- angiography
- coronary flow
- STEMI
- myocardial necrosis
Abstract
Aims: To assess the impact of reperfusion after primary percutaneous coronary intervention (PCI) on myocardial salvage and outcome of patients with acute ST-segment elevation myocardial infarction (STEMI).
Methods and results: This study included 1,406 patients with STEMI undergoing primary PCI. Blood flow restoration at epicardial and tissue levels was assessed by Thrombolysis in Myocardial Infarction (TIMI) and myocardial perfusion grade (MPG). Patients had paired scintigraphic examinations before, and 7-14 days after intervention. Based on TIMI and MPG grades, patients were divided into three groups: patients with optimal epicardial/optimal tissue perfusion (TIMI=3/MPG=3; n=801), patients with optimal epicardial/suboptimal tissue reperfusion (TIMI=3/MPG≤2; n=412) and patients with suboptimal epicardial/suboptimal tissue reperfusion (TIMI≤2/MPG≤2; n=193). In these groups, the median infarct size (25th-75th quartiles) in the 7-14 days scintigraphy was: 7.0% (1.0%-19.0%), 12.6% (5.0%-27.6%) and 18.7% (10.4%-33.7%) of the left ventricle (p<0.001); frequency of aborted myocardial infarction was: 15.5%, 10.0% and 4.7%, (p<0.001); estimates of 5-year mortality were: 7.8%, 16.0% and 20.1% (adjusted hazard ratio=0.43, 95% confidence interval 0.21-0.89; p=0.02 for optimal epicardial/optimal tissue vs suboptimal epicardial/suboptimal tissue reperfusion).
Conclusions: In patients with STEMI undergoing primary PCI, restoration of blood flow at epicardial and tissue levels was associated with increased myocardial salvage and improved long-term survival.
Introduction
The aim of any reperfusion therapy in patients with acute ST-segment elevation myocardial infarction (STEMI) is the prompt reopening of the occluded coronary artery which restores blood flow in the infarct-related artery and salvages ischaemic myocardium1. With the use of percutaneous coronary intervention (PCI) as a primary reperfusion therapy, full restoration of epicardial blood flow is achieved in close to 95% of STEMI patients2. Restoration of the epicardial blood flow, however, does not necessarily mean restoration of reperfusion at the microcirculation or tissue level. Even in patients with restoration of Thrombolysis in Myocardial Infraction (TIMI) flow grade of 3 at the epicardial level of the infarct-related artery, the tissue reperfusion as assessed by myocardial perfusion grade (MPG) 3 was restored in 17.4% to 66.0% of the patients3,4. Most of studies investigating reperfusion at the epicardial or tissue levels or the impact of reperfusion on clinical outcome were performed before the use of current antithrombotic therapy (as peri-PCI and maintenance therapy), known to exert beneficial effects on reperfusion and clinical outcome. The intricate relationship between reperfusion at epicardial artery and tissue levels is poorly understood. Furthermore, in patients with restored tissue reperfusion (MPG 3), the relationship between functional status of microcirculation and the viability of surrounding working myocardium is largely unknown.
We undertook this study to investigate the impact of restoration of blood flow with primary PCI at the epicardial and tissue levels on myocardial salvage, frequency of aborted myocardial infarction, left ventricular ejection fraction and long-term major adverse cardiac events.
Methods
Patients
The study included 1,406 patients with STEMI admitted within the first 24 hours from the symptom onset and treated with PCI in two German hospitals from January 2002 through December 2007. Details of the source sample and the inclusion/exclusion criteria are published in a previous study from our group5. The diagnosis of STEMI required: chest pain lasting ≥20 minutes and ST segment elevation of ≥1 mm in at least two extremity electrocardiographic leads or ≥2 mm in at least two contiguous precordial leads or left bundle branch block of new onset. Heart failure in acute stage of STEMI was classified according to Killip classification6.
Angiographic examination and primary PCI
A culprit lesion was described in the presence of an acute occlusion, intraluminal filling defects (or thrombus), ulcerated plaques with contrast-filled pocket protruding into plaque with or without delayed contrast wash-out, extra-luminal contrast, dissection or intraluminal flaps7. Coronary artery disease in coronary arteries other than infarct-related artery was defined as coronary stenoses ≥50% lumen obstruction. Blood flow in the epicardial coronary arteries and myocardial perfusion grade (MPG) were graded according to the Thrombolysis in Myocardial Infarction (TIMI) Group criteria8. TIMI flow grade 3 and MPG 3 were considered as restoration of optimal blood flow at the epicardial coronary artery and tissue levels, respectively. Based on the prior studies3,4, TIMI flow grades 0-2 and MPG 0-2 were grouped together and were considered to represent suboptimal blood flow restoration at the epicardial artery or tissue levels. The left ventricular ejection fraction (LVEF) was measured on left ventricular angiograms using the area-length method9.
Primary PCI and periprocedural care were performed according to the standard criteria. Stents were used in 88% of patients (n=1,230). Antithrombotic treatment consisted of clopidogrel (600mg as a loading dose followed by 75mg/day for at least four weeks) and aspirin (200mg/day continued indefinitely).
SPECT imaging
Two single photon emission computed tomography (SPECT) images with 99mTc-sestamibi were performed before and 10 days after (range seven to 14 days) primary PCI procedure. Initial perfusion defect (area at risk before primary PCI) and final infarct size (perfusion defect in the second SPECT imaging after primary PCI) were determined according to previously described methods5. The defect size was defined as the <50% uptake area. The salvage index was calculated as the difference between initial area at risk and final infarct size normalised by initial area at risk and expressed as percentage. This parameter reflects the proportion of initial area at risk salvaged (by intervention or spontaneously occurring). Aborted myocardial infarction was defined as infarct size (perfusion defect in the second SPECT imaging) of 0 in patients with an initial perfusion defect >0 (perfusion defect in the first SPECT imaging) plus normal left ventricular ejection fraction and normal regional wall motion.
ST-segment resolution
A 12-lead electrocardiogram was performed before and 90 to 120 minutes after first balloon inflation. The sum of ST-segment elevation was measured 20ms after the end of the QRS complex in: leadsI, aVL, and V1 through V6 for anterior infarction; leads II, III, aVF for inferior infarction and leads V5 toV6 for lateral infarction. The ST-segment elevation resolution was calculated as the initial sum of ST-segment elevation minus the sum of ST-segment elevation on the second ECG divided by the initial sum of ST-segment elevation and expressed as a percentage.
Study outcomes and details of follow-up
The outcomes of the study are: infarct size, frequency of aborted myocardial infarction, left ventricular systolic function at six months and the 5-year incidence of major adverse cardiovascular events (MACE), defined as a composite of mortality, nonfatal myocardial infarction and target vessel revascularisation. The follow-up information included: a phone call at 30 days, a visit at six months, a phone call at one year and yearly phone calls thereafter. Patients who had cardiac complaints underwent a complete clinical, electrocardiographic and laboratory evaluation. Information on deaths was obtained from hospital records, death certificates or phone contact with relatives of the patient or patients’ referring physicians. The follow-up information was collected by personnel unaware of clinical diagnosis or status of reperfusion at the end of primary PCI.
Statistical analysis
Normality of distribution for continuous variables was tested with a Kolmogorov-Smirnov test. Continuous data with skewed distribution are presented as median (with 25th-75th percentiles) and compared with a Kruskal-Wallis rank-sum test and a Wilcoxon rank-sum test. Categorical variables were compared with a chi-square test. Five-year incidences of mortality, nonfatal myocardial infarction and target vessel revascularisation were estimated by applying the Kaplan-Meier method. Comparison between groups was made with log rank test. The association between status of reperfusion (dichotomised in three categories: optimal epicardial/optimal tissue reperfusion, optimal epicardial/subobtimal tissue reperfusion and suboptimal epicardial/suboptimal tissue perfusion) and all-cause mortality was tested with the Cox proportional hazards model. All parameters of Table1 having a p-value <0.10 plus infarct size in the second SPECT imaging (used instead of peak creatine kinase MB and peak troponin as a more reliable estimate of necrosis) were entered into the model. Analyses were performed using S-plus statistical package (S-PLUS; Insightful Corp, Seattle, WA, USA). Atwo-sided p<0.05 was considered to indicate statistical significance.
Results
Based on the TIMI grade and MPG patients were divided into three groups: patients with optimal epicardial/optimal tissue perfusion (TIMI grade=3, MPG=3; n=801 patients, 57%), patients with optimal epicardial/suboptimal tissue reperfusion (TIMI grade=3, MPG≤2; n=412 patients, 29%) and patients with suboptimal epicardial/suboptimal tissue reperfusion (TIMI grade ≤2, MPG≤2; n=193 patients, 14%).
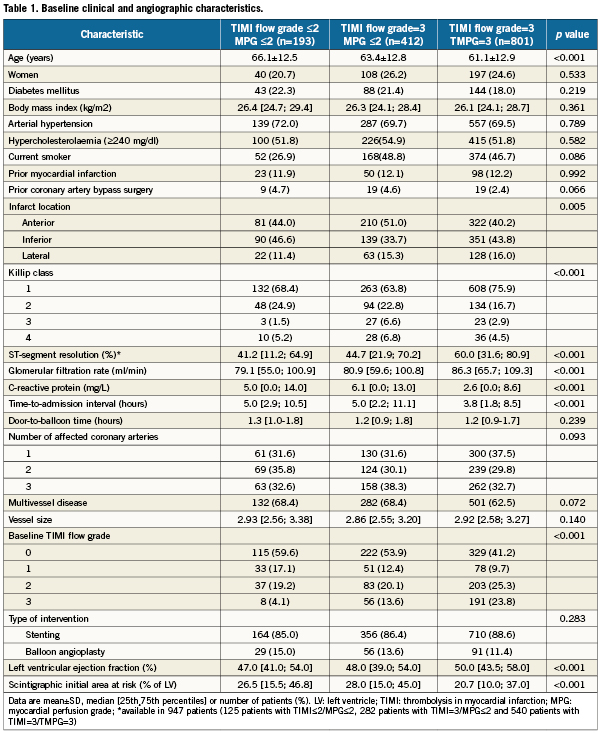
Patients’ characteristics
Baseline characteristics of patients are shown in Table1. Patients with optimal blood flow restoration at both levels were of younger age, were more often in Killip class 1, had a greater degree of ST-segment resolution and better renal function and had lower concentrations of C-reactive protein and shorter time-to-admission intervals than patients of the other two groups. Furthermore, they more often had residual blood flow in the infarct-related artery (baseline TIMI flow grades 2 and 3), better LVEF and smaller initial area at risk in the baseline SPECT imaging. There were differences in the infarct location with anterior infarcts being more frequent among patients with optimal epicardial/suboptimal tissue reperfusion (Table1). Overall time-to-admission, door-to-balloon and time-to-treatment intervals (median and interquartile range) were 4.2 (2.0-9.7) hours, 1.25 (0.88-1.75) hours and 5.8 (3.3-11.2) hours, respectively.
Impact of reperfusion on the markers of myocardial necrosis
Three estimates of the extent of myocardial necrosis – peak creatine kinase MB, peak cardiac troponin T, and scintigraphic infarct size 7-14 days after primary PCI were assessed. In patients with optimal epicardial/optimal tissue, optimal epicardial/suboptimal tissue and suboptimal epicardial/suboptimal tissue reperfusion, peak creatine kinase MB activity (median and interquartile range) was 122.0 (59.1-248.0) U/L, 155.0 (71.7-288.5) U/L and 158 (79.0-291.0) U/L, respectively (P<0.001); peak cardiac troponin was 3.39 (1.43-6.18) µg/L, 4.61 (2.33-8.47) µg/L, 5.14 (2.57-9.12) µg/L, respectively (p<0.001) and scintigraphic infarct size in the 7-14 days SPECT imaging was 7.0% (1.0%-19.0%) of the left ventricle, 13.0% (5.0%-28.0%) of the left ventricle and 17.0% (7.0%-30.0%) of the left ventricle, respectively (p<0.001; Figure1).

Figure 1. The impact of reperfusion at epicardial and/or tissue level on markers of necrosis. CKMB indicates creatine kinase myocardial band; MPG: myocardial perfusion grade; IS: infarct size; TIMI: Thrombolysis In Myocardial Infarction; Data are medians with 25th-75th percentiles.
Myocardial salvage and aborted myocardial infarction
In patients with optimal epicardial/optimal tissue, optimal epicardial/suboptimal tissue and suboptimal epicardial/suboptimal tissue reperfusion, the salvage index (percentage of initial area at risk that was salvaged) was 57.9% (31.5%-85.7%), 45.0% (23.0%-74.8%) and 34.6% (17.8%-55.9%) respectively (p<0.001). There were 174 patients with aborted myocardial infarctions. The proportion of patients with aborted infarctions according to epicardial/tissue reperfusion were 15.5% (n=124) in patients with optimal epicardial/optimal tissue reperfusion, 10.0% (n=41) in patients with optimal epicardial/ suboptimal tissue reperfusion and 4.7% (n=9) in patients with suboptimal epicardial/suboptimal tissue reperfusion, (p<0.001; Figure2). Initial area at risk (perfusion defect in the baseline SPECT imaging) was 13.0% (5.1%-24.5%) of the left ventricle in patients with optimal epicardial/optimal tissue reperfusion, 13.7% (8.0%-25.7%) of the left ventricle in patients with optimal epicardial/suboptimal tissue reperfusion and 16.5% (9.0%-24.0%) of the left ventricle in patients with suboptimal epicardial/suboptimal tissue reperfusion (p=0.820).
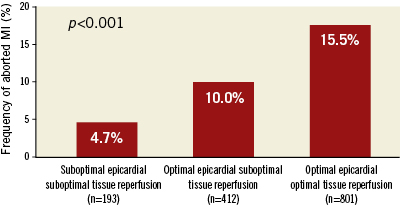
Figure 2. Frequency of aborted myocardial infarction (MI) according to status of reperfusion after primary PCI.
Impact of reperfusion on 6-month left ventricular function
Follow-up angiography was performed in 1,026 patients (73%). Baseline and 6-month LVEF data were available in 976 patients. In patients with optimal epicardial/optimal tissue, optimal epicardial/suboptimal tissue and suboptimal epicardial/suboptimal tissue reperfusion, 6-month LVEF was 55.0% (48.3%-61.0%), 51.0% (43.0%-58.0%), and 51.0% (42.0%-59.0%), respectively (p<0.001; Figure3). Compared to baseline values, patients with suboptimal reperfusion at both levels did not show a significant increase in 6-month LVEF; the other two groups of patients did show a significant increase in LVEF (Table 1; Figure 3).
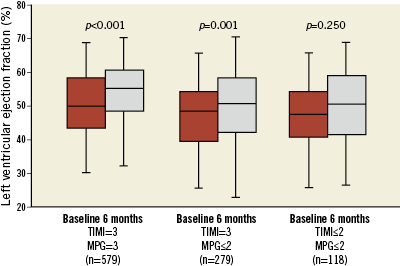
Figure 3. Left ventricular ejection fraction at baseline and six months after primary PCI. Data are medians with 25th-75th and 5th-95th percentiles.
Impact of reperfusion on long-term clinical outcome
The median (interquartile range) follow-up was 1,505 days (751-1,800 days). Overall, there were 132 deaths (of them 90 deaths were of cardiovascular origin) and 47 nonfatal myocardial infarctions. Target vessel revascularisation was needed in 336 patients. Kaplan-Meier estimates of adverse cardiac events during the follow-up are shown in Table2. Among all three components of MACE, mortality showed the strongest association with the status of reperfusion at the end of primary PCI (odds ratio [OR]=3.00, 95% confidence interval [CI] 1.85-4.86, P<0.001 for suboptimal epicardial/suboptimal tissue reperfusion group versus optimal epicardial/optimal tissue reperfusion group and OR=2.31, 95% CI 1.53-3.49, p<0.001 for optimal epicardial/suboptimal tissue reperfusion group versus optimal epicardial/optimal tissue reperfusion group).
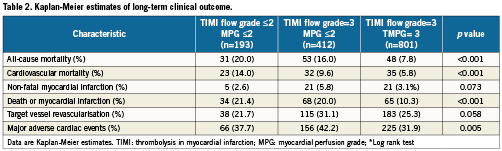
There were 90 deaths of cardiovascular origin (Table 2). Cardiovascular mortality showed a strong association with status of reperfusion at the end of primary PCI (OR=2.96, 95% CI 1.70-5.14, p<0.001 for suboptimal epicardial/suboptimal tissue reperfusion group versus optimal epicardial/optimal tissue reperfusion group and OR=1.84, 95% CI 1.12-3.02, p=0.014 for optimal epicardial/suboptimal tissue reperfusion group versus optimal epicardial/optimal tissue reperfusion group). There were no significant association between status of reperfusion after primary PCI and the incidence of nonfatal myocardial infarction of target vessel revascularisation during follow-up (Table 2).
Because differences in composite endpoints between groups were mainly driven by differences in mortality, the association between status of reperfusion after primary PCI and mortality was tested in the Cox proportional hazards model (see methods for variables entered into the model). The model showed that status of reperfusion was an independent correlate of long-term mortality (hazard ratio=0.43, 95% CI 0.21-0.89; p=0.02 for optimal epicardial/optimal tissue vs. suboptimal epicardial/suboptimal tissue reperfusion; Figure4).
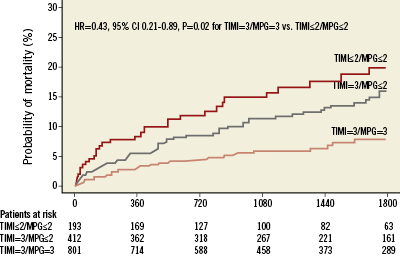
Figure 4. Probability of mortality according to status of reperfusion after primary PCI. HR: hazard ratio; CI: confidence interval; MPG: myocardial perfusion grade; TIMI: thrombolysis in myocardial infarction
Discussion
The main findings of this study are as follows:
1) Primary PCI applied within the time-to-treatment of 5.8 (3.3-11.2) hours and with current periprocedural adjunct antithrombotic therapy, restored an optimal reperfusion at epicardial and tissue levels in 57% of patients. In 29% of patients optimal reperfusion was restored only at epicardial level and in 14% of patients reperfusion was suboptimal at both levels.
2) Restoration of optimal reperfusion at epicardial and tissue levels was associated with increased myocardial salvage, decreased enzymatic and scintigraphic infarct size and increased frequency of aborted myocardial infarction compared with failure to restore reperfusion at one (tissue) or at both levels.
3) Patients with complete (at both levels) or partial (epicardial level) restoration of reperfusion showed an improvement in the left ventricular function six months after primary PCI.
4) Reperfusion status immediately after primary PCI was an independent correlate of long-term mortality but not of nonfatal myocardial infarction or the need for target vessel revascularisation.
The impact or reperfusion status on clinical outcome has been previously addressed in the setting of blush3,10, TIMI flow11,12 and no-reflow4,13 studies. Although epicardial and tissue reperfusion are intricately interrelated, prior studies focused primarily on either the impact of tissue reperfusion (blush studies) or epicardial flow (TIMI studies) on the clinical outcome. In distinction to these studies, in our study the clinical outcome was investigated in groups defined by joint consideration of epicardial and tissue reperfusion as it occurs in reality. In prior studies, intermediate grades of reperfusion (TIMI grade 2 and MPG 2) were considered as either normal or abnormal reperfusion, so the comparison between studies is, at best, rather problematic. Since available evidence strongly suggests that TIMI grade 211,12 and MPG 23,4 are markers of suboptimal reperfusion that signify a poor outcome, in the present study they are considered to represent abnormal reperfusion. Our study reflects the contemporary practice of primary PCI both in terms of intervention type (88% with stenting) and adjunct antithrombotic therapy. Furthermore, the association of reperfusion status after primary PCI with outcome (extent of myocardial necrosis, left ventricular function and major adverse events) was investigated with reliable biochemical and scintigraphic markers over a long-term follow-up.
A prior study by van ‘t Hof et al10 including 777 patients treated with primary angioplasty concluded that myocardial reperfusion can be reliably described by myocardial blush grade which correlated with enzymatic infarct size, left ventricular function and long-term mortality. A retrospective analysis of the CADILLAC (Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications) trial that included 1,301 patients (96.1% with post-primary PCI TIMI grade 3), showed that tissue reperfusion was a powerful correlate of survival and that normal tissue perfusion was achieved only in a minority (17.4%) of patients3. An angiographic analysis performed in 30% of study sample, seven months after the index event, showed an improvement in left ventricular function irrespective of tissue reperfusion grade. Importantly, in this study, patients with MPG 2 had a distinct intermediate survival between those with MPG 0-1 and 3.3 In a study, by Poli at al14, in which left ventricular function was studied with 2D echocardiography, MPG was an independent correlate of late recovery of left ventricular function (6-month) and that the greatest improvement was observed in patients with restored tissue reperfusion (MPG 2-3). Although the present study and the study by Poli et al14 differ with regard to classification of tissue reperfusion, our data seem to corroborate these findings. An interesting study by Hoffmann et al15 showed that tissue reperfusion after primary angioplasty improves over time (7.5±5.6 months) and that patients with recovery of reperfusion had better left ventricular function. In a prior study, we have found that resolution of no-reflow was associated with improvement in the left ventricular function six months after primary PCI16.
As in prior studies3, the present study reported a strong association between status of reperfusion immediately after primary PCI and long-term mortality, possibly due to inherent association of suboptimal reperfusion with infarct size, no-reflow phenomenon and microvascular obstruction, known to be important correlates of increased risk of death in patients with STEMI5. With regard to two other MACE components –nonfatal myocardial infarction and target vessel revascularisation– we found no association with reperfusion status immediately after primary PCI. Although the lack of association is not entirely explainable, the stabilising effects of coronary stents (used in 88% of patients) and contemporary antithrombotic therapy may impact on these events that develop at epicardial artery level more than status of tissue reperfusion, which otherwise impacts heavily on future mortality. On the other hand, stent thrombosis is a rare event17, and restenosis has a relatively benign course18 and may make a mild contribution to mortality.
Finally, finding of myocardial necrosis in patients with restored reperfusion at epicardial and tissue levels may provide information on the relative sensibilities of vascular and working myocardial tissue. The combined use of angiography, able to reveal the functionality of myocardial vasculature, and scintigraphy able to differentiate necrotic from viable myocardium, allows assessment of sensibility of microvasculature and working myocardium to ischaemia. Morphologic studies in dogs by Kloner et al19 have demonstrated that ultra-structural evidence of microvascular damage lagged behind myocardial cell injury by 40 to 50 minutes, suggesting that microvascular tissue is more resistant to ischaemia than working myocardium. Our data in humans seem to support such findings. Microvascular obstruction in the course of myocardial ischaemia implies severe capillary obliteration caused by endothelial swelling, endothelial protrusions, membrane-bound and free floating intraluminal bodies (blebs) and extravascular swelling20. We hypothesise that in patients with restored tissue perfusion, the described microvascular alterations are less manifest indicating preservation of microvascular tissue viability. The demonstration of myocardial necrosis by SPECT imaging in the setting of preserved microvascular function may indicate that ischaemia was long enough to irreversibly damage the more susceptible working myocardium, but not the more resistant microvascular tissue. Apart from showing the presence of myocardial necrosis despite restored tissue reperfusion, our study offers additional support for this hypothesis. First, patients with restored tissue reperfusion had significantly shorter time-to-treatment interval compared to other study groups. Second, patients with restored tissue reperfusion had a higher proportion of patients with spontaneously occurring coronary recanalisation (TIMI grade 2 and 3) at the time of angiography. Both these mechanisms indicate an earlier restoration of blood flow in these patients which might have been early enough to preserve vascular tissue but not working myocardium.
Conclusion
The current practice of primary PCI restored optimal reperfusion at epicardial and tissue levels in 57% of patients. Restoration of optimal reperfusion at epicardial and tissue levels was associated with increased myocardial salvage, decreased scintigraphic infarct size, increased frequency of aborted myocardial infarction and better left ventricular function six months after primary PCI. Reperfusion status immediately after primary PCI impacts on mortality but not on occurrence of nonfatal myocardial infarction or on the need for target vessel revascularisation over long-term follow-up.
Conflicts of interest statement
The authors have no conflicts of interest to declare.