The highlight of the World Stroke Congress in Istanbul, 2014, was the presentation of the Dutch randomised trial - MR CLEAN – the first study demonstrating the superiority of catheter-based thrombectomy (CBT) over the best medical therapy, including intravenous thrombolysis1. Just a few months later, a series of randomised trials, performed in various countries, confirmed these initial results. All of these trials demonstrated improved functional outcomes, but the differences in overall mortality were not significant.
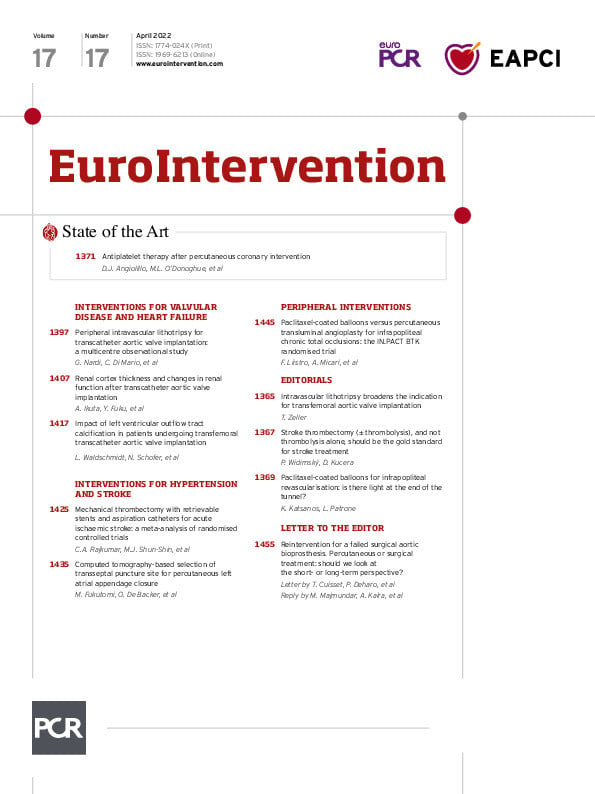
In the current issue of EuroIntervention, Rajkumar et al2 present a meta-analysis of 12 randomised trials, with 2,558 patients suffering acute anterior ischaemic stroke. The main finding of this meta-analysis is that thrombectomy reduced all-cause mortality at 90 days (16.1% vs 19.2%, odds ratio [OR]: 0.81, 95% confidence interval [CI]: 0.66-0.99; p=0.024). Despite intracranial manipulation with catheters, the rates of symptomatic intracranial haemorrhage did not differ between CBT patients and the control group. A very important observation for clinical practice is that for every 5.4 patients treated with thrombectomy, one less patient will be dependent at 90 days. Put into context, for thrombolysis, the number needed to treat is 18, i.e., 18 stroke patients need to be treated with thrombolysis to prove clinical benefit for one patient. In other words, mechanical thrombectomy is 3.3 times more effective than thrombolysis. Furthermore, this paper includes an important message for the cardiology community: “…to rapidly expand the pool of specialists able to perform the technique…it may be possible to utilise interventional cardiology teams, which are already on-call 24/7 to treat thrombi in the coronary circulation, although comprehensive training would be required to apply their existing skills to a new vascular bed.”
Thus, there is no doubt that CBT is the most effective treatment of acute ischaemic stroke. This has been known for seven years - since early 2015 - when the first five randomised trials were published. Cumulative benefits across subgroups favour CBT, with a number needed to treat ranging from 5.3 to 8.73. Unfortunately, the implementation into widespread daily practice is extremely slow. The main reason for this is a lack of interventionalists in many countries and regions4. This could be overcome by all specialists with expertise in catheter interventions: interventional neurologists, neuroradiologists, vascular neurosurgeons, and interventional cardiologists5, joining forces. Although thrombectomy is already widely available in several European countries, this is still not the case in most countries. An ominous message for the professional community is the fact that the European Stroke Organization (ESO) has published separate guidelines for thrombectomy6 and thrombolysis7. These two sets of guidelines should be merged into one document, with a clear statement that thrombectomy (±thrombolysis) is the preferred treatment option, while thrombolysis alone should only be used in remote regions, or places without neurointerventional services. Acute myocardial infarction guidelines changed similarly 19 years ago, putting primary angioplasty as the gold standard, and leaving thrombolysis as a second option only for remote regions. Modern neurospecialists understand and support this development, however there is still a lot of resistance among many conservative neurologists.
Neurologists (or strokologists in some countries) should remain the key and leading specialists for stroke patients. Their role in early diagnosis, CBT indication, and post-intervention treatment in stroke units (including careful individual decisions about pharmacotherapy and rehabilitation) is essential, and with the increased use of CBT will be even more important.
The ideal future scenario should be as follows: 1) a prehospital diagnosis of acute stroke, including direct contact between emergency services staff and a neurospecialist, and a joint decision about the transport destination; 2) patients with suspected large vessel occlusion stroke should be transferred directly to tertiary (comprehensive, CBT-capable) stroke centres, bypassing the nearest non-CBT hospitals; 3) the neurointerventional team should be alerted during the transport; 4) the angiography suite and computed tomography (CT) suite should be next door to each other, or the angiography suite should be equipped with a rotational flat-panel CT option589. The in-hospital door-to-groin puncture time should be kept below 30 minutes for all patients, with an ideal goal of 15 minutes. With such fast-track treatment, many patients can be saved from death or severe disability.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.