.70, p<0.001) were noted after TA. Transient no-reflow phenomenon, residual intracoronary thrombus and minor distal thrombus embolisation were observed in two (7.1%), 11 (39.3%) and 10 (25.7%) patients, respectively. All but one patient remained asymptomatic during hospital admission. Scheduled control angiography was performed 6±2 days (min-max, 3-10 days) after PPCI in 11 (39%) patients, demonstrating coronary artery patency and TIMI flow grade 3 in all patients. During clinical follow-up, successfully performed in all patients at 40±23 months (min-max, six to 95 months), there was one sudden cardiac death (4%) and three (11%) non-cardiac deaths. One patient (4%) was admitted with non-STEMI (new coronary angiogram without stenosis) and the remaining 22 (78.5%) remained asymptomatic and free of cardiac events.
Conclusions: Our series suggests that lone TA might be safely performed as a primary revascularisation procedure in STEMI in selected cases. Further information based on additional and larger studies is recommended to confirm our findings.
Introduction
Intracoronary thrombus increases the complication rate of percutaneous coronary intervention (PCI) in acute coronary syndromes, including acute myocardial infarction1-4. Thrombus aspiration (TA) has emerged as a valuable tool in avoiding distal thrombus embolisation and no-reflow phenomenon during primary PCI (PPCI), improving final TIMI flow, myocardial blush grade and, most importantly, clinical outcomes5-9. On these grounds, the use of TA has been recommended in clinical practice guidelines (Class IIa recommendation)10.
The standard PPCI procedure in ST-elevation myocardial infarction (STEMI) includes TA followed by balloon dilation if required and, finally, coronary stenting. The rationale behind this sequence is restoration of epicardial and microcirculatory flow and improvement in luminal geometry and haemorrheology at the culprit location. However, this sequence of treatment can be questioned in situations where TA has rendered an optimal result as assessed by angiography or intracoronary imaging, particularly when additional balloon dilation or stenting may be associated with additional risks (like major side branch jailing), where an absolute contraindication to antiplatelet therapy is present or where the suspicion of a non-atherosclerotic cause of myocardial infarction exists. In these situations, the long-term benefit-risk ratio of limiting PCI revascularisation to lone thrombus aspiration is currently unknown.
In this study, we investigated the safety of a strategy of lone thrombus aspiration, without added balloon dilation or stenting, in selected STEMI patients in whom TA resulted in successful restoration of epicardial flow and no significant residual stenosis was observed.
Methods
Out of 1,737 consecutive primary PCI procedures performed at our institution between June 2004 and August 2011, 757 (43.5%) were performed with TA. In 28 cases (3.7% of all TA procedures), the procedure was limited by the operator to lone thrombus aspiration due to achievement of an excellent angiographic result, defined as: 1) restoration of TIMI flow grade 311; 2) residual TIMI thrombus grade ≤312; 3) absence of a residual significant stenosis; and 4) absence of significant distal thrombus embolisation. These patients constituted our study population.
Recorded clinical variables included: age, gender, smoking, hypertension, diabetes, dyslipidaemia, personal or family history of coronary heart disease (CAD) and all medical charts were reviewed.
Coronary angiograms were analysed before and after TA. Coronary flow was assessed with the thrombolysis in myocardial infarction (TIMI) flow grade classification11: TIMI 0, absence of any antegrade flow beyond the coronary occlusion; TIMI 1, antegrade coronary flow beyond the occlusion although filling of the distal coronary bed is incomplete; TIMI 2, delayed antegrade flow with complete filling of the distal territory, and TIMI 3, normal flow and filling of the distal artery. Intracoronary thrombus burden was assessed using the TIMI thrombus grade (TTG) classification12: grade 0, no thrombus; grade 1, possible thrombus is present; grade 2, definite thrombus, with greatest dimensions ≤1/2 the vessel diameter; grade 3, definite thrombus, but with greatest linear dimension >1/2 but <2 vessel diameters; grade 4, definite thrombus with the largest dimension ≥2 vessel diameters, and grade 5, total occlusion. Quantitative angiographic analysis was performed using the CAAS II system (Pie Medical Imaging, Maastricht, The Netherlands). Angiographic complications reviewed were: distal embolisation, no-reflow phenomenon, coronary dissection and coronary perforation.
STEMI was defined and treated according to current clinical practice guidelines13. In-hospital evolution reviewed included recurrent angina, haemodynamic instability, urgent revascularisation or haemorrhagic complications. Clinical follow-up was performed reviewing all medical charts and via telephone interview.
Continuous variables are expressed as mean±SD or median (25th-75th), as appropriate. Categorical variables are expressed as percentages. The distribution of the quantitative variables was assessed with the Kolmogorov-Smirnov test. Continuous variables were compared with t-test or Mann-Whitney U test, as appropriate. A paired t-test or Wilcoxon test was used to compare angiographic differences before and after TA. The Kaplan-Meier statistical method was used to generate survival curves. All calculations were considered to be significant in the presence of a p-value <0.05. The SPSS 20.0 (SPSS Inc., Chicago, IL, USA) statistical software package was used for all calculations.
Results
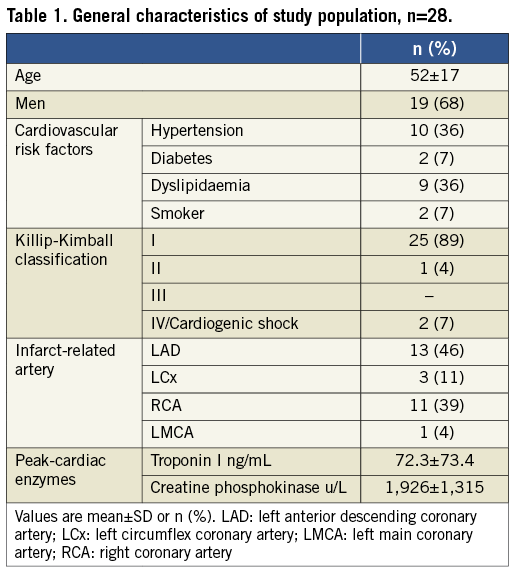
Patient demographics are shown in Table 1. The 28 patients treated with lone TA were younger than the overall PPCI population (52±18 vs. 63±14 years, p<0.001) and, in total, 21 patients (75%) were less than 70 years old. No differences in gender, diabetes, hypertension or dyslipidaemia with the overall PPCI population were found. Smoking prevalence was lower (7%) than in the overall PPCI population (30%, p=0.0058). Myocardial infarction size as assessed by peak CK rise (1,926±1,315 UI) was similar to that in the overall PPCI group (2,271±2,091 UI).
Seven patients (25%) had a previous diagnosis of arrhythmia, atrial fibrillation being the most common; paroxysmal in two (7%) and chronic in four (14%). Three (11%) reported cocaine abuse, two had mechanical valves (non-therapeutic INR values in both cases), one had HIV infection and was under highly active antiretroviral therapy, another received a renal transplant, one had a strong family history of protein C deficiency and, finally, two developed in-hospital STEMI after being admitted due to gastrointestinal bleeding (both patients in atrial fibrillation).
All patients had on-going chest pain and persistent ST-segment elevation immediately before coronary angiography. Prior to PPCI, five patients (18%) received pharmacological thrombolysis without reperfusion criteria. Most patients presented in Killip-Kimball class I. Two patients presented out-of-hospital cardiac arrest. Adjunctive treatment included antithrombotic and antiplatelet therapy (100% aspirin, 93% clopidogrel, 89% glycoprotein IIb/IIIa inhibitors, 48% unfractionated heparin and the remainder 52% with enoxaparin), lipid lowering agents, beta-blockers and angiotensin-converting enzyme inhibitors according to standard practice.
Large intracoronary thrombus was documented in all patients. Mean culprit vessel diameter was 3.3±0.8 mm, with occlusion in 18 (64%). The left anterior descending (LAD) was the most frequent culprit artery. Two patients had two-vessel disease. Coronary aneurisms were found in two patients (right and circumflex coronary artery, respectively), one an ectatic vessel and in two cases with thrombus in the RCA. Finally, one patient had a LAD to pulmonary artery fistula.
Thrombus aspiration was performed with the following systems: Export® AP catheter (Medtronic, Minneapolis, MN, USA) in 20 patients (71%), Pronto® V3 catheter (Vascular Solutions Inc., Minneapolis, MN, USA) in four (14%), ThromCAT® system (Spectranetics Inc., Colorado Springs, CO, USA) in two and, finally, a Diver (Invatec S.p.a., Roncadelle, Italy) and Rescue system (Boston Scientific, Natick, MA, USA) in one patient/each. A FilterWire EX™ system (Boston Scientific) was used in a patient treated with the Export AP catheter.
Angiographic thrombus burden modification with TA is shown in Table 2. A significant reduction in TIMI thrombus grade (5 [4-5] to 1 [0-1.75], p<0.001) and coronary stenosis percentage as well as an increase in final TIMI flow (0 [0-2] to 3 [3-3], p<0.001) and minimum lumen diameter were noted after TA (Figure 1). In five, TA was performed in two branches rising from a bifurcation (Figure 2). Transient no-reflow phenomenon, residual intracoronary thrombosis and non-clinically significant thrombus embolisation were observed in two (7%), 11 (39%) and 10 (26%) patients, respectively. Intracoronary imaging was performed to ensure the results of TA in six (21%) patients: intravascular ultrasound (IVUS) in four (14%) and optical coherence tomography (OCT) in two (7%) (Figure 3 and Figure 4).
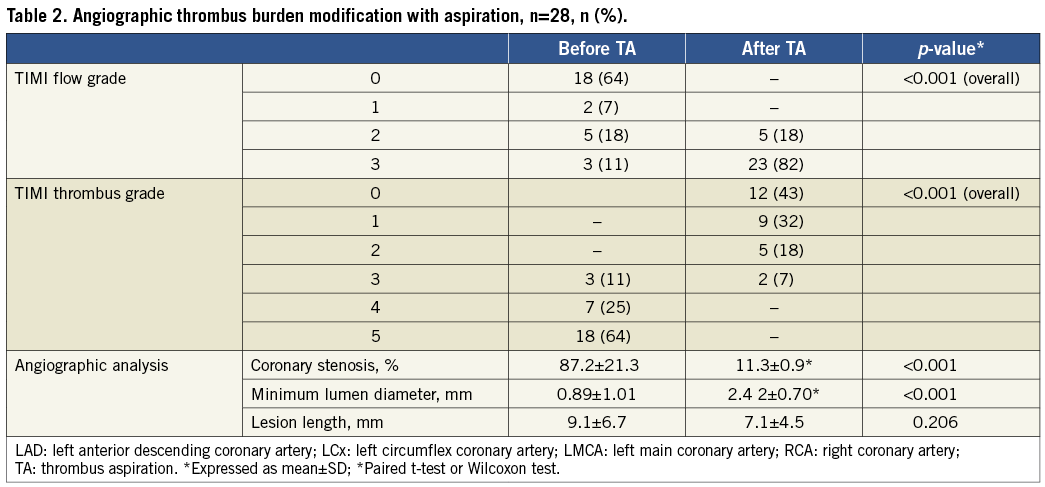
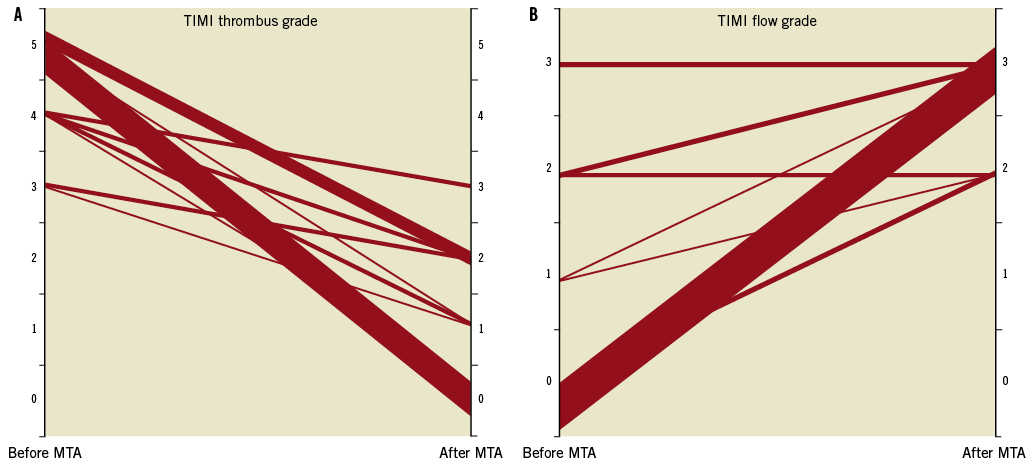
Figure 1. Influence of thrombus aspiration (TA) on TIMI flow grade and TIMI thrombus grade. A) shows changes in TIMI flow grade and (B) shows changes produced in TIMI thrombus grade. In both panels the diameter of the connector is proportional to the number of patients undergoing each situation.
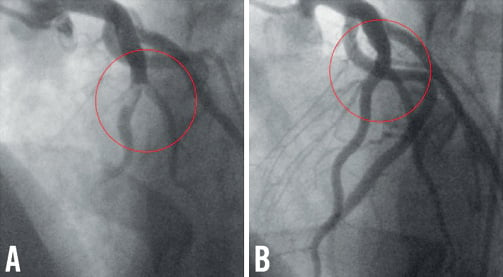
Figure 2. Coronary angiogram before and after thrombus aspiration. A) Coronary angiography revealing grade 4 intracoronary thrombus in both left anterior descending artery and first diagonal branch. Stenting might cause compromise side branch patency or require double-stent techniques. B) Coronary angiography after thrombus aspiration showing effective epicardial flow restoration, absence of distal significant embolisation or an angiographically significant culprit lesion.
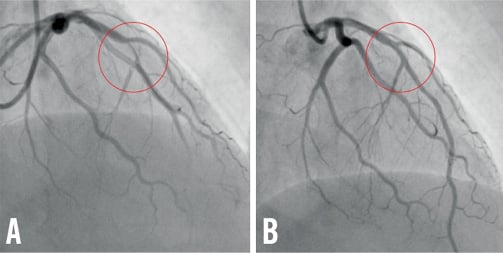
Figure 3. Coronary angiogram of one of the patients included in the study before and immediately after thrombus aspiration. A) Coronary angiography depicting a significant flow-obstructing lesion in the left anterior descending artery (LAD) suggestive of grade 4 intracoronary thrombus with anterograde flow impairment (TIMI 2). B) Coronary angiography after thrombus aspiration showing flow restoration and absence of a significant stenosis.
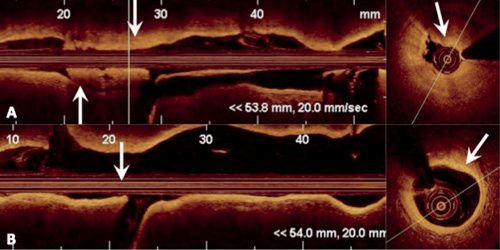
Figure 4. Optical coherence tomography images before and 48 hours after thrombus aspiration. (Same patient as in Figure 3). This figure shows optical coherence tomography images before, and after thrombus aspiration plus 48 hours of antithrombotic and antiplatelet treatment. After the first passage of the aspiration device (A), a large intracoronary thrombus is observed occluding the vessel (top row arrows). After repeated passages of the aspiration device (B), an almost total thrombus aspiration was achieved and a non-obstructive fibrous underlying plaque without ulceration was observed (inferior row arrows).
In hospital, all patients but one remained asymptomatic. An immediate control angiogram for coronary artery assessment was performed in 11 patients (39%) 6±2 days (min-max, 3-10 days). Coronary artery patency and TIMI flow grade 3 were preserved in all patients. In four, residual TTG-1 thrombus was observed but no further TA was attempted. In one case, residual stenosis was thought to be significant (QCA 50%) and thus elective stent implantation was successfully performed. One patient died in hospital of non-cardiac cause (sepsis). The remaining 26 patients (93%) evolved favourably without cardiac symptoms until hospital discharge, with a significant improvement in left ventricular ejection fraction (%) (46±13 to 51±13, p<0.001).
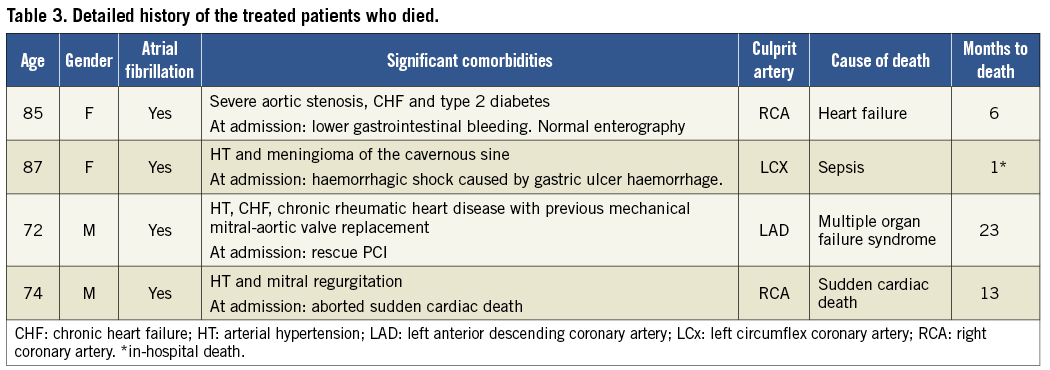
Clinical follow-up was successfully performed in all remaining 26 patients at 40±23 months (min-max, six to 95 months) after hospital discharge (Figure 5). During follow-up three patients (12%) had died: two of documented non-cardiac causes and one presented sudden death 375 days after PCI. This patient had a nine-month follow-up evaluation that included a treadmill exercise test (negative) and a control coronary angiogram showing no coronary stenoses. Detailed information of the patients who died during follow-up is shown in Table 3. One patient was admitted with NSTEMI (new coronary angiogram without stenosis) and the remaining 22 patients (85%) remained asymptomatic and free of cardiac events. Remarkably, two patients developed atrial fibrillation during follow-up.
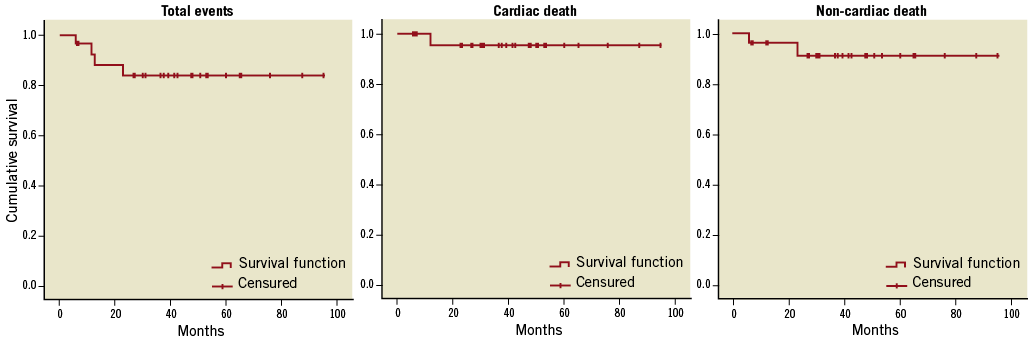
Figure 5. Kaplan-Meier survival estimates. Kaplan-Meier estimates for overall survival and events documented in the study follow-up.
Late scheduled angiographic follow-up was performed in seven cases (27%) at 9±14.2 months (min-max, 1-36 months). In all cases persistently good results, obtained with lone TA at the culprit stenosis location, were documented.
Discussion
Our clinical series suggests that, in selected STEMI patients, TA can be used safely as a lone revascularisation technique during PPCI, without subsequent balloon dilation or stent implantation, provided that an excellent result, as judged by angiography or intracoronary imaging, is obtained. In the following paragraphs these aspects will be discussed in detail.
The TAPAS trial and other studies demonstrated that TA is associated with improved myocardial perfusion, left ventricular function and clinical outcomes in patients with STEMI treated with PPCI6,8,9,14,15. The rationale behind those studies was that, by aspirating friable fractions of the occlusive thrombus, distal coronary embolisation and microcirculatory impairment is less likely to occur during subsequent balloon dilation or stenting. Although these studies did not emphasise obtaining a complete resolution of the culprit stenosis, in clinical practice it is not infrequent that TA yields a complete disappearance of the culprit coronary obstruction, as judged with angiography.
This observation becomes particularly relevant when reasons to avoid stenting are present in the individual patient, firstly in cases in which the aetiology of thrombotic occlusion might be primarily due to non-atherosclerotic causes (and that may occur in 4% to 7% of all patients presenting with STEMI)16. Aetiologies that should be taken into consideration include embolism17-21, pro-thrombotic states related to malignancy22, and acute endothelial dysfunction related to drug intake (cocaine)23-25. Secondly, a number of patients presenting with STEMI have contraindications for sustained antiplatelet therapy due to concomitant bleeding risks (up to 7% of diabetic patients)26. Thirdly, there are cases where stenting the culprit site has associated procedural risks, such as in bifurcation or ostial locations which, in the context of acute coronary syndromes, have been identified as a predictor of future stent thrombosis27. Finally, recent studies have shown that between 4% to 22% of infarct-related arteries occur in non-significant obstructive plaques (<50%) (this number may rise to 22% in young men and 34% in young women)28-30. In these cases, the long-term risk/benefit ratio of ending PCI with stenting vs. passivation of the plaque with intense medical treatment has not been correctly addressed in the literature, as discussed in the next paragraph.
An obvious concern for the interventionalist is whether, in these cases, limiting revascularisation technique to TA is safe. Current standard practice in PPCI includes adjunctive antiplatelet/antithrombotic treatment and thrombus aspiration followed by angioplasty and/or stent implantation. A tacit assumption is that stenting, followed by the development of a neointimal layer, will seal ulcerated atheroma, contributing to passivation of the culprit coronary stenosis and to improved clinical outcomes. However, this has not been demonstrated, and studies like the CADILLAC trial did not identify differences in reinfarction between the balloon and the stent treatment arms that received concomitant IIb/IIIa antiplatelet treatment31. The latter aspect emphasises the key role of adequate antithrombotic treatment in STEMI patients.
Current medical therapy of STEMI (aspirin, thienopyridines, GP IIb/IIIa inhibitor, heparin, etc.) contributes to passivation of the plaque, reduction of thrombus volume and prevention of re-thrombosis/re-occlusion. Also, the widespread use of statins and optimised medical therapy in coronary artery disease, acting on plaque stabilisation, has demonstrated significant improvements in clinical outcomes32,33. In this regard, the PROSPECT trial (a prospective natural-history study of coronary atherosclerosis)32 provided indirect evidence on the safety of medical management of patients with a high-risk atheroma in patients with acute coronary syndromes, as established with virtual histology-intravascular ultrasound. Remarkably, the three-year cumulative rate of major adverse cardiovascular events was nearly equally divided between events related to lesions initially treated and those related to previously untreated lesions, suggesting that untreated plaques might stabilise with intensive treatment32.
Although limited in size, our series supports the concept that TA can be safely used in selected patients. At the present time, only two studies34,35 and some isolated case reports36,37 have addressed clinical outcomes in these circumstances. Fokkema et al proposed, with a report of five cases, that, when thrombus aspiration results in complete restoration of epicardial blood flow without significant residual stenosis or signs of plaque rupture, additional angioplasty with balloon or stent placement may not be necessary35. At one-year follow-up and also, as in our series, three-year follow-up, all patients remained asymptomatic and free of cardiovascular events linked with obstructive atherosclerosis. This indicates that thrombus aspiration as a standalone therapy was safe and effective in these patients. A similar approach, in which PPCI was stopped as soon as coronary flow was re-established and further intervention was only performed in the presence of significant residual stenosis at early follow-up, has recently been proposed with good short-term outcomes re-emphasising the concept that in selected STEMI patients stenting may not be necessary38.
In order to place our findings in proper perspective, some limitations of our study should be taken into account. First, our study was designed to investigate clinical outcomes in patients in whom lone TA resulted in complete flow restoration with small residual luminal narrowing and without significant thrombus embolisation. Consequently, any generalisation of our results to the overall population of patients undergoing PPCI would be inappropriate. Second, our small sample size and the fact that all interventions were performed at the discretion of the operator produce significant limitations when drawing conclusions. Finally, as a single-centre experience the external reproducibility of our findings has to be challenged.
Conclusions
Our results suggest that, in selected patients undergoing PPCI in whom an optimal result (as assessed with angiography or intracoronary techniques) has been obtained with TA, additional stenting can be avoided, particularly in cases in which the operator considers that the potential benefit conferred by stenting might be outweighed by anatomical or clinical characteristics (risk of side branch compromise in bifurcations, concomitant oral anticoagulation, concomitant malignancy, etc.). Further studies are needed to address the safety and efficacy of lone TA in selected STEMI patients.
Conflicts of interest statement
The authors have no conflicts of interest to declare.

