Abstract
Aims: Primary percutaneous coronary intervention (PCI) for ST-elevation myocardial infarction (STEMI) usually restores TIMI 3 flow in the occluded artery, but microvascular impairment may persist in >30% of patients. Less is known about microvascular reperfusion in STEMI patients treated with thrombolysis followed by early PCI. We aimed to assess the association between TIMI myocardial perfusion (TMP) at the end of the PCI procedure and left ventricular function (LVEF) and infarct size after three months in such patients.
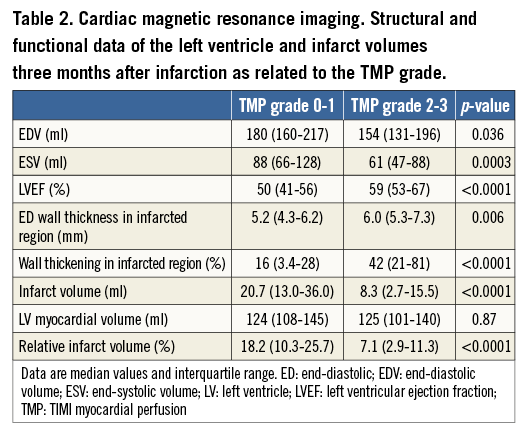
Methods and results: Patients with STEMI treated with thrombolysis and early PCI were included. TMP grade was assessed at the end of the PCI procedure, and MRI was performed after three months. Of the 89 patients included, 92% (n=82) had TIMI 3 flow at the end of the PCI procedure, while only 62% (n=55) had TMP grade 2 or 3. Patients with TMP grade 2-3 had significantly higher LVEF (59% [53-67] vs. 50% [41-56], p<0.0001) and smaller infarct size (8.3 ml [2.7-15.5] vs. 20.7 ml [13.0-36.0], p<0,0001) after three months.
Conclusions: In STEMI patients treated with thrombolysis and early PCI, the TMP grade at the end of the PCI procedure was significantly associated with LVEF and infarct size after three months.
Introduction
Primary percutaneous coronary intervention (PCI) is the preferred reperfusion strategy in ST-elevation myocardial infarction (STEMI), but, in areas with transfer times of more than 90-120 min to PCI, initial thrombolysis remains the treatment of choice1. Immediate transfer for early angioplasty after thrombolytic therapy has been shown to improve outcome compared with thrombolysis alone2, and has shown similar efficacy and safety results to those of primary PCI in areas with long transfer delays3,4.
Angiographic successful reperfusion in STEMI has been defined as TIMI (Thrombolysis In Myocardial Infarction) 3 flow in the epicardial artery5. However, complete restoration of epicardial flow does not necessarily translate into flow restoration on the myocardial level or to microvascular reperfusion, and normal tissue perfusion may be obtained in only 25-55% of the patients6,7. In 1994, the first studies demonstrated a correlation between coronary flow reserve and regional myocardial function on angiography8.
TIMI myocardial perfusion (TMP) grade provides important prognostic information beyond epicardial flow6,7,9-11. Full reperfusion at the myocardial level is as important as restoration of TIMI 3 flow, and is an independent predictor of myocardial function recovery and long-term survival12-14. The importance of myocardial reperfusion in STEMI patients treated by thrombolysis followed by early PCI has previously been assessed by left ventriculography11, and recent studies have indicated that TMP grade correlates with both the presence and the extent of early and late microvascular obstruction (MVO) on magnetic resonance imaging (MRI)15.
Due to its high spatial resolution, high accuracy and reproducibility, MRI is considered the gold standard for measuring left ventricular ejection fraction (LVEF) and volumes16,17. Further, late enhancement imaging 10-30 min after contrast administration offers a precise method to distinguish and quantify the size and transmurality of infarcted myocardium with better sensitivity and reproducibility than echocardiography and scintigraphy16,18.
The aim of this study was to assess the relationship between TMP grade at the end of the PCI procedure and MRI-determined LVEF and infarct size after three months in STEMI patients treated with thrombolysis followed by early PCI.
Methods
PATIENTS AND STUDY DESIGN
This was a pre-specified substudy of the NORwegian study on DIstrict treatment of ST Elevation Myocardial Infarction (NORDISTEMI)19,20. The study design and clinical results have been published previously20. In brief, patients with STEMI of less than 6 hrs duration and more than 90 min expected time delay to primary PCI received full-dose thrombolysis and were randomised to transfer for immediate coronary angiography and intervention if indicated (early invasive group), or managed conservatively in the local hospital. Patients in the conservative group were referred for urgent angiography only if there was persistent chest pain or <50% reduction of ST-segment elevation 60 min after initiation of thrombolysis (rescue indication), or if there was haemodynamic instability. In the present substudy, patients from both groups being treated by thrombolysis followed by early PCI, and being able and willing to undergo cardiac MRI, were included.
TIMI flow was assessed prior to and after the PCI procedure, and TMP grade was assessed at the end of the PCI procedure. All patients were evaluated by MRI after three months.
Reasons for not being able to undergo MRI after three months were death (n=6), disabling stroke, pacemaker, claustrophobia or refusal to make the journey to the imaging centre (100-400 km). Patients with known renal impairment or development of renal dysfunction during hospitalisation were also excluded because of potential toxicity related to gadolinium use21.
All patients provided written informed consent in accordance with the revised Declaration of Helsinki before enrolment. The study was approved by the Regional Ethics Committee for Medical Research and registered at the website www.clinicaltrials.gov, NCT00161005.
CORONARY ANGIOGRAPHY AND TMP GRADE
PCI was performed as a standard procedure. The choice of stent type and the use of glycoprotein IIb/IIIa inhibitors and referral for surgery in case of left main coronary artery disease or serious three-vessel disease were left to the judgement of the operator.
The TMP grade was assessed at the end of the PCI procedure. After intracoronary injection of 200 µg glycerol trinitrate, coronary angiography was performed using Ioversol 350 mg I/ml (Optiray®; Covidien Deutschland GmbH, Neustadt, Germany). The TMP grades were defined as 0 to 3 according to the method of Gibson et al9. For comparison and analysis, patients were divided into two groups in accordance with previous studies14: Group I=TMP grade 0 or 1 and Group II=TMP grade 2 or 3. TMP grading was done by an observer blinded to clinical results.
CARDIAC MAGNETIC RESONANCE IMAGING
Cardiac magnetic resonance imaging was performed in a 1.5T whole-body scanner (Philips Intera; Philips Medical Systems, Best, The Netherlands), using a five-element synergy-cardiac coil as previously described6.
Image analysis was performed on a View Forum workstation (Philips Medical Systems). End-diastolic and end-systolic volumes (EDV, ESV), LVEF and left ventricular myocardial volume were calculated by assessment of the short-axis images. Myocardial first-pass perfusion was analysed by measuring the signal intensity vs. time. Signal intensity was measured in the region of the infarction and in remote, not infarcted myocardium. Maximum contrast enhancement and time to peak were analysed.
Infarct size was assessed in the delayed enhancement images. The infarct volume was reported in ml and as percent of total left ventricular myocardium volume. The cut-off for large infarct size was defined as the 75th percentile in accordance with previous studies22-25. The observer conducting the image analysis was blinded to clinical data. The intraobserver variation coefficients for EDV and LVEF were 2.5 and 3.8%, respectively. The intraobserver variation coefficient for estimation of total infarct volume was 10.2%.
CLINICAL FOLLOW-UP
Cardiovascular events in terms of death, reinfarction, stroke and new ischaemia within the first year after the infarction were collected as part of the main protocol of the NORDISTEMI study19.
DESIGN AND STATISTICAL ANALYSIS
This substudy was a cohort study of exposed (TMP grade 0-1) versus unexposed (TMP grade 2-3) patients with the outcomes large infarct (defined as >75th percentile, 17.7%) and impaired left ventricular ejection fraction (<40%).
Analyses of effect modifiers and quantification of confounders were performed by stratification analysis. Confounding effects were quantified by comparing the crude odds ratio (OR) to the adjusted Mantel-Haenszel OR (ORmh). Effect modification was estimated by the Breslow-Day test of heterogeneity in the stratification procedure. Control for multiple confounders was performed by the multivariate logistic model and estimation of multiple interactions using the logistic likelihood ratio test26.
Receiver operating characteristic (ROC) curve analysis was performed for the ability of TMP to discriminate large infarct size and impaired LVEF. Estimated area under the curve (AUC) >0.75 indicates a good discriminatory effect of TMP grade on the outcomes large infarct size and low LVEF. A test of significance against an AUC=0.5 diagonal null hypothesis of non-discriminatory effect was performed.
Continuous variables were presented as medians with interquartile range. As several data were skewed, the Mann-Whitney U test was used for group comparison of continuous data. Categorical data were given as numbers and percentages, and analysis was performed using the chi-square test or Fisher’s exact test when appropriate.
Statistical analysis was performed using Epi Info™ version 3.3.2 (CDC, Atlanta, GA, USA). A p-value of <0.05 was considered statistically significant.
Results
Eighty-nine of the 266 patients included in the NORDISTEMI study were enrolled in this substudy, 71 from the early invasive group and 18 rescue patients from the conservative group. TIMI flow grade 3 was observed before PCI in 48 patients, and after PCI in 82 patients (92%). TMP grade after PCI was as follows: TMP grade 0 in 3 patients, TMP grade 1 in 31 patients, TMP grade 2 in 27 patients, and TMP grade 3 in 28 patients. The patients were divided into two groups depending on their TMP grade after PCI: Group I, TMP grade 0 and 1 (n=34), and Group II, TMP grade 2 and 3 (n=55). Baseline characteristics according to TMP group are shown in Table 1.
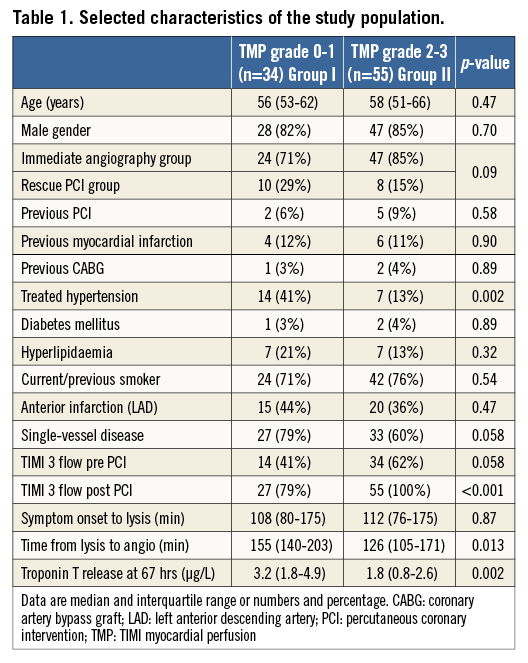
Patients with TMP grade 0-1 had a longer time from thrombolysis to angiography. There were no significant differences in infarct-related artery (LAD vs. LCX and RCA) between groups. More patients in Group II had TIMI 3 flow before PCI (60% vs. 40%). Significantly more patients in Group II had TIMI 3 flow after the procedure (Table 1). Patients in Group I had significantly higher values of troponin T at 67 hrs.
No significant differences were found between TMP groups in first-pass perfusion of the myocardium by MRI after three months. In both groups, maximum contrast enhancement and maximum contrast enhancement/time to peak were significantly reduced in the infarcted area compared to normal, remote myocardium (data not shown).
Patients with TMP grade 2-3 post PCI had significantly lower EDV, higher LVEF and better regional wall thickening in the infarcted region, and these patients also had significantly smaller infarct sizes (Table 2).
In a supplementary analysis, infarct size and LVEF were studied in relation to TIMI flow prior to PCI. When patients with TIMI flow 0, 1 and 2 (n=41) were compared with patients with TIMI 3 flow (n=48) prior to PCI, no significant differences were found in infarct size (11% [8-16] vs. 9% [4-19], p=0.47) or in LVEF (55% [47-60] vs. 57% [52-65], p=0.22) .
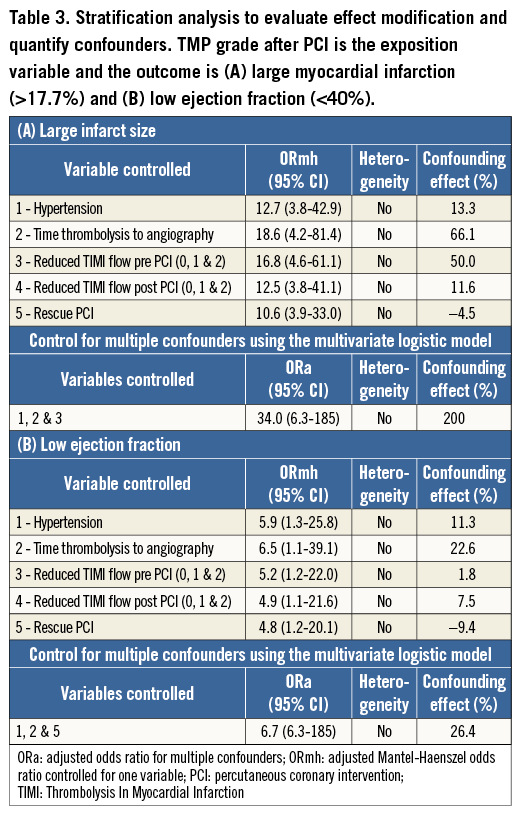
The prevalence of large infarct size and low LVEF in our population was 23/89 (25.8%) and 11/89 (12.4%), respectively. The patients with TMP grade 0-1 had an 11.2 times higher risk of developing large infarctions (95% confidence interval [CI]: 3.6-35.1, p<0.0001) and a 5.3 times higher risk of developing low LVEF (95% CI: 1.3-21.8, p=0.011).
Adjusting for potential confounders (hypertension, time from thrombolysis to angiography, TIMI flow at angiography, TIMI flow post PCI and belonging to the rescue PCI group) using a multivariate logistic model changed the results significantly. Adjusted OR (ORa) and 95% CI was 34.0 (6-185) for developing large infarctions, and 6.7 (6-185) for developing low LVEF, in patients with TMP 0-1 compared to TMP 2-3 (Table 3).
ROC curve analysis evaluating TMP grade 0-1 as a test for discriminating large relative infarct size (>17.7%) and impaired left ventricular function (LVEF <40%) is shown in Figure 1A and Figure 1B. For discriminating large infarct size, AUC was 0.77 (95% CI: 0.67-0.85, p=0.0001), and, for LVEF <40%, AUC was 0.69 (95% CI: 0.58-0.78, p=0.03).
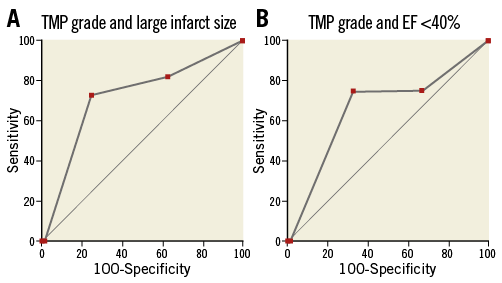
Figure 1. ROC curve analysis for large myocardial infarction and for impaired LVEF. ROC curve analysis for TMP grade after PCI as a diagnostic test of large myocardial infarction (>17.7%, 75th percentile) (A), and impaired LVEF (<40%) (B), evaluated by MRI at three months after STEMI.
A total of 15 out of 89 patients experienced a cardiovascular event (reinfarction, stroke or new ischaemia) within the first year after the index infarction: six out of 34 patients in the TMP grade 0-1 group (17.6%) and 9/55 in the TMP grade 2-3 group (16.4%). None of the patients died.
Discussion
The present study addresses the ability of the TMP grade at the end of a PCI procedure to predict large infarctions or reduced LVEF, in patients with STEMI treated with thrombolysis followed by early PCI. Both LVEF and infarct size were assessed by MRI three months after the infarction. The results suggested that TMP grade post PCI is an important predictor of both LVEF and infarct size in STEMI patients treated by a pharmaco-invasive strategy. Patients with TMP grade 0-1 had significantly higher OR for developing large infarctions (>17.7% of the left ventricle) and low LVEF (<40%) compared to patients with TMP grade 2-3. Our data are in agreement with previous studies performed in STEMI patients treated by thrombolysis11. Our study demonstrates that the time delay from thrombolysis to angiography was an important confounder for the predictive effect of TMP grade, both on infarct size and LVEF. These findings are in agreement with previous results showing that TIMI flow 2 or less and myocardial blush grade (MBG) 0 and 1 were associated with time delay pre PCI, and also associated with increased end-diastolic and end-systolic volumes at follow-up15,27.
In 2008, Pride et al28 showed reduced morbidity and mortality in STEMI patients with high angiographic perfusion score, which combines TIMI flow grade and TMP grade, treated with late PCI following fibrinolytic therapy. Our finding is contrary to the study of Wong et al15 which did not show a correlation between TMP grade and LVEF after three months. This might be due to their smaller study population and a slightly different definition of impaired myocardial perfusion at PCI. Furthermore, they included solely patients who underwent primary PCI15.
In a recent study on TMP grade after late recanalisation (>24 hours) of infarct-related arteries, moderate improvements in LVEF in patients with both perfusion grade 0-1 and grade 2-3 were found, but there was no significant difference between the groups29. In the present study on patients treated with early PCI after thrombolysis, the patients with TMP grade 2-3 had significantly better regional wall function, global LVEF and smaller infarct volumes after three months. The reason for this discrepancy is not clear, but we might speculate that, with late infarct artery recanalisation, the predictive ability of the TMP grade post PCI on LVEF is reduced or lost. Our finding that time delay from thrombolysis to PCI was an important confounder for the predictive effect of TMP grade supports this explanation. Furthermore, both during primary PCI and early post PCI for STEMI there is an evolution of MBG and TMP grade, and it is the final perfusion outcome that is best correlated to remodelling, LV function and even to mortality27,30.
TMP grade 0-1 was associated with larger left ventricular end-diastolic and end-systolic volumes, and reduced diastolic wall thickness and reduced systolic wall thickening in the infarcted region. These data indicate favourable left ventricular remodelling in patients with restored myocardial perfusion (TMP grade 2-3).
Normalised epicardial blood flow after STEMI as assessed by TIMI flow grades has been related to improved outcome, both after thrombolytic treatment and after primary PCI9,31. However, myocardial tissue perfusion may be impaired despite restoration of normal epicardial blood flow. Recent studies indicate that myocardial perfusion, measured as myocardial TMP grade, may allow further risk stratification. Patients with myocardial TMP grades 0 and 1 have been shown to have larger enzymatic infarct sizes, lower LVEF and higher mortality6,9,12,13,30,32-35. Brener et al gave evidence for TMP grade 2 and 3 predicting survival both at 30 days and at three years in a trial with 3,602 patients14. In our study, we observed all patients over a period of one year but did not find any difference in clinical outcome between the groups. More patients and a longer follow-up period might have been necessary for this analysis to be conclusive.
Although first-pass perfusion at MRI, measured as maximum contrast enhancement, was significantly reduced in infarcted myocardium compared to remote reference myocardium in both groups, we found no significant differences in first-pass perfusion between patients with TMP grade 0-1 and those with TMP grade 2-3. This is in agreement with our previous results in STEMI patients treated with primary PCI, in which there was a significant reduction in maximum contrast enhancement in the TMP grade 0-1 group on early MRI within five days after the STEMI, but no significant differences after three months6. Considering the findings in both of these studies, one could speculate that MRI perfusion might be most useful in the acute phase of myocardial infarction.
Infarct-related artery patency at baseline angiography before primary PCI for STEMI is associated with improved one-year clinical outcomes, including lower death rates36. In the present study, when the patients were dichotomised depending on TIMI flow at angiography prior to PCI, no significant differences were found between groups in left ventricular function or infarct size at MRI after three months. However, reduced TIMI flow pre PCI was found to have a significant confounding effect on the predictive effect of TMP grade on infarct size.
We suggest that TMP grading post thrombolysis and PCI may be used as a complementary predictor of large final infarct size and severely reduced LVEF, and may be an alternative when early cardiac magnetic imaging is not available.
Limitations
The generalisation of our data is limited by the small sample size of only 89 patients. The limited number of patients did not allow us to divide TMP grade 2-3 into separate groups with intermediate and normal microcirculation, respectively. Another limitation is that TMP is an angiographic tool which requires specific training before one can draw conclusions on myocardial perfusion.
It should be noted that to define infarct size >17.7% as large was correct for our study population. However, in similar studies of STEMI patients, the 75th percentile for infarct size ranged from 15.7% to 30%. Accordingly, extrapolation of our results to other STEMI populations should be done with caution.
The presence of MVO demonstrated by MRI early after infarction is associated with impaired myocardial salvage23. In the present study MVO was not assessed as there were no early MRI data collected.
Conclusions
When assessed by contrast-enhanced MRI three months after STEMI treated by thrombolysis and early PCI, patients with TMP grade 2-3 post PCI had higher LVEF and smaller infarct sizes compared to patients with TMP grade 0-1. The risk of developing large infarctions and low LVEF was significantly increased in patients with TMP grade 0-1, even after adjustment for confounders. TMP grading post thrombolysis and PCI may be used as a predictor of large final infarct size and severely reduced LVEF, and may be an alternative when early cardiac magnetic imaging is not available. TMP grading should be considered as a relevant supplement to TIMI flow when the success of a PCI procedure is evaluated.
| Impact on daily practice When assessed by contrast-enhanced MRI three months after STEMI treated by thrombolysis and early PCI, patients with TMP grade 0-1 post PCI had significantly lower LVEF and larger infarct sizes compared to patients with TMP grade 2-3, even after adjustment for confounders. TMP grading post thrombolysis and PCI may be used as a predictor of large final infarct size and severely reduced LVEF, and may be an alternative when early cardiac magnetic imaging is not available. TMP grading should be considered as a relevant supplement to TIMI flow when the success of a PCI procedure is evaluated. |
Acknowledgements
The study was funded by grants from the Scientific Board of the South Eastern Norway Regional Health Authority. The authors are grateful for the excellent MRI scanning assistance of Vigdis Rosseland and Marianne Nesheim and the secretarial work of Grethe Hansen.
Conflict of interest statement
The authors have no conflicts of interest to declare.