Abstract
Aims: The aim of this study was to investigate the prognosis in patients with atrial fibrillation (AF) and intracerebral haemorrhage (ICH) having a left atrial appendage occlusion (LAAO) versus patients receiving standard medical therapy.
Methods and results: A total of 151 patients from the Nordic countries with AF and previous ICH who underwent LAAO using the AMPLATZER Cardiac Plug or the AMPLATZER AMULET were compared to a propensity score-matched group of 151 patients receiving standard medical therapy. The two groups were matched so that their risks for stroke and bleeding were similar (CHA2DS2-VASc and HAS-BLED scores). The standard care patients were identified from the Danish Stroke Registry among 787 patients with AF and ICH. The primary endpoint was a composite of all-cause mortality, ischaemic stroke and major bleeding. Patients with AF and a prior ICH treated with LAAO had a lower risk of the composite outcome as compared to patients treated with standard medical care (events/1,000 years [95% confidence interval]: 53.3 [44.3-64.1] vs. 366.7 [298.2-450.9]; hazard ratio 0.16 [0.07-0.37]).
Conclusions: LAAO is suggested to be of major clinical benefit in AF patients having sustained an ICH. These results have to be confirmed in a randomised clinical trial.
Abbreviations
ACP: AMPLATZER Cardiac Plug
AF: atrial fibrillation
ICH: intracerebral haemorrhage
LAAO: left atrial appendage occlusion
OAC: oral anticoagulation
Introduction
Oral anticoagulation (OAC) is effective in reducing the risk of cardioembolic stroke in patients with atrial fibrillation (AF)1. However, OAC carries a risk of major bleeding including intracerebral haemorrhage (ICH). A history of spontaneous or OAC-associated ICH increases the risk of recurrent ICH and many patients with AF and ICH are therefore denied OAC due to the fear of recurrent ICH2,3. These unprotected AF patients have a high cardioembolic risk that might even exceed the risk of recurrent ICH4. The question of whether to resume OAC in a patient with AF following an ICH remains a clinical dilemma.
Percutaneous left atrial appendage occlusion (LAAO) may potentially be a solution to this clinical dilemma. LAAO is increasingly used to reduce the risk of stroke and bleeding in patients with AF5,6. The randomised PROTECT-AF trial showed that LAAO with the WATCHMAN™ device (Boston Scientific, Marlborough, MA, USA) was superior to OAC in the primary combined endpoint of stroke, bleeding and mortality after four years7. The study was, however, carried out in AF patients eligible for warfarin. Treatment by warfarin for 45 days is recommended after WATCHMAN implantation whereas the AMPLATZER™ Cardiac Plug (ACP) or the newer AMPLATZER™ AMULET™ (both St. Jude Medical, St. Paul, MN, USA) is implanted using only antiplatelet therapy in the post-procedural period.
Currently, transcatheter LAAO is primarily used in AF patients who have a contraindication to or do not tolerate OAC, including patients with a previous ICH. Observational registry studies suggest that LAAO reduces the risk of stroke and bleeding when compared to the predicted rates of stroke and bleeding6. However, such studies may be misleading as a result of bias in selecting patients for LAAO and lack of appropriate comparator groups. So far, there has been no randomised clinical trial of LAAO in AF patients with a previous ICH.
The aim of this study was to compare the clinical outcome, including ischaemic stroke, major bleeding and all-cause mortality, in AF patients with a previous ICH having LAAO with those treated by standard medical therapy in a propensity score-matched follow-up study.
Methods
STUDY POPULATION
LAAO GROUP
We identified all AF patients with a prior ICH who underwent LAAO with the ACP or the AMPLATZER AMULET at one of the eight largest Nordic LAAO centres (Denmark: Aarhus and Copenhagen; Finland: Turku, Helsinki and Tampere; Sweden: Stockholm, Gothenburg and Lund) (n=176). Patients were identified from the beginning of LAAO at each centre covering the time period from 2009 until 1 March 2015. During this period, the total number of AMPLATZER LAAO cases carried out in the eight institutions was 397. In 176/397 (44%) the indication for LAAO was a previous ICH. The median time from ICH to LAAO was 189 days (25-4,533 days).
STANDARD CARE GROUP
ICH patients with AF who survived at least 180 days after admission with ICH between 2005 and 2014 were identified in the Danish Stroke Registry (DSR) (n=787)8. Information on vital status was obtained from the Danish Civil Registration System9. The criterion of at least 180 days survival was used to exclude those patients who were very sick or disabled after their ICH and who therefore would not represent adequate candidates for LAAO or antithrombotic therapy.
EFFICACY AND SAFETY OF LAAO
Data on procedural success and periprocedural complications (0-7 days) were registered. Periprocedural complications were registered according to the EHRA/EAPCI expert consensus statement10 and included death, ischaemic stroke, TIA, haemorrhagic stroke, pericardial effusion/tamponade, valvular complications, device migration/embolisation, major bleeding, pulmonary oedema, myocardial infarction, pulmonary embolism and arrhythmia requiring treatment.
CLINICAL OUTCOMES
We assessed the following clinical outcomes separately and as a composite outcome: acute ischaemic stroke, major bleeding and all-cause mortality. Major bleeding was defined as intracranial haemorrhage, hospitalisation needed because of bleeding, decrease in Hb >2 g/dL or requiring blood transfusion.
In the LAAO group, the information on outcomes was obtained at planned clinical follow-up visits and from medical records, supplemented by data from national registries for vital status and hospital admissions. In the standard care group, outcome data were obtained from the Danish Civil Registration System (mortality), the DSR (ischaemic stroke) and the Danish National Registry of Patients (major bleedings). The Danish National Registry of Patients comprises data, including diagnoses and surgical procedures, on all discharges from all non-psychiatric hospitals in Denmark since 197711.
COVARIATES
Data needed for the calculation of the CHA2DS2-VASc and HAS-BLED risk scores were obtained. Those parameters include age, sex, previous stroke, congestive heart failure/ventricular dysfunction, hypertension, diabetes mellitus, vascular disease, abnormal renal function, abnormal liver function, prior major bleeding or predisposition, and drugs predisposing to bleeding. We excluded the parameter of labile INR values from the HAS-BLED score as this information was not available for the standard care group. The CHA2DS2-VASc score is widely used and considered the best estimate for predicted stroke risk in AF patients12, while HAS-BLED is the most widely accepted risk score for prediction of bleeding in AF patients13.
Furthermore, data on the use of oral anticoagulants and antiplatelets during follow-up were obtained from medical records (LAAO group) or through linkage with the Danish National Database of Reimbursed Prescriptions14 (standard care group).
The study was approved by the Danish Data Protection Agency (ID 1-16-02-371-13). According to Danish law, ethical approval is not required for registry-based studies. In Finland and Sweden, the study was approved by ethics committees.
DATA ANALYSIS AND STATISTICS
We used a time-dependent propensity score matching (nearest neighbour matching) method to reduce the risk of bias due to confounding. We aimed to match each LAAO patient with one standard care patient with a similar propensity score using replacement. The propensity score was based on the clinical parameters in the CHA2DS2-VASc and HAS-BLED risk scores assessed on the day of the LAAO procedure (LAAO patients), or on the corresponding day after admission with ICH for matched standard care patients. In brief, for an LAAO patient with treatment at time “t” post ICH, possible controls would include patients without LAAO and still at risk (not censored, not yet having had an outcome event) at time “t”. The propensity score for the standard care group was updated over time post ICH using longitudinal data to ensure the best possible balance at time zero in the regression model. The calliper was chosen as 0.2 times the standard deviation of the logit propensity score. An absolute standardised difference <10% and a variance ratio between 0.8 and 1.25 were considered to support the assumption of balance between the groups.
Follow-up started at the day of LAAO procedure (LAAO patients) or at the corresponding day after admission with ICH for matched standard care patients (the same time interval from index ICH to the start of follow-up in the two groups) and ended at the day of the first outcome event (death, ischaemic stroke or major bleeding, respectively), date of emigration, death (in the analyses on ischaemic stroke and major bleeding) or the end of the study period, whichever came first. Because of the gap of inclusion periods for LAAO-treated and standard care patients, the maximum follow-up time for each propensity score-matched pair potentially diverges. Therefore, we ensured identical maximum follow-up time for each pair defined by the shortest maximum follow-up time in the match. The matching was followed by construction of Kaplan-Meier survival curves and Cox proportional hazards regression. We used a robust sandwich estimator to estimate standard error.
In a sensitivity analysis, we propensity score-matched the LAAO cohort (n=176) with the standard care patients in the DSR database (n=787) according to CHA2DS2-VASc and HAS-BLED risk scores. However, in this additional analysis only standard care patients who had resumed or started OAC within 180 days after their index ICH were included. As it was only possible to match few patients in this analysis on time from index ICH to LAAO procedure or the corresponding day for standard care patients, we used an alternative approach and started follow-up at the day of LAAO for LAAO patients or at day 180 after ICH in the OAC-treated standard care patients.
All data analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC, USA).
Results
EFFECTIVENESS AND SAFETY OF LAAO PROCEDURE
LAAO was successful in 172 of 176 cases (97.7%). The rate of periprocedural complications was 4.0% (7/176). There were no procedure-related deaths or ischaemic strokes. One patient with a history of cerebral amyloid angiopathy and multiple ICHs had a small new ICH at day 1, but showed rapid and full spontaneous recovery. One patient had pericardial effusion/tamponade and another had device migration/embolisation. One patient had haematemesis and three patients had femoral vein access-site bleedings.
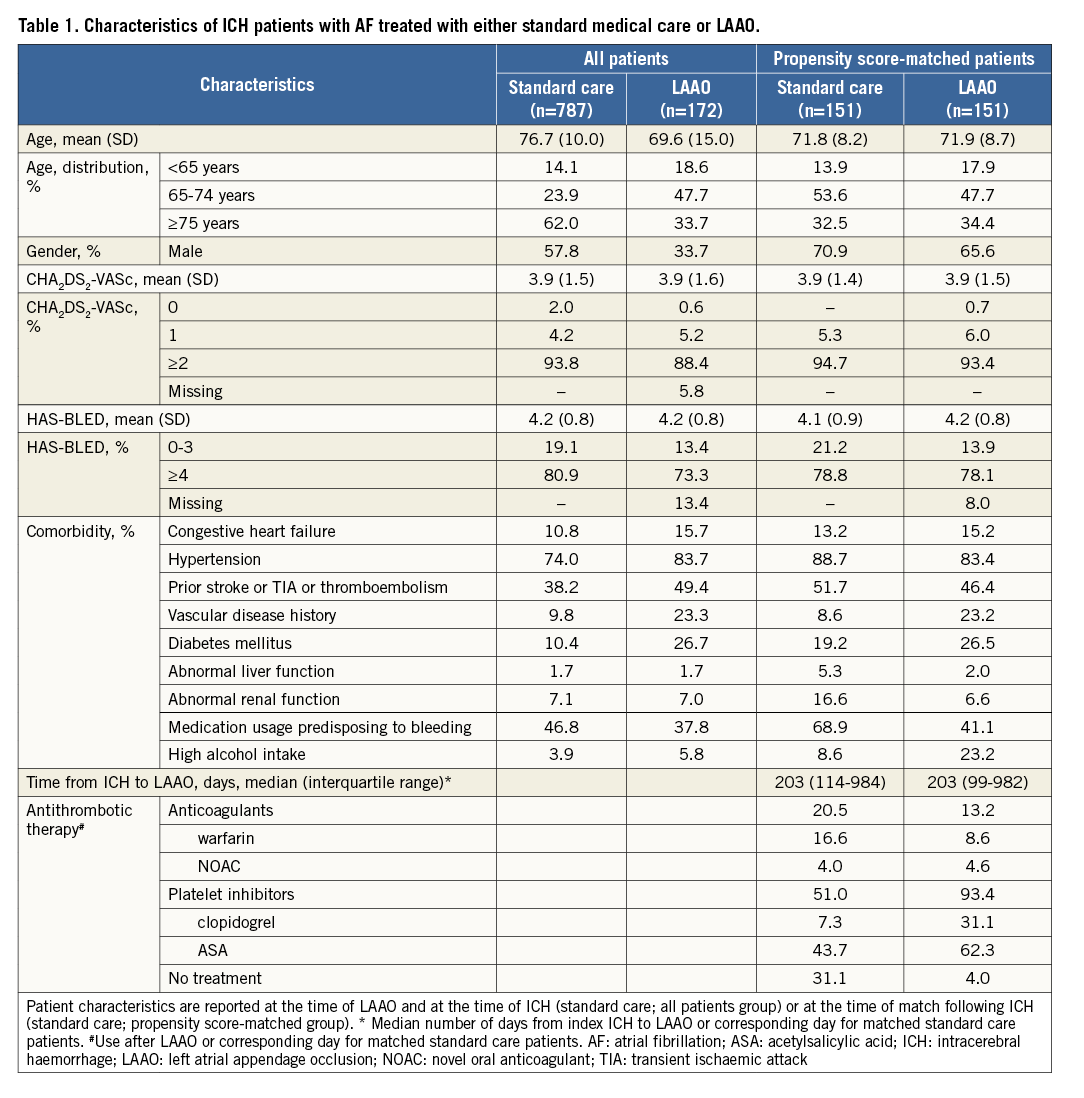
PATIENT CHARACTERISTICS
A total of 787 AF patients who survived more than 180 days after admission for ICH were identified in the DSR. We were able to match 151 patients from the LAAO group with 151 patients from the standard care group. Patient characteristics for the LAAO and standard care groups before and after matching are shown in Table 1.
CLINICAL OUTCOMES
The median follow-up time was 182 days (25%/75% quartile: 88/372 days). The event rate for the composite endpoint of ischaemic stroke, major bleeding and all-cause mortality was significantly lower in the LAAO group than in the standard medical care group (events/1,000 years [95% confidence interval]: 53.3 [44.3-64.1] vs. 366.7 [298.2-450.9]). The clinical outcomes are presented in Table 2, and Kaplan-Meier curves for the composite outcome of ischaemic stroke, major bleeding and all-cause mortality among the propensity score-matched LAAO and standard care patients are shown in Figure 1.
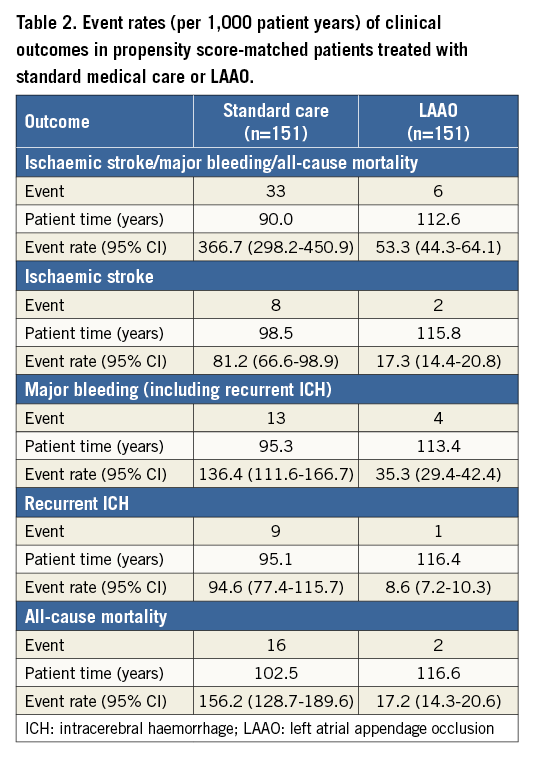
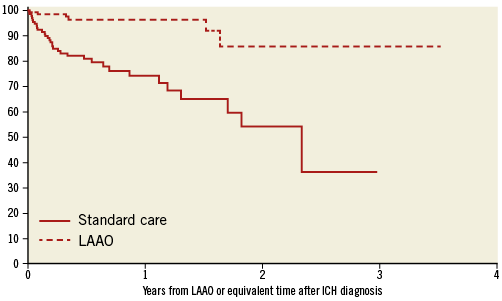
Figure 1. Kaplan-Meier curves for event-free survival. Kaplan-Meier survival curves for the composite outcome (ischaemic stroke, major bleeding, all-cause mortality) in propensity score-matched AF patients with a prior ICH treated with left atrial appendage occlusion (LAAO; dotted line) or standard medical care (solid line). Follow-up started at the day of procedure for patients with LAAO or corresponding day after admission for ICH for patients in the standard care group.
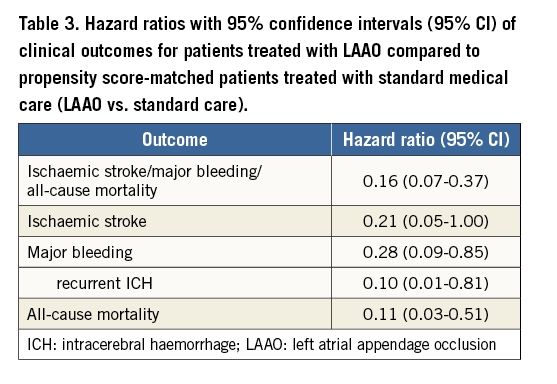
The lower event rates observed among the LAAO patients are also reflected by the propensity score-matched hazard ratios (HR) for the clinical outcomes, which are shown in Table 3. Patients with AF and a prior ICH treated by LAAO had a significantly lower risk of all-cause mortality (HR 0.11 [0.03-0.51]), major bleeding (HR 0.28 [0.09-0.85]), recurrent ICH (HR 0.10 [0.01-0.81]) as well as the composite outcome (HR 0.16 [0.07-0.37]) as compared to patients treated by standard medical care. The risk of ischaemic stroke (HR 0.21 [0.05-1.00]) was borderline statistically significantly lower.
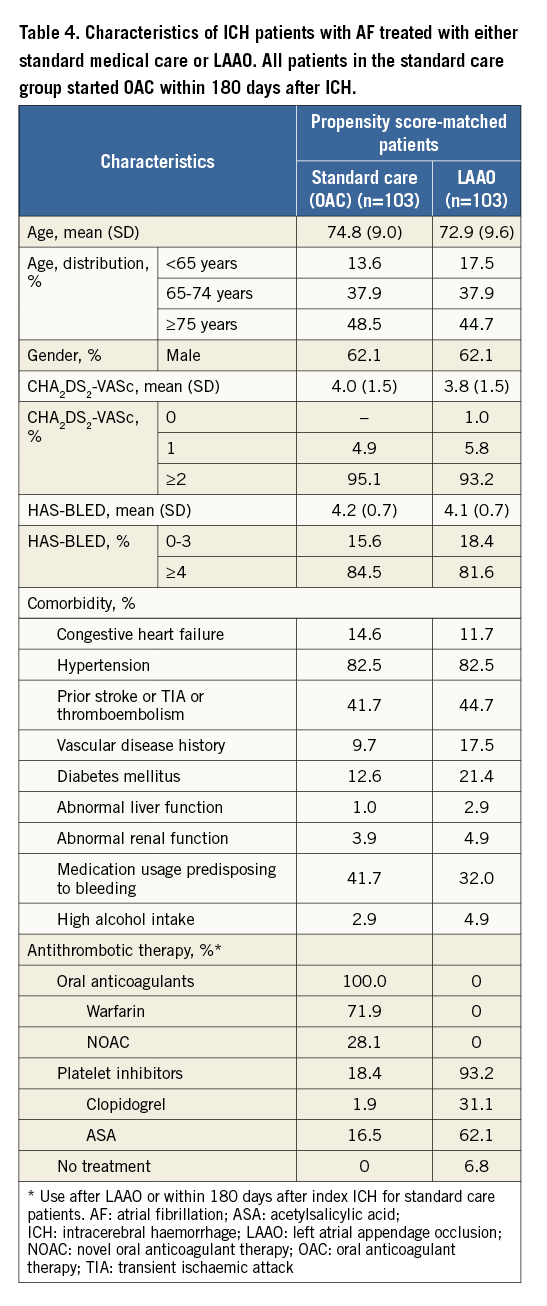
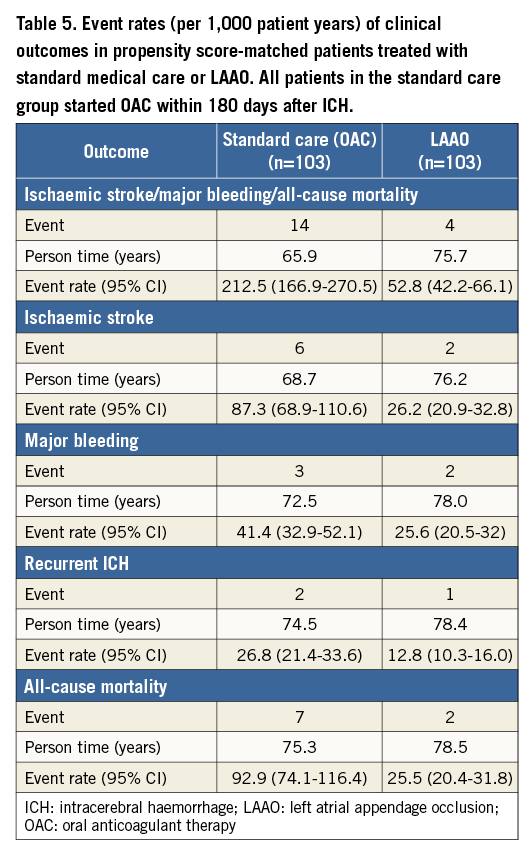
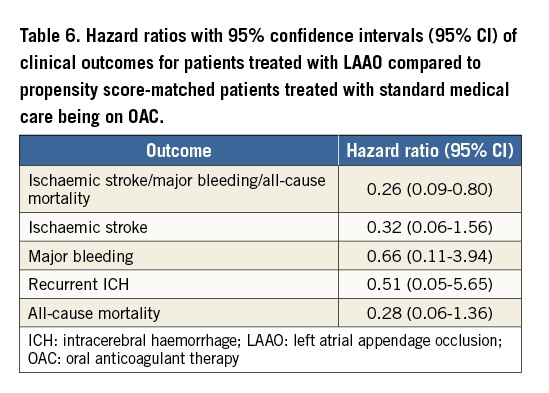
When LAAO patients, in a separate analysis, were compared with standard care patients who were all treated with OAC within 180 days after their index ICH, we were able to propensity score match 103 LAAO patients with 103 standard care patients. The median time from index ICH to LAAO among the LAAO patients in this analysis was 211 days (interquartile range: 108-1,248). The characteristics of these patients are presented in Table 4. In this additional analysis, there was a significantly lower risk with LAAO vs. OAC treatment in the combined clinical outcome of ischaemic stroke, major bleeding and mortality with an HR of 0.26 [0.09-0.80]. HR and rates for the separate events were numerically favourable for LAAO, although these analyses did not reach statistical significance (Table 5, Table 6).
Discussion
In this propensity score-matched follow-up study among Nordic patients with AF and a previous ICH, we found LAAO to be associated with a substantially lower risk of the composite endpoint of ischaemic stroke, major bleeding and all-cause mortality when compared to standard medical care. Among the separate clinical outcomes, LAAO was associated with a significantly lower risk of all outcomes except for ischaemic stroke, which was only borderline significant.
The procedural success of LAAO using the AMPLATZER devices was high (98%) with a low periprocedural complication rate (4%). This corresponds well with data reported from the large European/Canadian registry study of the ACP (n=1,047) where the procedural success was 97% and the periprocedural adverse event rate was 5%6. Data from the eight Nordic centres in this study included cases from the beginning of LAAO in all centres and therefore also included the learning curve for the procedure.
In the standard care group of patients, 31% did not receive any antithrombotic treatment during follow-up, reflecting the reluctance to resume antithrombotic drug therapy in AF patients having sustained an ICH. Platelet inhibitors were given in 51% and OAC in 21%. In the LAAO group, 93% were treated with platelet inhibitors after LAAO. The majority received ASA monotherapy. Randomised studies have shown that antiplatelet therapy is inferior to OAC for stroke prevention in patients with AF. Thus, the observed lower ischaemic stroke rate in the LAAO group is unlikely to be explained by differences in antithrombotic treatment between the two groups. The more frequent use of OAC in the standard care group may possibly have added to the observed higher rate of major bleeding in this group.
ASA monotherapy was the preferred post-implantation antithrombotic therapy in five out of the eight participating LAAO centres. A recent study from the largest of the eight LAAO centres has shown a low rate of device-related thrombosis of 1.9%, suggesting ASA monotherapy to be sufficient with AMPLATZER LAAO devices15.
Our study is the largest controlled observational study so far of LAAO involving real-life patients with AF and previous ICH. Previous ICH is a serious contraindication to OAC therapy and a leading indication for referral to LAAO in the Nordic countries. A small single-centre case series of 20 patients with AF and a previous ICH treated with the AMPLATZER Cardia Plug also showed LAAO to be safe and effective16. In a recent observational study, LAA ligation with the LARIAT® device (SentreHEART, Palo Alto, CA, USA) was reported to be safe and effective in a group of 139 AF patients ineligible for oral anticoagulation therapy17.
Strengths and limitations
The strengths of this study include the multinational design with inclusion of all consecutively treated LAAO patients from the largest Nordic centres, the propensity score-matched design and the complete follow-up.
Although we achieved a well-balanced match on all elements of the CHA2DS2-VASc and HAS-BLED risk scores between the LAAO and the standard care group, we cannot exclude the possibility that our results remain influenced by confounding factors because of the observational nature of the study. Indeed, confounding by indication due to selection of patients for LAAO with a high predicted chance of long-term survival pending a successful LAAO procedure is likely to be the most important methodological challenge to our study, as we lacked information on clinical characteristics that may play an important role both for prognosis and when deciding which preventive strategy to use (e.g., location and size of the index ICH, presence of microbleeds). We tried to address this problem by ensuring that all patients in the standard care group had survived at least 180 days after the ICH, by using time-dependent propensity score matching and by ensuring that time from the index ICH to the day of LAAO or the corresponding day for the standard care group was well balanced. Furthermore, we performed an additional analysis in which we only included OAC-treated patients in the standard care group based on the presumption that OAC would only be considered relevant in case the treating physician predicted that the patient would have a good chance of long-term survival. Also in this additional propensity score analysis, LAAO showed statistically significant superiority in the combined endpoint of ischaemic stroke, major bleeding and mortality when compared with standard care (OAC). However, it should be noted that it was not possible to ensure balance between LAAO patients and standard care patients on time from index ICH to LAAO or the corresponding day for the standard care patients in this analysis. In addition, we were not able to match all LAAO patients with suitable standard controls, which leaves room for potential selection bias. This applies both to the primary analysis as well as to the sensitivity analysis. Caution is therefore required when interpreting our findings.
Furthermore, different data capture procedures were applied in the DSR versus the Nordic LAAO database, and the statistical precision was moderate to poor in some of the analyses, even though our study is the largest so far examining the effectiveness and safety of LAAO among AF patients and previous ICH.
Conclusions
This observational propensity score-matched study suggests a potential therapeutic benefit of LAAO over standard medical therapy for prevention of stroke, major bleeding and death in patients with AF and a previous ICH. The inherent limitations of the observational study design require these results to be confirmed in a randomised clinical trial.
| Impact on daily practice Anticoagulation is controversial in AF patients with a prior ICH. Patients treated by LAAO had a significantly lower risk of the combined outcome of stroke, major bleeding and mortality compared with standard medical care in a propensity score-matched follow-up study. LAAO seems to be a promising stroke prevention strategy in patients with AF and a prior ICH. |
Funding
This study was supported by an unrestricted research grant from St. Jude Medical.
Conflict of interest statement
J. Nielsen-Kudsk, J. Lund and J. Odenstedt are proctors for St. Jude Medical. The other authors have no conflicts of interest to declare.