Device description
Name and manufacturer: The STENTYS Self-Apposing® stent; Stentys S.A., Paris, France.
Approval status: CE mark in 2010 (for acute coronary syndrome treatment). Sirolimus-eluting version received CE mark in 2014.
Platform: Nitinol.
Strut thickness: 102 microns (0.0040”; small-sized STENTYS) or 133 microns (0.0052”; medium- and large-sized STENTYS).
Coating: Available in three versions: (i) not coated (bare metal stent); (ii) paclitaxel-coated; (iii) sirolimus-coated.
Specific stent design: The STENTYS Self-Apposing stent has a typical “Z-shaped” architecture, which includes disconnectable stent struts called “interconnectors”. These latter allow stent disconnection at the level of the coronary bifurcation (Figure 1, Moving image 1, Moving image 2).
Guiding: 6 Fr.
Classification according to MADS: “A” (main branch [MB] stenting across side branch [SB], allowing one-stent [MB stenting + SB balloon; MB stenting + kissing] or two-stent [elective T-stenting; internal crush; culotte; TAP] strategy).
Delivery system: A 6 Fr compatible, rapid exchange delivery system delivers the stent into position over a conventional 0.014” guidewire. The stent is deployed by the withdrawal of a retractable sheath using the delivery system trigger (Online Figure 1).
Stent sizes: There are three different sizes commercially available: (i) small (2.5-3.0 mm); (ii) medium (3.0-3.5 mm); and (iii) large (3.5-4.5 mm).
Stent length: The stent is available in three different lengths: 17, 22 and 27 mm.
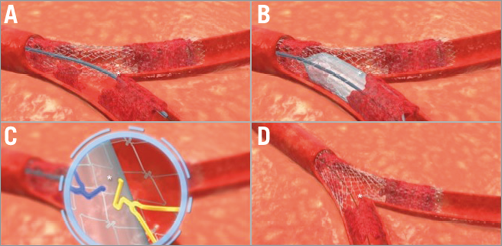
Figure 1. Sequence of STENTYS strut disconnection in a bifurcation lesion. A) Rewiring of the SB. B) Gentle balloon inflation into the SB. C) Disconnection of the STENTYS interconnectors. D) Wide opening of the STENTYS stent towards the SB. SB: side branch
Procedural details
The procedure is performed by wiring both MB and SB with standard 0.014” guidewires. MB predilation is recommended. The STENTYS stent is positioned in the main branch across the bifurcation, by advancing the system distal to the desired position by at least 5 mm (Online Figure 1A). Under fluoroscopy guidance, the dedicated trigger is retracted, allowing the withdrawal of the covering sheath (Online Figure 1B). Post-dilatation of the STENTYS stent with an adequately sized balloon is highly recommended. Proximal optimisation or kissing-balloon techniques are not mandatory due to the self-apposing nature of the device. If access or treatment of the side branch is required, a balloon is advanced into the SB after wire re-crossing, and inflated at low pressure, to perform the strut disconnection by a stretch (flexion) and a twist (rotation) motion imparted by the balloon onto the interconnector (Moving image 1). Side branch treatment, e.g., placement of an additional balloon-expandable stent, follows the usual indications and proceedings.
Clinical data
The first-in-man experience with the STENTYS Self-Apposing stent showed encouraging results in terms of procedural results and short- and medium-term efficacy and safety1,2. The STENTYS® Coronary Bifurcation Stent System fOr the PErcutaNeous treatment of de novo lesions in native bifurcated coronary arteries (OPEN I) study showed a six-month major adverse cardiovascular event (MACE) rate of 3.7% for the drug-eluting stent (DES) version of the stent, driven by target lesion revascularisation (TLR). MACE and TLR rates were significantly higher for the BMS version of the stent. Procedural success was 95.2%, while post-stenting disconnection was performed on 90% of the stents implanted. Angiographic follow-up performed in 95% of patients demonstrated late luminal loss of 0.42±0.45 mm and 0.16±0.45 mm in the target main vessel and side branch, respectively. Intravascular ultrasound (IVUS) assessment at six months showed an increase in the mean luminal area (mm2) observed at baseline and at follow-up (DES: 7.39±1.99 vs. 8.58±2.48; p>0.05, and BMS: 7.94±1.39 vs. 8.91±2.54; p>0.05)2. The recently presented OPEN II observational study enrolled 207 patients and showed a 12-month MACE rate of 13%, mainly driven by TLR. The rate of strut disconnection was 56.0%, while FKBI was performed in only 21.7%. FKBI was not associated with statistically significant differences in MACE observed at six and 12-month follow-up3.
The STENTYS Self-Apposing stent has also been successfully used in the setting of acute ST-elevation myocardial infarction (STEMI). The APPOSITION I study confirmed safety and feasibility of the STENTYS stent in STEMI patients with no cases of late stent malapposition at six-month follow-up4. The randomised APPOSITION II trial showed a lower rate of malapposed stent struts in the STENTYS group compared to the balloon-expandable group at three days after implantation (0.58% vs. 5.46%, p<0.001)5. The observational APPOSITION III registry data showed a 9.3% MACE rate in patients treated with STENTYS during primary percutaneous coronary intervention (PCI) for STEMI6. The randomised APPOSITION IV showed better four-month stent apposition using the sirolimus-eluting version of the STENTYS, as compared to zotarolimus-eluting balloon-expandable stents7.
Ongoing studies
The APPOSITION V trial randomising STEMI patients to treatment with the bare metal version of STENTYS vs. the MULTI-LINK VISION™ stent system (Abbott Vascular, Santa Clara, CA, USA) was prematurely stopped due to slow enrolment8,9. A novel balloon delivery system (BDS) was recently developed for the sirolimus-eluting version of the STENTYS. It consists of inflating a balloon at low pressures to split the covering delivery sheath longitudinally, which releases the self-apposing STENTYS SES. The stent deploys and apposes to the vessel wall whereafter the “jailed” sheath is retracted. This system aims for easy delivery and a highly precise longitudinal placement of the STENTYS SES.
Unique features
The self-apposing nature of the device allows covering different anatomies of bifurcations without manual adaptation of the position, which is sometimes a limitation using other dedicated devices.
Self-apposition is also thought to be of benefit in cases where sizing of a stent is difficult (e.g., aneurysmatic coronary arteries or STEMI patients with heavy thrombotic load).
The “Z-shape” architecture with disruption of the interconnectors allows a facilitated SB access.
Potential improvements
The crossing profile (1.397 mm) is relatively high and can cause failure of the procedure. In general, the current device requires careful predilatation of the lesion to avoid difficulties during positioning. Likewise, the sheath retraction system used for positioning can result in geographical mismatch between the lesion and the positioned STENTYS. The next-generation balloon-expandable device is currently under development.
Acknowledgements
The authors are thankful to Mr David Bouchez and Mr Tom Coles for their help with the iconographic material and the Moving images.
Conflict of interest statement
C. Naber is principal investigator of the OPEN II trial. The other authors have no conflicts of interest to declare.
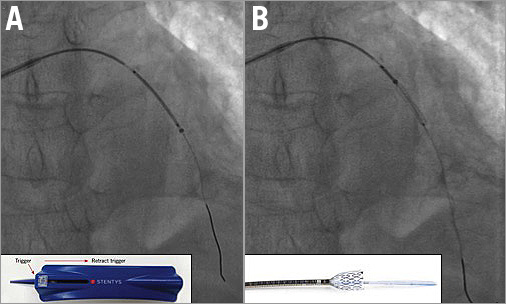
Online Figure 1. STENTYS Self-Apposing stent implantation under fluoroscopic guidance. A) The STENTYS stent is positioned in the main branch across the bifurcation, by advancing the system distal to the desired position by at least 5 mm. B) The dedicated trigger is retracted, allowing the withdrawal of the covering sheath.
Online data supplement
Moving image 1. Graphic representation of the STENTYS Self-Apposing stent implantation.
Moving image 2. Micro-computed tomography of a STENTYS Self-Apposing stent with opening to the side branch.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Graphic representation of the STENTYS Self-Apposing stent implantation.
Moving image 2. Micro-computed tomography of a STENTYS Self-Apposing stent with opening to the side branch.

