Abstract
Aims: Endovascular thrombectomy (EVT) improves outcome after acute ischaemic stroke (AIS) caused by an intracranial occlusion. The aim of the present study was to determine whether atrial fibrillation (AF) modifies the effect of EVT.
Methods and results: MR CLEAN was a randomised clinical trial of EVT plus usual care vs. usual care alone for patients with an intracranial occlusion. The primary outcome was the modified Rankin scale (mRS) score at 90 days. The primary effect parameter was the adjusted common odds ratio (acOR), estimated with ordinal logistic regression and adjusted for age and stroke severity at baseline. Treatment effect modification by AF was assessed using a multiplicative interaction variable. We included all 500 patients. In total, 135 (27%) had AF. These patients were older, had a worse pre-stroke mRS score and were less often treated with IV alteplase. In patients without AF, the estimated treatment effect was similar to the overall treatment effect (acOR 1.9, 95% CI: 1.3 to 2.7). In patients with AF, the treatment effect appeared lower (acOR 1.0, 95% CI: 0.6 to 1.9). The interaction of treatment effect and AF was not significant (p=0.09, after adjustment p=0.12).
Conclusions: This study did not show significant difference in the EVT effect between acute stroke patients with and those without AF.
Abbreviations
acOR: adjusted common odds ratio
AF: atrial fibrillation
AIS: acute ischaemic stroke
CI: confidence interval
cOR: common odds ratio
DSA: digital subtraction angiography
EVT: endovascular thrombectomy
MAP: mean arterial pressure
mRS: modified Rankin scale
mTICI: modified Thrombolysis In Cerebral Infarction
NIHSS: National Institutes of Health Stroke Scale
Introduction
Atrial fibrillation (AF) is associated with a four to five times increased risk of ischaemic stroke and causes approximately 15% of all acute ischaemic strokes (AIS)1,2. Patients with AIS due to AF are older, suffer from more severe neurological deficits, have a higher probability of remaining disabled and have higher mortality rates1-6. This unfavourable prognosis in AF patients could be due to the pathophysiology of infarction caused by AF. A higher proportion of white blood cells in clots of presumed cardioemoblic origin, extended recanalisation times and less favourable recanalisation have been reported7, but this was not confirmed in other studies8-10. Patients with cardioembolic stroke appear to have different occlusion locations and larger infarct volumes11.
Although a large randomised clinical trial of treatment with intravenous (IV) alteplase for AIS has not reported modification of treatment effect by AF12, other studies have suggested that patients with AF treated with IV alteplase have worse clinical outcomes after treatment3,4 and significantly higher rates of intracranial haemorrhage compared with patients without AF13.
Endovascular thrombectomy (EVT) with retrievable stents is a safe and effective treatment for patients with AIS caused by an intracranial arterial occlusion14-19. In these EVT trials, AF is more common (>30%) than in IV alteplase studies, which is probably related to the larger-sized emboli in AF. For this reason and on the assumption that infarcts caused by cardioembolic occlusions are less responsive to EVT, we investigated whether AF modifies treatment effect of EVT in patients with AIS in this pre-specified subgroup analysis of MR CLEAN20.
Methods
Full methods of the trial have been reported earlier14. Eligible patients had a proximal intracranial arterial occlusion of the anterior circulation that was confirmed on vessel imaging and that could be treated intra-arterially within six hours after symptom onset. Patients were randomised to EVT plus usual care or usual care alone. The trial was conducted in 16 stroke centres in the Netherlands. Approval was obtained from all ethics and research boards of participating centres, and all participants (or legal representatives) provided written informed consent. The trial procedures were in accordance with national and institutional guidelines.
OUTCOMES
The primary outcome was the modified Rankin scale (mRS) score at 90 days. Secondary outcome measures included neurological assessment with the National Institutes of Health Stroke Scale (NIHSS) at 24 hours and five to seven days or discharge if earlier and activities of daily living with the Barthel index at 90 days21,22. Radiological outcome measures included recanalisation on computed tomography angiography (CTA) at 24 hours, final infarct volume on CT at five to seven days and the modified Thrombolysis in Cerebral Infarction (mTICI) score on digital subtraction angiography (DSA) in the intervention arm23.
SAFETY
Safety parameters included haemorrhagic complications, progression of AIS, recurrent AIS, hemicraniectomy, other complications such as pneumonia or cardiac ischaemia, and death. Symptomatic intracranial haemorrhage was defined as neurological deterioration of four or more points on the NIHSS and confirmed with imaging.
CLINICAL DEFINITIONS
The acute diagnosis of AF could be based on pre-existing AF, identified through medical history, and de novo AF during hospitalisation. Although exact procedures of the latter differed in the various participating centres, all trial patients were monitored during the first 24 hours after AIS and the diagnosis of de novo AF was confirmed by 12-lead ECG. As all patients underwent CTA of cervical vessels before inclusion in the trial, we also assessed the presence of cervical carotid stenosis or occlusion.
STATISTICAL ANALYSIS
All analyses were based on the intention-to-treat principle. The primary effect parameter was the adjusted common odds ratio (acOR), estimated with ordinal logistic regression. Treatment effect modification by AF was assessed by means of a multiplicative interaction variable. Treatment effect and interaction were also assessed in all the secondary and safety effect parameters. The primary and all secondary effect parameters were adjusted for potential imbalances in major pre-specified prognostic variables adapted from the original trial protocol statistical analysis plan (age and stroke severity [NIHSS] at baseline). The analysis for the primary effect parameter was repeated after exclusion of the patients with cervical carotid stenosis or occlusion. The adjusted and unadjusted common odds ratios were reported with 95% confidence interval (CI) to indicate statistical precision. Binary outcomes were analysed with logistic regression and reported as adjusted and unadjusted odds ratios with 95% CIs. Continuous variables were analysed with linear regression and reported as adjusted and unadjusted beta values with 95% CIs. All reported p-values are two-sided. All statistical analyses are performed with Stata/SE 13.1 (StataCorp, College Station, TX, USA).
Results
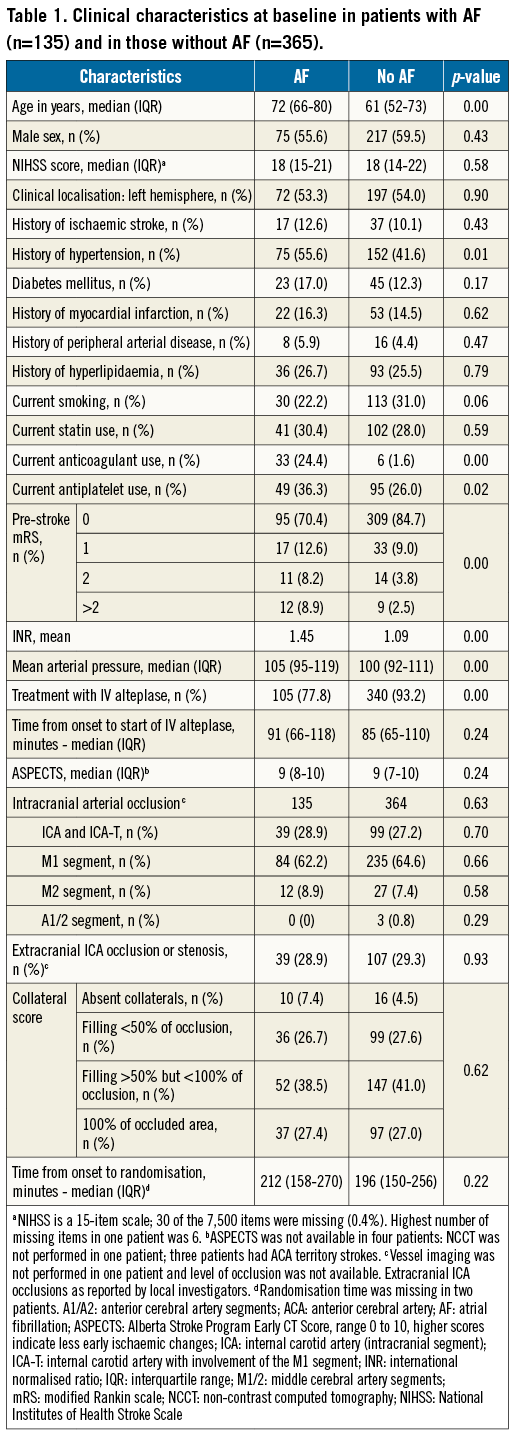
In total, 135 patients (27%) had AF, of whom 79 (58.5%) had pre-existing AF and 56 (41.5%) had de novo AF. Patients with AF were on average 12 years older, had a higher mean arterial pressure (MAP), were more likely to have a history of hypertension, and more often used anticoagulants and antiplatelet agents at baseline than patients without AF. Cervical carotid occlusions were equally present in patients with and in those without AF. Patients with AF also had a higher pre-stroke mRS score and were less likely to have been treated with IV alteplase (Table 1). Time from onset to intervention, duration of the procedure and chances did not differ between patients with and those without AF (data not shown).
PRIMARY OUTCOME
Data on functional outcome at 90 days were complete (Table 2). In total, 23 (17%) of all patients with AF and 104 (28%) of all patients without AF were functionally independent (mRS 0-2) (Table 2, Figure 1). The overall treatment effect favoured intervention and was statistically significant: the cOR was 1.7 (95% CI: 1.2 to 2.3) and the acOR was 1.7 (95% CI: 1.2 to 2.3). Although in patients without AF the treatment effect was similar to the overall effect in the study (cOR 2.0, 95% CI: 1.4 to 3.0 and acOR 1.9, 95% CI: 1.3 to 2.7), in AF patients the treatment effect seemed smaller. However, the unadjusted interaction of AF with treatment was non-significant (p=0.09) and was further attenuated after adjustment for age and NIHSS at baseline (p=0.12) (Figure 2). For the 354 patients without cervical carotid occlusion, the adjusted interaction of AF with treatment was also not significant (p=0.30).
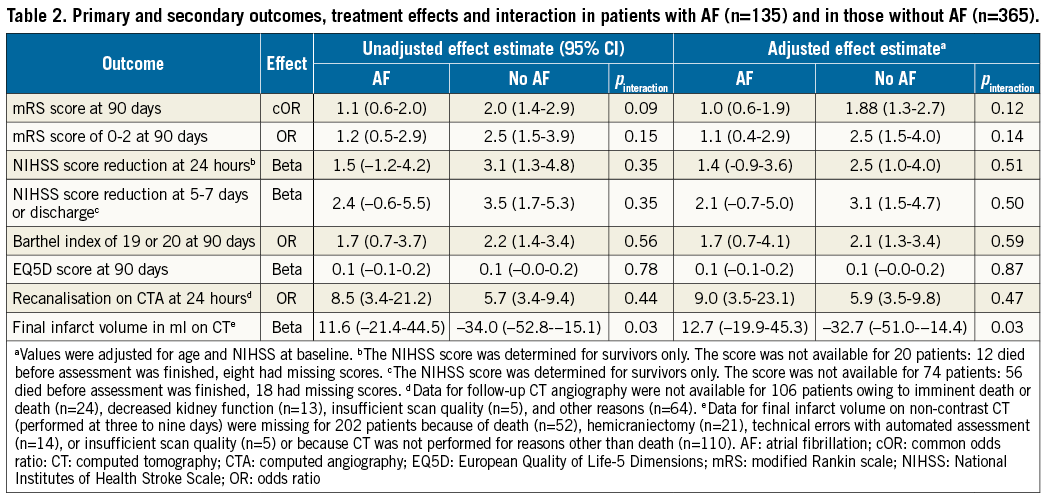
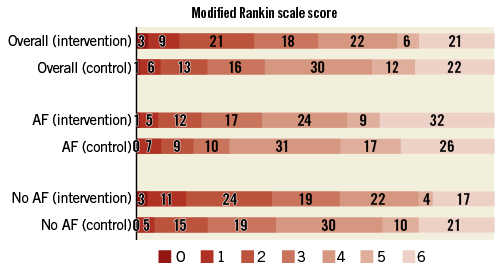
Figure 1. Effect of treatment on the distribution of the mRS scores at 90 days in the MR CLEAN trial. Shown is the distribution of scores on the modified Rankin scale. Scores range from 0 to 6, with 0 indicating no symptoms, 1: no clinically significant disability, 2: slight disability, 3: moderate disability, 4: moderately severe disability, 5: severe disability, and 6: death. Overall there was a significant difference between the intervention group and the control group in the overall distribution of scores in an analysis with univariable ordinal regression (adjusted cOR 1.67; 95% CI: 1.21 to 2.30). In patients without AF, the estimated treatment effect was similar to the overall treatment effect (acOR 1.9, 95% CI: 1.3 to 2.7). In patients with AF, the treatment effect appeared lower (acOR 1.0, 95% CI: 0.6 to 1.9). In the intervention arm, 18% of the patients with AF had an mRS of 2 or lower versus 38% of the patients without AF. Numbers are percentages.
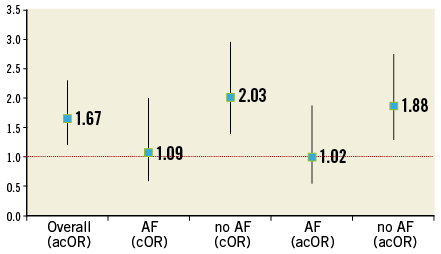
Figure 2. Modification of the effect of treatment by AF at baseline. Shown is the distribution of the common odds ratio of different patient groups (overall, patients with AF and patients without AF) after univariable ordinal regression and after adjustment of the treatment effect for age and stroke severity at baseline (adjusted common odds ratio). In patients without AF, the estimated treatment effect was similar to the overall treatment effect (acOR 1.9, 95% CI: 1.3 to 2.7). In patients with AF, the treatment effect appeared lower (acOR 1.0, 95% CI: 0.6 to 1.9). The interaction of treatment effect and AF was not significant (p=0.09, after adjustment p=0.12).
SECONDARY OUTCOMES
In patients without AF, the score on the NIHSS improved after five to seven days and was reduced with 3.1 points (95% CI: 1.5 to 4.7) whereas, in patients with AF, the NIHSS was not reduced significantly (2.1, 95% CI: -0.7 to 5.0). We found no interaction of AF with treatment for the secondary outcomes (NIHSS at 24 hours and five to seven days, Barthel index and EQ5D) (Table 2).
Recanalisation on CTA at 24 hours occurred in 80% (39/49) of the AF patients in the intervention arm and in 31% (16/51) of the AF patients in the control arm. In the patients without AF, recanalisation on CTA occurred in 78% (102/138) of patients in the intervention arm and in 33% (52/156) of patients in the control group. The interaction between AF and recanalisation was not significant (p=0.47). For final infarct volume on CT, the interaction of AF with treatment was significant (p=0.03). Patients with AF reached mTICI 2b/3 in 62% (38/61) of cases, and patients without AF did so in 57% (78/136) for a difference of 5% (95% CI: –20% to 10%) (p=0.52).
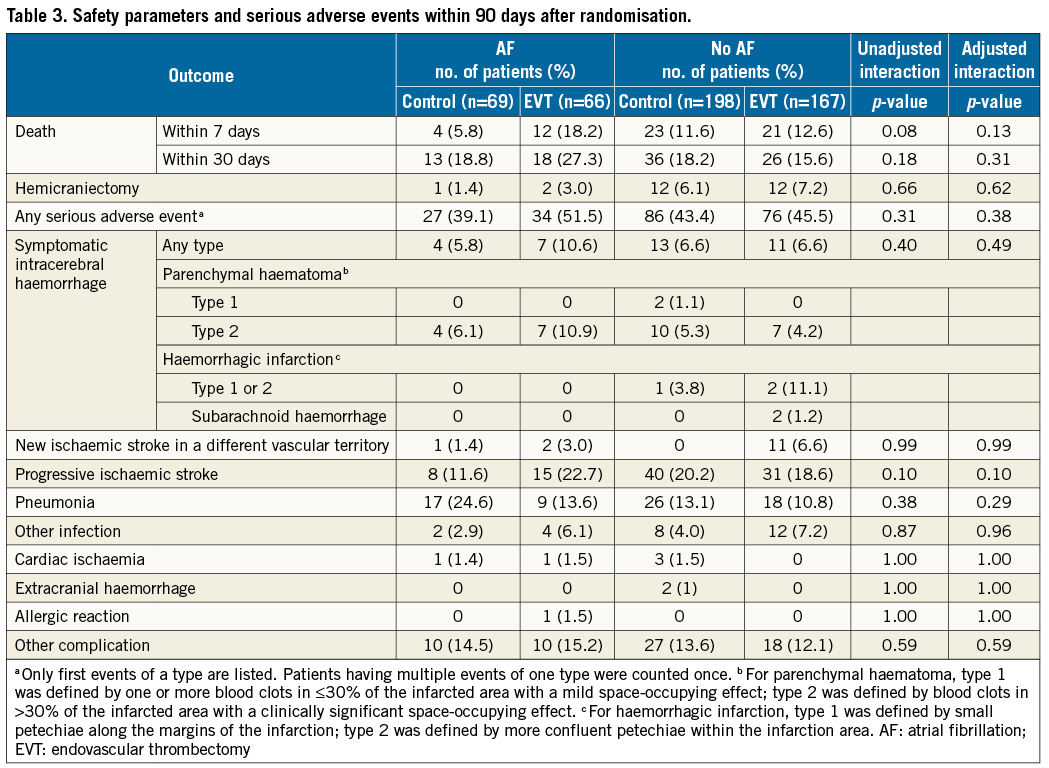
There were no significant differences in serious adverse events (SAE) between the AF and non-AF groups (Table 3). For mortality within seven days after randomisation, the interaction of treatment with AF was not significant (p=0.08) and was further attenuated after adjustment (p=0.13). More patients with AF in the intervention arm of the study died within seven days compared to patients in the control arm (12% difference, 95% CI: 1.5% to 23.2%). This significant difference (p=0.03) in mortality disappeared at 30-day follow-up. In the non-AF group, 11 (6.6%) patients in the intervention arm had a new AIS, whereas in the control arm there were no patients with new AIS. The AF group showed no such difference in new AIS between the intervention arm and the control arm.
Discussion
In this pre-specified subgroup analysis of the MR CLEAN trial, we looked for modification of the effect of EVT by AF, based on the assumption that patients with ischaemia caused by cardioembolic occlusions could be less responsive to treatment. Although the effect of treatment appeared smaller in patients with AF than in patients without AF, formal interaction testing was not statistically significant, meaning that we could not formally prove that EVT was less effective in patients with AF than in patients without AF.
Our assumption that patients with AF might respond less favourably to EVT than patients with ischaemic stroke of other aetiology was based on observations that patients with AF and ischaemic stroke generally do worse than those without AF, anecdotal reports of difficult clot removals in these patients, and studies reporting different composition of clots in AF patients7,9,10. Interaction testing is not a very sensitive way to assess differential treatment effects, especially so in moderately sized RCTs24. However, we showed that interaction terms and effects on the primary and all secondary outcomes consistently point in the direction of less treatment effect for patients with AF.
Most AF patients are treated with oral anticoagulants and therefore often have a contraindication for treatment with IV alteplase. We recently showed that patients who have not been pretreated with alteplase experience similar treatment effects25. It is not known whether periprocedural use of anticoagulation or antiplatelet therapy in these patients is effective26. Patients with AF were older and had a worse functional condition pre-stroke than patients without AF. These factors may result in a relatively poor prognosis at baseline. Although adjustment for age and stroke severity only slightly attenuated our results, it is difficult to compare patient groups with a 12-year difference reliably despite this statistical adjustment. The age difference could therefore partially explain the worse outcomes in the AF group. AF patients in our study did not have a larger infarct volume as has been reported by others. This is probably due to selection of patients with intracranial embolic occlusions, which excludes small and lacunar infarctions. However, the reduction in infarct volume was smaller in AF patients than in patients without AF. This may partially explain our results. In patients with cervical carotid obstruction and AF, stroke may possibly be caused by the carotid lesion instead of AF. However, exclusion of patients with carotid stenosis or occlusion did not change our results. Finally, microscopic and macroscopic thrombus characteristics were not available; however, a recent systematic review did not report differences between AF and non-AF patients in microscopic or macroscopic thrombus characteristics27.
Other randomised trials of EVT for AIS included comparable proportions of AF patients (35%-38%), but did not report on possible treatment effect modification by AF15-18. The pooled analysis of the five recent thrombectomy trials does not report on treatment effect modification by AF19.
Two earlier studies analysed differences in treatment effect between AF and non-AF patients28,29. The IMS III investigators reported smaller effect sizes of EVT for patients with AF but reported no interaction term28. The SYNTHESIS investigators also reported smaller effect sizes in AF patients; however, the interaction was not significant (p=0.85)29. Moreover, as this concerns neutral trials, the results of subgroup analyses have to be interpreted with care.
Limitations
This study has several limitations. The subgroup of patients with AF (n=135) was relatively small, limiting the precision of our estimates. Secondly, we merged patients with a history of AF and patients with de novo AF. The latter group may have had AF before the AIS but could also have acquired AF as a result of their AIS. This may have resulted in an overestimation of patients with a true cardioembolic origin of their intracranial occlusion. However, stroke risk does not differ according to AF pattern (chronic or paroxysmal)30.
Conclusions
To the best of our knowledge, this analysis is the first to investigate the modification of the effect of EVT for patients with AIS caused by a proximal intracranial occlusion of the anterior circulation by AF. This study did not show significant difference in the EVT effect between acute stroke patients with and those without AF. Although the effect of EVT appeared to be absent in patients with AF, this study could not prove that AF modified the effect of EVT. A more precise estimate in pooled data from the thrombectomy trials is needed.
| Impact on daily practice The findings of this study do not support withholding endovascular thrombectomy in patients with atrial fibrillation and acute ischaemic stroke. |
Funding
The MR CLEAN trial was supported by the Dutch Heart Foundation and by unrestricted grants from AngioCare BV, Medtronic/Covidien/ev3, MEDAC Gmbh/LAMEPRO, Penumbra Inc., Stryker and Top Medical/Concentric.
The trial is registered under number NTR1804 in the Dutch trial register and under ISRCTN10888758 in the ISRCTN register.
Conflict of interest statement
Erasmus MC received funds from Stryker, Servier Cardiovascular and Bracco Imaging for consultations by D. Dippel. AMC received funds from Stryker for consultations by C. Majoie. MUMC received funds from Stryker and Codman for consultations by W. van Zwam. The other authors have no conflicts of interest to declare.