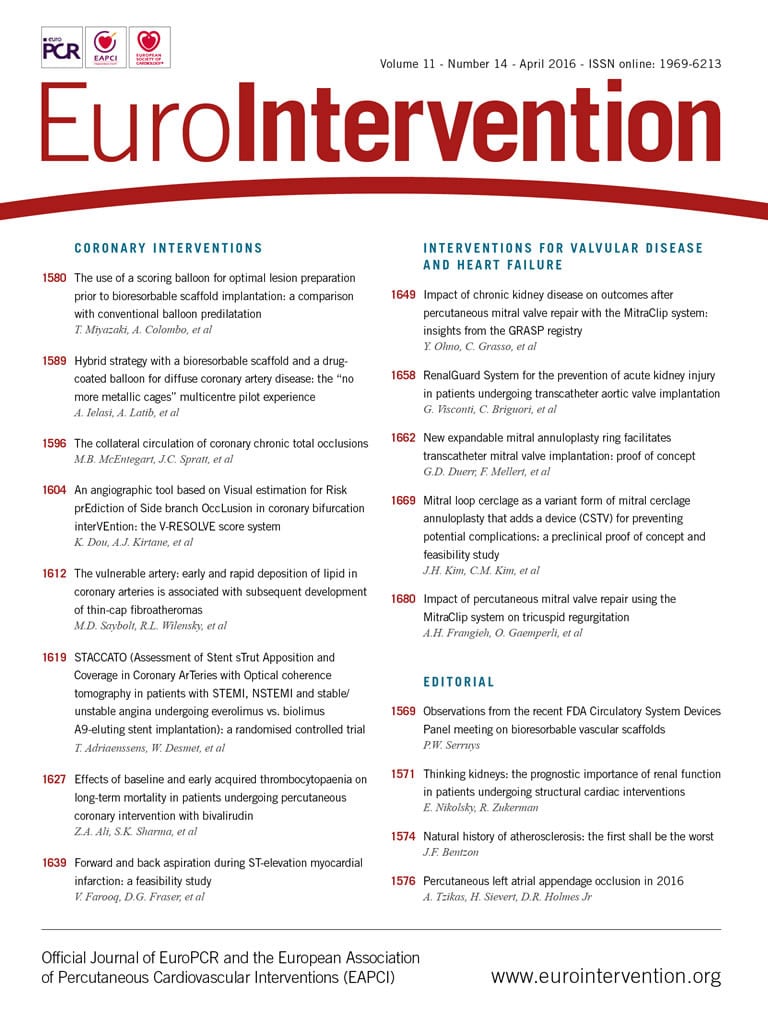
Percutaneous left atrial appendage (LAA) occlusion has been developed as an alternative, non-pharmacological treatment for stroke prevention in patients with non-valvular atrial fibrillation (AF)1-4. Oral anticoagulation (OAC) with warfarin or novel oral anticoagulation agents (NOACs), such as dabigatran, rivaroxaban, apixaban, etc., has been considered the gold standard therapy5. However, OAC therapy with any of the current agents is associated with an increased risk of bleeding, the potential for drug-drug interactions such as triple therapy (OAC and two antiplatelet drugs), and compliance both early and later, with up to 20-25% of patients discontinuing the drugs at intermediate-term follow-up, thus leaving them unprotected. Percutaneous LAA occlusion has gained increasing attention from physicians and patients alike, especially for patients with an increased bleeding risk. The most widely studied device for LAA closure is the WATCHMAN™ device (Boston Scientific, Marlborough, MA, USA). It is the only device that has been evaluated in randomised clinical trials and is the only device approved for stroke prevention in the USA1-3. However, other devices such as the AMPLATZER™ Cardiac Plug and the AMPLATZER™ Amulet™ (both St. Jude Medical, St. Paul, MN, USA) are widely used globally (Figure 1)4.

Figure 1. The most commonly used devices for LAA closure. A) The WATCHMAN (Boston Scientific). B) The AMPLATZER Amulet (St. Jude Medical).
Safety
The safety of percutaneous LAA closure was a concern during the early phases of technology development. Periprocedural major adverse events (MAEs), including pericardial bleeding/tamponade, stroke, device embolisation, etc., occurred in 5-7% of patients in PROTECT AF and other studies, reflecting the learning curve effect of a relatively complex procedure1-4. Indeed, the need for transseptal access, the fragility and enormous anatomical variability of the LAA placed LAA closure among the most challenging procedures, both for interventional cardiologists and for electrophysiologists. Fortunately, the results of subsequent randomised trials such as PREVAIL3 and reports from registries have documented a decrease of MAEs to 2-3% of patients6. Nevertheless, LAA closure is a preventive therapy and an even lower MAEs rate (<1%) remains the goal. This can be achieved with careful patient selection criteria, improvements in device design, advancements in cardiac imaging, and, more importantly, by following specific guidelines regarding physician training and certification to perform LAA closure procedures7.
Efficacy
The four-year results of the PROTECT AF study showed a remarkable decrease in all-cause mortality for the intention-to-treat patient population who underwent LAA closure with the WATCHMAN device as compared to patients receiving warfarin (HR 0.66, 95% CI: 0.45-0.98; p=0.04)3. The magnitude of this improvement has not been seen with either warfarin or NOACs8. In addition, the randomised trials with WATCHMAN have shown an approximately 80% reduction in haemorrhagic stroke compared with warfarin. The magnitude of this specific reduction is also greater than that seen in the meta-analyses of NOACs versus warfarin3,8. Non-randomised multicentre registries with broader patient groups have also confirmed favourable outcomes in patients not eligible for OACs, with a 59-77% reduction in stroke and bleeding as compared to individual patient risk predicted by CHA2DS2-VASc and HAS-BLED scores4,6. Although LAA occlusion has not yet been randomly evaluated in patients not eligible for OACs, it is widely used globally and is now the focus of a randomised trial, the ASAP-TOO. Large-scale studies comparing LAA occlusion with NOACs are still pending. Scientific concerns that AF is a systematic disease affecting parts of the left atrium other than the LAA, the role of peri-device leaks and device thrombosis (observed in approximately 4% of patients), and the lack of long-term data on large patient populations are issues that need to be studied more carefully. Nevertheless, notwithstanding the improvements of drug therapies in terms of safety and efficacy, the management of patients with AF remains challenging in everyday clinical practice, particularly for patients who are not good candidates for OAC due to previous bleeding, renal impairment, high risk of falling, coronary artery disease and stenting, etc.
Future perspectives
Certainly, LAA closure addresses an unmet clinical need for patients with AF: adequate efficacy in stroke prevention without major bleeding events. Improvements in periprocedural safety are achieved gradually. However, the choice, dosage and duration of antithrombotic medication post LAA closure need to be clearly determined, especially in the era of NOACs. Relevant studies are being designed and initiated but it will take several years for their results to emerge. In the meantime, conceivably, it would be more reasonable to prioritise LAA closure for patients who would benefit more, such as those with previous major bleeding (intracranial, gastrointestinal or other), renal impairment, very elderly, etc.9. Another important consideration for the implementation of any new therapy is cost. Initial results with the WATCHMAN device demonstrated LAA closure to be cost-effective and cost-saving for stroke risk reduction in patients with non-valvular AF and contraindications to warfarin10. Of course further studies using NOACs are needed.
Conclusions
In conclusion, percutaneous LAA occlusion has been documented to be an alternative to chronic OAC for stroke prevention in selected patients with non-valvular AF in both randomised clinical trials and registries, with a reduction in haemorrhagic stroke and improvement in survival. There remains an unmet clinical need to decrease the burden of AF-related strokes and at the same time decrease the rate of major bleeding events associated with long-term OAC therapy. Despite the observed reduction in periprocedural safety events, further improvements are required for this technically demanding, preventive procedure. Continued scientific study will allow further conclusions for optimal patient selection criteria.
Conflict of interest statement
A. Tzikas is a consultant, proctor and has received speaker honoraria and research grants from St. Jude Medical. The Mayo Clinic and D. Holmes have licensed technology for LAAO to Boston Scientific. H. Sievert’s institution has ownership interest in or has received consulting fees, travel expenses or study honoraria from the following companies: Abbott, Access Closure, AGA, Angiomed, Arstasis, Atritech, Atrium, Avinger, Bard, Boston Scientific, BridgePoint, Cardiac Dimensions, CardioKinetix, CardioMEMS, Coherex, Contego, CSI, EndoCross, EndoTex, Epitek, Evalve, ev3, FlowCardia, Gore, Guidant, Guided Delivery Systems, Inc., InSeal Medical, Lumen Biomedical, HLT, Kensey Nash, Kyoto Medical, Lifetech, Lutonix, Medinol, Medtronic, NDC, NMT, OAS, Occlutech, Osprey, Ovalis, Pathway, PendraCare, Percardia, pfm medical, Rox Medical, Sadra, SJM, Sorin, Spectranetics, SquareOne, Trireme, Trivascular, Velocimed, Veryan.