Abstract
Background: Thrombectomy is an effective treatment for acute ischaemic stroke (AIS).
Aims: The aim of this study was to compare clinical outcomes with intracranial artery occlusion site among AIS patients treated in the setting of a cardiology cath lab.
Methods: This was a single-centre, prospective registry of 214 consecutive patients with AIS enrolled between 2012 and 2018. All thrombectomy procedures were performed in a cardiology cath lab with stent retrievers or aspiration systems. The functional outcome was assessed by the modified Rankin Scale (mRS) after three months.
Results: Ninety-three patients (44%) had middle cerebral artery (MCA) occlusion, 28 patients (13%) had proximal internal carotid artery (ICA) occlusion, 27 patients (13%) had tandem (ICA+MCA) occlusion, 39 patients (18%) had terminal ICA (T-type) occlusion, and 26 patients (12%) had vertebrobasilar (VB) stroke. Favourable clinical outcome (mRS ≤2) was reached in 58% of MCA occlusions and in 56% of isolated ICA occlusions, but in only 31% of T-type occlusions and in 27% of VB stroke. Poor clinical outcome in T-type occlusions and VB strokes was influenced by the lower recanalisation success (mTICI 2b-3 flow) rates: 56% (T-type) and 50% (VB) compared to 82% in MCA occlusions, 89% in isolated ICA occlusions and 96% in tandem occlusions.
Conclusions: Catheter-based thrombectomy achieved significantly better clinical results in patients with isolated MCA occlusion, isolated ICA occlusions or tight stenosis and tandem occlusions compared to patients with T-type occlusion and posterior strokes.
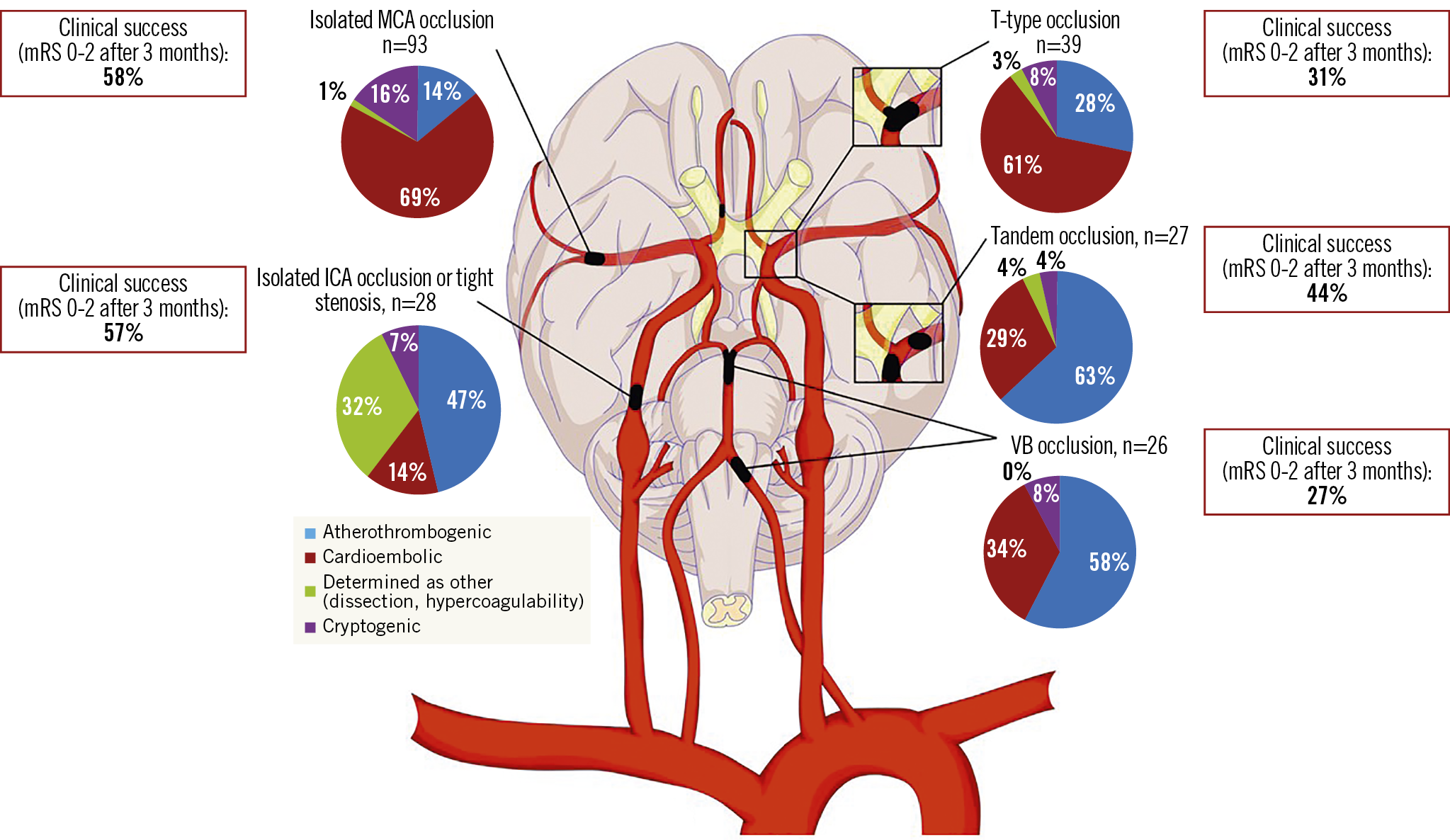
Visual summary. Endovascular intervention of isolated MCA or ICA occlusions provides greatest clinical benefit, while interventions in posterior circulation have lower chance for clinical success.
Introduction
According to estimates by the World Health Organization, stroke is the second leading cause of preventable death worldwide and the leading cause of serious, long-term disability1. It is also the second most common cause of dementia, the most frequent cause of epilepsy in the elderly, and a frequent cause of depression2,3. The majority of strokes (87%) are classified as ischaemic, the rest (13%) as haemorrhagic4.
Death or severe disability occurs in patients with emergent large vessel occlusion. Approximately one third of all ischaemic strokes are caused by middle cerebral artery (MCA) occlusion. Vertebrobasilar (VB) strokes represent about 5-6% of all ischaemic strokes, but prognosis may be fatal5. A prompt and complete restoration of blood flow in the affected artery is the key factor for a favourable neurological outcome – “time is brain”. Until recently, intravenous tissue plasminogen activator (t-PA) was the only proven treatment for large vessel occlusion. However, the landscape of ischaemic stroke treatment has changed with the publication of five randomised multicentre controlled clinical trials in 2015. According to these trials, catheter-based mechanical thrombectomy (CBT) was proven to be an effective treatment for proximal occlusions of the major intracranial arteries in acute stroke patients, and became a class IA indication6,7,8,9,10. Approximately 30% of ischaemic strokes are caused by large vessel occlusion and should be considered for intervention11.
The aim of this study was to compare clinical outcomes of patients treated by CBT for acute ischaemic stroke based on intracranial artery occlusion site and stroke aetiology.
Methods
STUDY PATIENTS
This was a single-centre, prospective, observational registry of consecutive patients (pts) treated by CBT for an acute ischaemic stroke. A total of 214 consecutive pts (mean age 67.4±12.2, range 21-92 years, male 53.7%) were enrolled between October 2012 and June 2018. The study was based on the pre-specified protocol approved by the ethics committee and was designed in collaboration among cardiologists, neurologists and radiologists12. All participants (or their legal representatives) provided written informed consent. On admission, all patients were examined by a neurologist, including basic laboratory screening. Afterwards, a computed tomography (CT) scan with angiography was performed to confirm large vessel occlusion and to rule out intracranial haemorrhage. On the basis of a comprehensive examination and compliance with inclusion criteria, an endovascular intervention was indicated. Intravenous thrombolytic pretreatment was administered by a neurologist based on CT scan and coagulation results.
Inclusion criteria were: moderate to severe acute ischaemic stroke (National Institutes of Health Stroke Scale [NIHSS] score ≥6), time interval <6 hours from symptom onset (except for basilar artery occlusion, where the therapeutic window was not strictly limited and the treatment strategy was assessed individually) or CT scan <2 hours from time of “wake-up stroke” diagnosis, no or only small ischaemia visible on the admission CT scan, CT evidence for an occluded major artery (either CT angio or dense artery sign on CT scan), expected ability to start intervention within <60 minutes from CT and age ≥18 years. Exclusion criteria were previously known neurologic symptoms (modified Rankin Scale [mRS] score 2-5), known severe hypoglycaemia, unmeasurable international normalised ratio (INR), intracranial bleeding and CT evidence of large ischaemia.
INTERVENTIONS
All interventions were performed in the cardiology cath lab either by a board-certified interventional radiologist or by a cardiologist with a licence for interventional angiology (Czech Medical Chamber – licence no. F021), mostly under local anaesthesia. The decision concerning the revascularisation strategy was made by the interventionist. In patients with proximal internal carotid artery (ICA) occlusion or tight stenosis, the default strategy was carotid stenting in the acute phase; we did not perform deferred stenting in this study. The dose of heparin administered was at the operator’s discretion and depended on the patient's physical constitution, type of procedure and preprocedual INR value. In patients with an effective INR value or in those who had been demonstrably taking any of the new oral anticoagulants, the heparin dose was either reduced or not administered at all.
FOLLOW-UP
The success of recanalisation was assessed immediately post procedure by follow-up angiography. Patients were subsequently monitored in the intensive care unit in either the Department of Cardiology or the Department of Neurology. Most cases in our study group had a control CT scan on day 1 to evaluate infarction size and possible haemorrhage. Details have been described previously12. During the remaining hospitalisation, at least 24-hour electrocardiography monitoring, sonography of the carotid arteries and transthoracic/transoesophageal echocardiography were performed in all patients to exclude other possible sources of embolisation. In indicated cases, prolonged ECG monitoring (48 hours, 7 days, 30 days) was carried out during three-month follow-up. The aetiology of strokes was determined based on the TOAST classification13.
ANTITHROMBOTIC REGIMEN
After the acute phase the antithrombotic regimen was individualised based on stroke aetiology and stroke severity. In atherothrombotic strokes (e.g., ICA lesions), antiplatelet treatment was initiated, while in cardioembolic or cryptogenic strokes anticoagulation treatment was initiated if no contraindication was present. The onset of these antithrombotic treatments varied between day 2 and day 14 after stroke onset, based on the extent of final ischaemia and presence/absence of haemorrhagic transformation.
STUDY ENDPOINTS
The primary endpoint was a functional neurologic outcome in three months assessed by board-certified neurologists. The secondary endpoints were angiographic recanalisation success rate, change of the NIHSS (ΔNIHSS) score from admission to discharge and symptomatic intracranial bleeding. The degree of dependence after a stroke was measured using the mRS after three months of follow-up. Two patients (foreign tourists) were lost during three-month follow-up. The study registry included patients’ demographic and epidemiological data – age, sex, body mass index (BMI), prior stroke/transient ischaemic attack (TIA), known coronary and peripheral arterial disease, arterial hypertension, hyperlipidaemia, diabetes mellitus, chronic kidney injury, current smoking (defined as ≥1 month prior to admission), atrial fibrillation (AF; known or de novo identified either during the hospitalisation or during three-month follow-up) and chronic antithrombotic therapy; periprocedural data – time intervals (symptoms onset – door time – CT scan – needle time [if] – groin puncture time – recanalisation time [if]), change of NIHSS score from admission to discharge and angiographic findings (type of occluded artery, preprocedural and post-procedural modified Thrombolysis In Cerebral Infarction [mTICI] flow).
STATISTICAL ANALYSIS
Age, BMI and scores as continuous variables were described by a mean including standard deviation. All other variables were dichotomous, expressed as number and proportion. The normal distribution of continuous variables enabled their comparison among occlusion sites using one-way ANOVA with Tukey's multiple comparisons test. The difference in NIHSS score at admission and discharge was assessed by paired t-test. Furthermore, dichotomous variables among occlusion sites were statistically evaluated using the χ² test. All tests were two-tailed, and the level of significance was set at 0.05. Statistical analyses were performed using Prism 8 (GraphPad Software, Inc., La Jolla, CA, USA) and Stata version 16 software (StataCorp, College Station, TX, USA).
Results
BASELINE CHARACTERISTICS
A total of 214 patients were enrolled in the study. Mean age of this cohort was 67.4±12.2 years, with VB stroke (71.9±8.8) patients being significantly older than others. The prevalence of active smoking, hypertension, diabetes mellitus, dyslipidaemia, renal insufficiency, prior stroke/TIA and known coronary and peripheral artery disease did not differ significantly among the occlusion sites. Intravenous thrombolytic pretreatment was administered in 88 pts (41.1%). General anaesthesia was used in a total of 32 pts, significantly more often in T-type and VB strokes (p=0.031). Details are presented in Table 1.
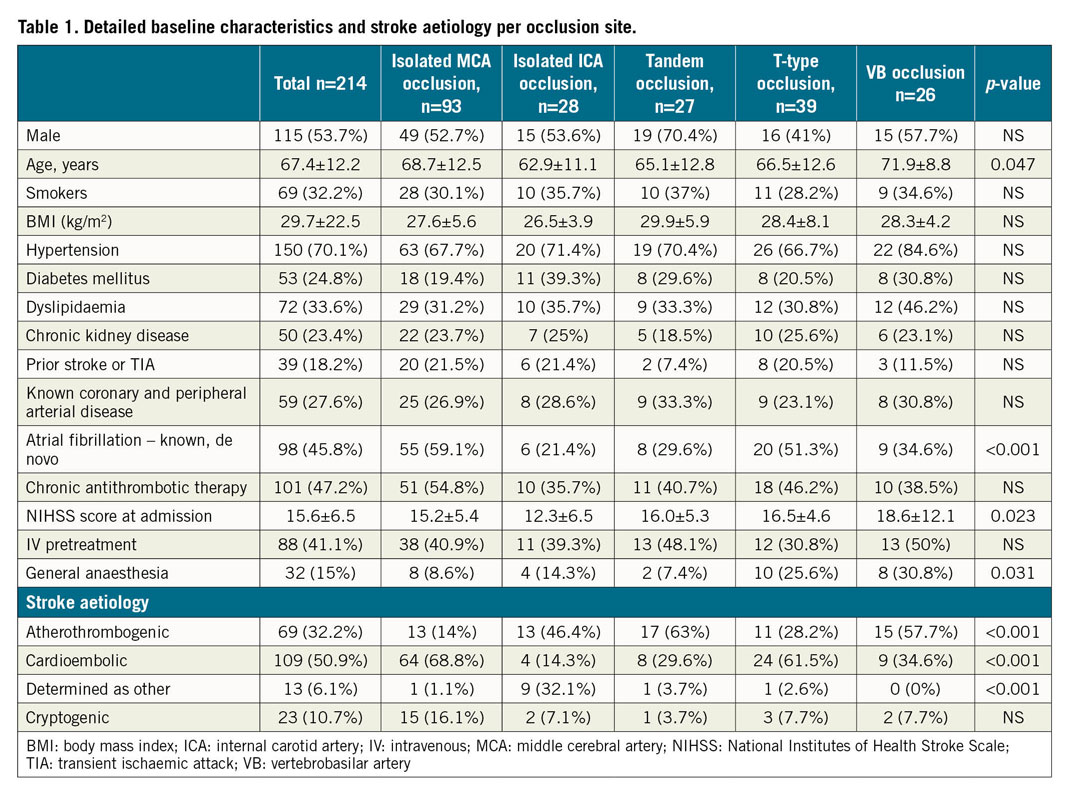
OCCLUDED ARTERIES
The distribution of intracranial artery occlusion sites was non-uniform. Ninety-three pts (43.5%) had MCA occlusion, 28 pts (13.1%) had isolated ICA occlusion/tight stenosis, 27 pts (12.6%) had tandem occlusion (ICA+MCA), 39 pts (18.2%) had terminal internal carotid artery (T-type) occlusion, 26 pts (12.1%) had VB stroke, and one patient had an isolated anterior cerebral artery (ACA) occlusion.
STROKE AETIOLOGY
The AIS aetiology was assumed to be cardioembolic in 50.9%, atherothrombogenic in 32.2%, cryptogenic in 10.7% and determined as other in 6.1% of pts. Isolated MCA occlusion and T-type strokes were significantly more frequently caused by cardioembolism (68.8% and 61.5%), which was also reflected by more frequent occurrence of AF in these patients (59.1% and 51.3%). VB strokes, tandem occlusion and isolated ICA occlusion/tight stenosis strokes were mostly atherothrombogenic (57.7%, 63.0% and 46.4%). Details are presented in Figure 1.

Figure 1. Stroke aetiology by occlusion site. Isolated MCA occlusion is most frequently caused by cardioembolism, while proximal ICA and VB lesions are most frequently caused by atherothrombosis. ICA: internal carotid artery; MCA: middle cerebral artery; VB: vertebrobasilar artery
ANGIOGRAPHIC OUTCOMES
The overall recanalisation success rate (mTICI 2b-3 flow) was 76.2%. The proportion of successful recanalisation was significantly higher in MCA (81.7%), ICA (89.3%) and tandem (96.3%) occlusions compared to T-type (56.4%) and VB (50%) occlusions (p<0.001). A total of 13 patients (6.1%) suffered from symptomatic intracranial bleeding (defined as ΔNIHSS ≥4 within 48 hours after intervention) with uniform distribution among all occlusion sites. Detailed primary and secondary endpoints are shown in Table 2. Examples of thrombectomy procedures per anatomic stroke type are shown in Figure 2-Figure 4. The only patient with isolated ACA occlusion was a 50-year-old man, smoker. His NIHSS score decreased from 12 (at admission) to 0 (at discharge). The recanalisation was successful with final mTICI 3 and the patient reached full neurological recovery (mRS 0) in three-month follow-up. The stroke aetiology was assumed to be due to known hypercoagulability.
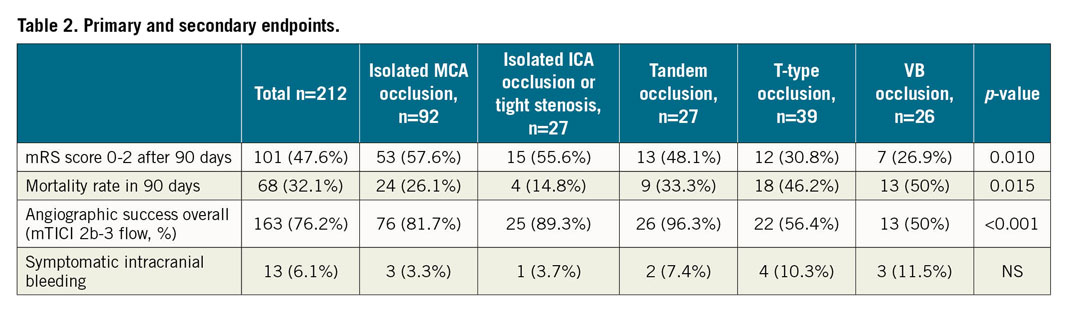

Figure 2. Typical angiographic findings in proximal ICA occlusion and in MCA occlusion. From left to right: (1) proximal ICA severe stenosis with intraluminal thrombus, (2) after stent implantation, (3) MCA occlusion, (4) after thrombectomy.
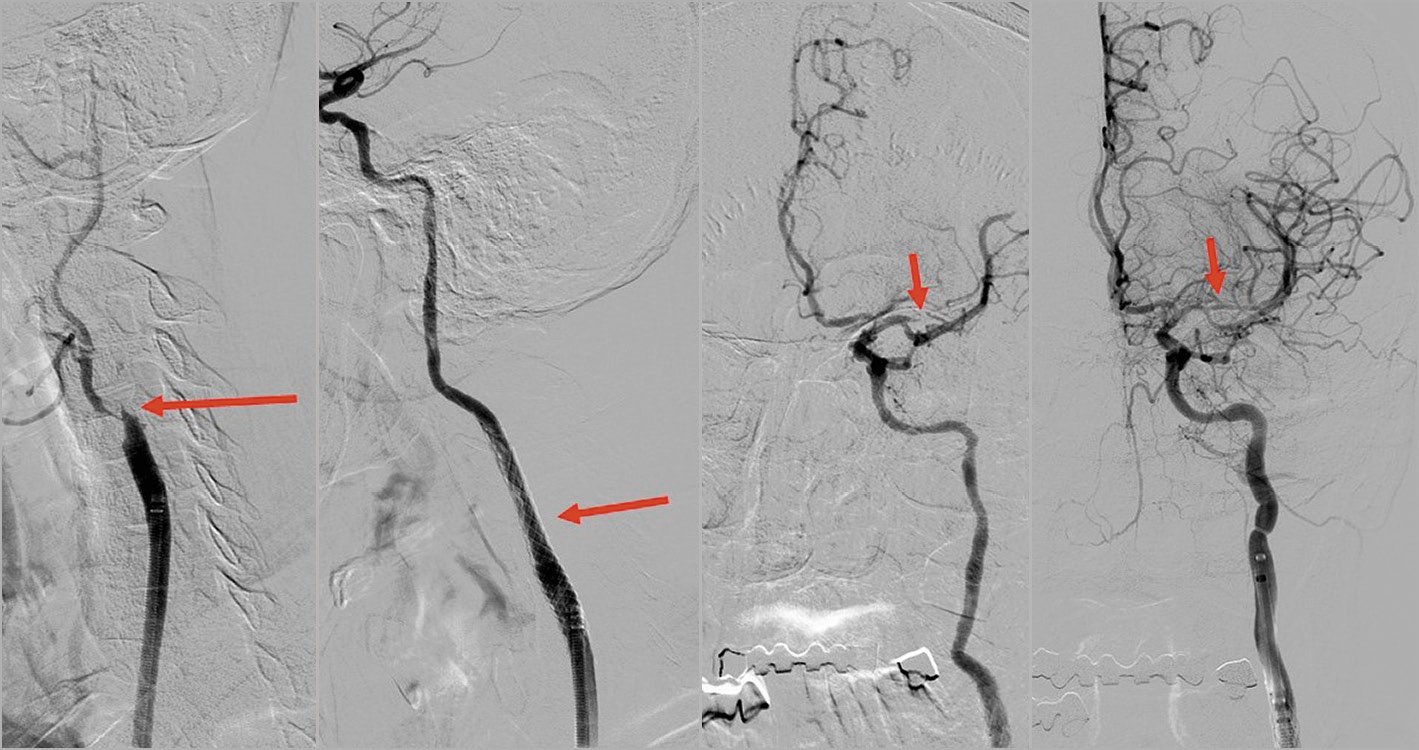
Figure 3. Typical angiographic findings in the tandem occlusion (proximal ICA and MCA occlusion). From left to right: (1) proximal ICA occlusion, (2) after stent implantation, (3) MCA occlusion, (4) after thrombectomy.

Figure 4. Typical angiographic findings in ICA T-occlusion and in BA occlusion. From left to right: (1) terminal ICA occlusion (T-type), (2) after thrombectomy, (3) BA occlusion, (4) after thrombectomy. BA: basilar artery
CLINICAL OUTCOMES
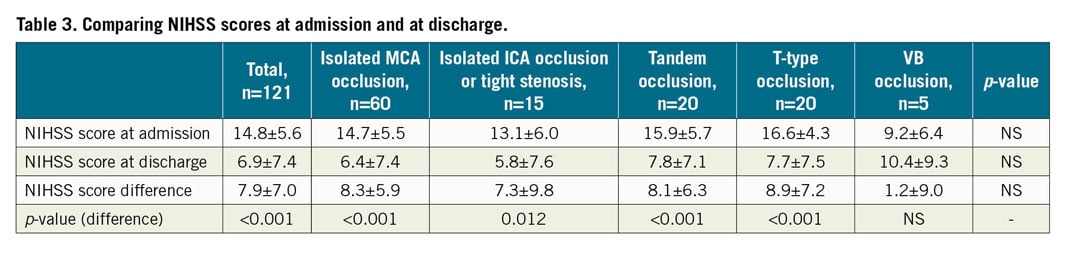
The primary study endpoint was three-month clinical outcome with a favourable clinical outcome defined as mRS ≤2, which was reached in 47.6% (101 of 212 pts). Patients’ clinical outcomes varied significantly among occlusion sites. A favourable clinical outcome was achieved significantly more often in MCA occlusions (56.7%) and isolated ICA occlusions or tight stenosis (55.6%) compared to others (p=0.010). In addition, patients without diabetes had twice as much chance of achieving a favourable clinical outcome as patients with diabetes, and not using general anaesthesia increased the chance of a favourable clinical outcome almost three times. The overall mortality rate was 32.1% with significantly higher rates in T-type and VB occlusions (46.2% and 50%, p=0.015). The distribution of mRS score based on occluded artery site is presented in Figure 5. The distribution of NIHSS scores at admission was not uniform among occlusion sites. Patients with VB strokes had the highest NIHSS scores (18.6±12.1); on the other hand, patients with isolated ICA occlusion or tight stenosis had the lowest scores (12.3±6.5). Comparing NIHSS scores at admission and discharge based on occlusion site (unfortunately determined in only 121 patients), NIHSS scores decreased significantly in almost all stroke types except VB stroke. Details are shown in Table 3.
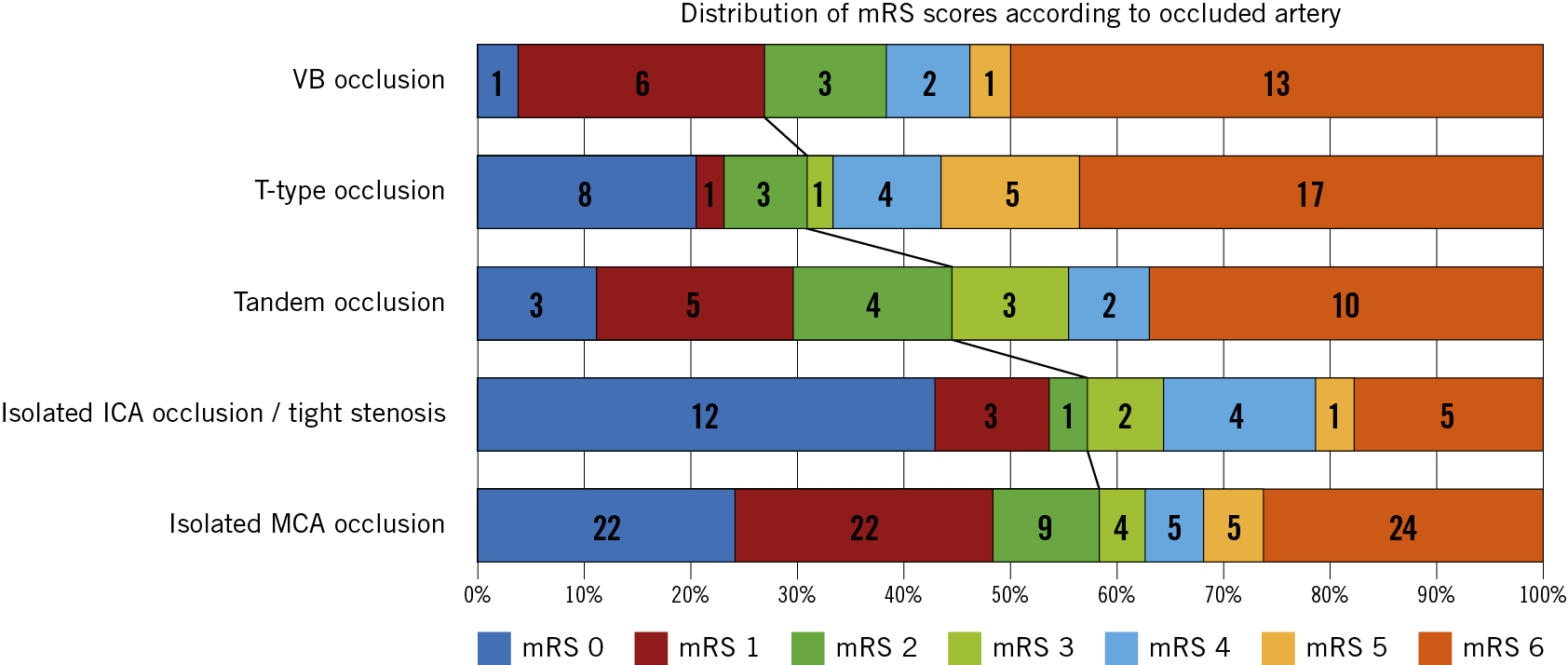
Figure 5. Distribution of mRS scores based on occluded artery site. From the lowest clinical success rates (VB occlusion) to the highest rates (isolated MCA occlusion). ICA: internal carotid artery; MCA: middle cerebral artery; mRS: modified Rankin Scale; VB: vertebrobasilar artery
Discussion
COMPARISON WITH TREVO 2000 REGISTRY14 IN NON-SELECTED ALL-COMERS
In our study group of patients treated for anterior and posterior strokes with mechanical thrombectomy for large vessel occlusions, a favourable clinical outcome (mRS score ≤2 at three months) was reached in 47.6% (101 of 212 pts). Despite the fact that the angiographic success rate was higher in the Trevo 2000 study (92.8%) versus our study (76.2%), the resulting favourable clinical outcomes (mRS score ≤2) were comparable (55.3% in Trevo versus 47.6% in PRAGUE-16). This may be explained by the different distribution of occlusion sites. Patients’ baseline characteristics (age, diabetes mellitus, AF, NIHSS score at admission) did not differ in the other compared data. Details are shown in Table 4.
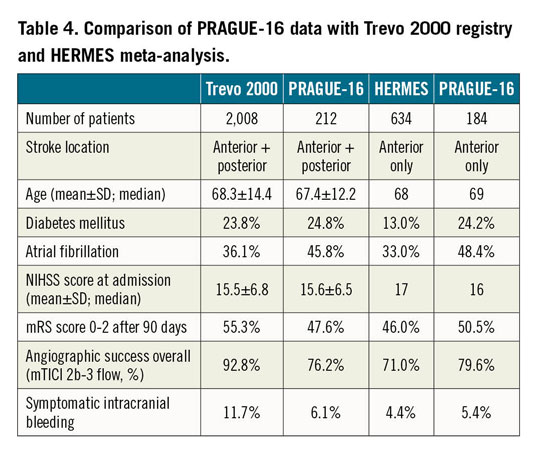
COMPARISON WITH FIVE RANDOMISED TRIALS15 IN ANTERIOR STROKE
A previous meta-analysis of five randomised trials (MR CLEAN, ESCAPE, REVASCAT, SWIFT PRIME, and EXTEND IA) found favourable clinical outcomes (mRS score 0-2 after 90 days) in 46% of pts and an angiographic success rate of 71% in cases treated by thrombectomy for anterior stroke. In our study subgroup with anterior stroke only (184 patients), neurological recovery was achieved in 50.5% of cases and successful recanalisation in 79.6%, which is consistent with expert neurointerventional centre data. Furthermore, the risk of symptomatic intracerebral haemorrhage in our study (5.4%) was comparable with that reported in the meta-analysis (4.4%). Baseline characteristics of patients differed only by the presence of AF, which was more common in our study. Details are shown in Table 4.
OUTCOMES BASED ON OCCLUSION SITE
The best clinical outcomes (mRS score ≤2 at three months, mortality rate) were reached in patients with MCA and isolated ICA occlusions/tight stenosis. In these patients, the recanalisation success rate was high (81.7%, 89.3%) and blood flow was restored in less than four hours from symptom onset. The incidence of symptomatic intracranial bleeding was the lowest in these two groups as well. Better clinical outcome in these patients might also be influenced by lower initial NIHSS scores as a powerful predictor for long-term outcome16,17. T-type occlusion and VB strokes were associated with the poorest outcomes. Untreated VB strokes are associated with almost 100% mortality. Therefore, endovascular treatment is strongly recommended, although, according to a meta-analysis of 45 clinical trials, three patients with this life-threatening diagnosis have to be treated to prevent one death or dependency5,18. In our study, patients with T-type occlusion or VB strokes had a higher initial NIHSS score, lower recanalisation success rate and higher incidence of intracranial haemorrhage. VB stroke patients were the oldest subgroup. The North American Solitaire Stent Retriever Acute Stroke (NASA) registry found that age, occlusion site, high NIHSS score, diabetes, no t-PA, ≥3 passes, and use of rescue therapy were associated with poor 90-day outcome despite successful recanalisation19.
OUTCOMES BASED ON STROKE AETIOLOGY
AF is associated with a 4-5 times increased risk of ischaemic stroke20. It is known that patients who suffered from cardioembolic ischaemic stroke tend to have worse outcomes after any (not only endovascular) treatment compared to patients with other aetiologies of stroke21. Generally, patients with AF are older, have a worse functional pre-stroke condition and appear to have different occlusion locations and larger infarct volumes22. In half of all ischaemic strokes (50.9%), stroke aetiology was assumed to be cardioembolic, mostly due to known or de novo identified AF (81.7%). Isolated MCA occlusion and T-type strokes were caused mostly by cardioembolism (68.8% and 61.5%, respectively); VB strokes, isolated ICA occlusion/tight stenosis and tandem occlusion strokes were mostly atherothrombogenic (57.7%, 46.4% and 63%, respectively).
OUTCOMES OF STROKE THROMBECTOMY PERFORMED IN CARDIOLOGY CATH LABS
The main limitation of the widespread use of mechanical thrombectomy for the treatment of acute ischaemic stroke is the lack of experienced interventionalists in many countries and regions. Thus, in some regions, cardiologists in close cooperation with neurologists, offer stroke thrombectomy services. The first published data provided outcomes comparable to those of stroke thrombectomy performed by neuroradiologists10,23,24,25. Our study presents the largest series of consecutive patients with acute ischaemic stroke treated in the cardiology cath lab.
Study limitations
The main study limitation is the single-centre design. However, the consecutive enrolment of all thrombectomy patients treated in this institution during the study period and the complete three-month follow-up formed a good base for this analysis, which does not compare two treatments, but rather several anatomic and aetiologic variants of the same disease treated by the same method.
Conclusions
Catheter-based thrombectomy achieved significantly better clinical results in patients with isolated MCA occlusion, isolated ICA occlusions and tandem occlusions compared to patients with T-type occlusion and posterior strokes.
|
mpact on daily practice Stroke aetiology and location of the thrombotic occlusion play a very important role in the angiographic and clinical outcomes of acute ischaemic stroke patients treated by thrombectomy. Patients with posterior circulation strokes and anterior strokes caused by carotid artery terminus occlusion have worse outcomes, and techniques for these stroke subtypes should be further refined. |
Funding
Supported by the Charles University Research Project Progress Q35.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.