In this chapter of Tools & Techniques, methods of thrombus management in the treatment of ST elevation myocardial infarction (STEMI) are considered and supported by clinical cases. The following is a summarised overview of the chapter. The complete, unabridged version with images is available online at: http://www.pcronline.com/eurointervention/72nd_issue/A26.
Indications and background
The key to successful treatment of STEMI is restoration of coronary blood flow. Primary percutaneous coronary intervention (PPCI) has been accepted as the gold standard therapy for STEMI. Both pharmacological and mechanical strategies are used to overcome the thrombus associated with the culprit plaque, and minimise its embolic potential.
Most commonly, mechanical intervention for thrombus is focused on extraction of the clot associated with the culprit lesion, thus restoring flow, minimising distal embolisation and associated microvascular obstruction (Figure 1). Concomitant antiplatelet and antithrombotic pharmacology serves to limit thrombus proliferation and ensure continued patency of the stented artery. However, the invasive nature of PPCI combined with aggressive antithrombotic therapy generates a delicate bleeding/thrombotic balance.
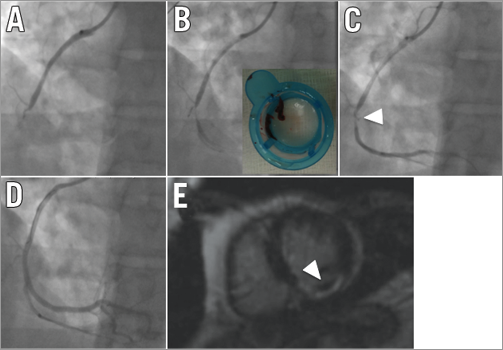
Figure 1. A patient underwent primary PCI for inferior STEMI caused by an acute total occlusion of the mid RCA. A) The coronary wire passage through the occlusion and the aspiration of a fair amount of thrombus (B and inset) resulted in the restoration of TIMI 3 flow (C). Stenting of the culprit lesion (arrowhead) achieved an excellent angiographic result (D). Baseline cardiac magnetic resonance demonstrated microvascular obstruction (white arrowhead - E).
Difficulties
Treatment of a coronary occlusion associated with a heavy burden of thrombus is fraught with difficulty. The operator must always remain vigilant when instrumenting the culprit vessel to avoid embolisation of the clot downstream or upstream into more proximal vessels. Despite thromboaspiration and antithrombotic/antiplatelet therapies, thrombus often persists at the site of a culprit lesion (Figure 2) and raises anxieties regarding the risk of distal embolisation and no-flow following stenting.
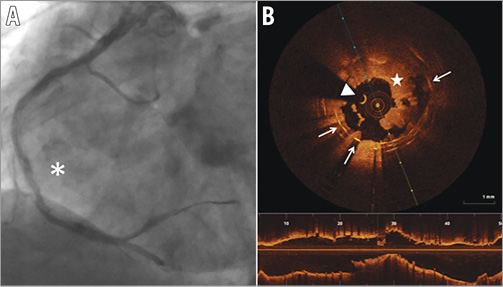
Figure 2. Stent thrombosis. A) Coronary angiogram showing acute stent thrombosis of the right coronary artery (white asterisk). B) Optical coherence tomography image demonstrating the high burden of thrombus associated with the acute stent thrombosis, despite thromboaspiration and administration of antithrombotic agents. A circumferential and almost totally occlusive thrombus is evident (white star), overlying stent struts (white arrows). White arrowhead: guidewire artefact.
Methods
The purpose of this educational review is to highlight the potential pitfalls of STEMI percutaneous coronary intervention in the presence of thrombus and offer tips and tricks to achieve an optimal outcome for patients. We have provided case examples to illustrate the application of the tools & techniques and generate discussion and comment through the EuroIntervention website.
The tools & techniques for thrombus treatment in STEMI include:
– Arterial access selection
-Intervention for STEMI often highlights the delicate balance existing between thrombosis and bleeding. Radial access selection has been demonstrated to offer benefit and allows the interventionist greater freedom in selecting antithrombotic and antiplatelet therapies.
– Thrombus extraction
-Thrombus aspiration.
Thromboaspiration is widely accepted as an integral element of STEMI PCI. Despite the intuitive benefit of thrombus extraction, the technique is associated with the potential risk of proximal and distal embolism. The pitfalls and potential strategies to avoid complication of the technique are detailed in the online version.
-Mechanical thrombus extraction.
The thrombotic burden can exceed the capability of thromboaspiration and consequently selective cases may benefit from the use of extraction devices utilising high-pressure saline jets, laser, or mechanical thrombus disruption. We illustrate their potential role through review of challenging clinical cases.
– Distal protection
– Pharmacology
-Multiple therapeutic targets for the acute treatment of thrombus exist, in the setting of STEMI. We outline the role of periprocedural glycoprotein IIb/IIIa receptor inhibition, intracoronary thrombolysis and perfusion strategies in the treatment of STEMI complicated by thrombus.
– Stenting technique and selection
-The direct stenting technique, covered stent and self-expanding stent technology all offer potential advantages in minimising embolisation of thrombus and plaque material during acute intervention.
The online version of this paper provides a more detailed, in-depth description of each aspect of thrombus management in STEMI.
Conflict of interest statement
The authors have no conflicts of interest to declare.

