Abstract
Background: Retrievable stents and aspiration catheters have been developed to provide more effective arterial recanalisation in acute ischaemic stroke.
Aims: The aim of this analysis was to test the effect of mechanical thrombectomy on mortality and long-term neurological outcome in patients presenting with acute large-vessel anterior circulation ischaemic stroke.
Methods: A structured search identified randomised controlled trials of thrombectomy (using a retrievable stent or aspiration catheter) versus control on a background of medical therapy which included intravenous thrombolysis if appropriate. The primary endpoint was disability at 90-day follow-up as assessed by the modified Rankin scale (mRS). Secondary endpoints included all-cause mortality and symptomatic intracranial haemorrhage. A Bayesian mixed-effects model was used for analysis.
Results: Twelve trials met the inclusion criteria, comprising a total of 1,276 patients randomised to thrombectomy and 1,282 patients to control. Randomisation to thrombectomy significantly reduced disability at 90 days (odds ratio [OR] 0.52, 95% credible interval [CrI] 0.46 to 0.61, probability(control better)<0.0001). Furthermore, thrombectomy reduced the odds of functional dependence at 90 days, indicated by an mRS score >2 (OR 0.44, CrI 0.37 to 0.52, p<0.0001). Thrombectomy reduced all-cause mortality at 90 days (16.1% vs 19.2%, OR 0.81, 95% CrI 0.66 to 0.99, p=0.024). The frequency of symptomatic intracranial haemorrhage was similar between thrombectomy (4.2%) and control (4.0%) (OR 1.12, 95% CrI 0.76 to 1.68, p=0.72).
Conclusions: In patients with an acute anterior circulation stroke, modern device thrombectomy significantly reduces death and subsequent disability. The magnitude of these effects suggests that universal access to this treatment strategy should be the standard of care.
Introduction
The holy grail of treatment in acute ischaemic stroke caused by large vessel occlusion is prompt removal of the thrombus obstructing the cerebral artery to minimise permanent brain injury. This has become possible with the development of cerebral artery aspiration catheters and retrievable stents.
Acute ischaemic stroke accounts for 2.7 million deaths annually and is the leading cause of severe long-term disability in adults worldwide1. Administration of intravenous tissue plasminogen activator (IV-tPA) within 4.5 hours of symptom onset reduces subsequent disability, is first-line medical therapy, and is an established treatment target for healthcare systems globally2. However, IV-tPA does not achieve recanalisation in the majority of cases: success varies according to the length and composition of the occlusion, and long-term disability remains common3.
In stroke caused by large vessel occlusion, higher rates of revascularisation have been reported when mechanical thrombectomy is used in addition to thrombolysis4. The advantage arises because mechanical extraction is more effective at removing established thrombus which is resistant to enzymatic destruction through fibrinolysis. The addition of thrombectomy may therefore allow treatment to be effective over a broader time window from symptom onset, thereby providing effective therapy to patients who may otherwise achieve a poor result, or even be contraindicated, from thrombolytics.
Aspiration catheter techniques for acute ischaemic stroke apply negative pressure to suction the thrombus through or into a dedicated neurothrombectomy catheter. Retrievable stents consist of a self-expanding mesh which is deployed alongside the thrombus, ensnaring the clot within its struts, which is then retrieved into the catheter. Both techniques may be used with or without thrombolysis, and crossover between these technologies is common in clinical practice.
In 2016, the HERMES collaboration published a pooled patient-level analysis of the first five randomised controlled trials (RCTs) of thrombectomy using second-generation devices5. This confirmed that thrombectomy reduced disability at 90-day follow-up, albeit in a narrow patient population. We have conducted an updated meta-analysis which permits consolidation of subsequent RCTs which have covered a range of devices6, applied increasingly pragmatic protocols suitable for real-world service conditions78, and also provided focus on patients presenting late (up to 24 hours) after stroke onset910. By synthesising these data, we have been able to calculate a contemporary, real-world, estimate of the effect size of thrombectomy for stroke, and test whether any benefits extend to a reduction in all-cause mortality.
Methods
SEARCH STRATEGY
We performed a structured search of PubMed to identify all RCTs in any language which assigned patients to thrombectomy or control for the treatment of acute anterior circulation stroke, on a background of medical therapy, which could include intravenous thrombolysis. We searched for trials between January 2010 and July 2020. The search string is available in Supplementary Appendix 1.
The search was conducted independently by two investigators (C.A. Rajkumar and S. Ganesananthan) and the senior investigator (M. Shun-Shin) arbitrated any discrepancies.
INCLUSION AND EXCLUSION CRITERIA
We included any RCT which examined the effect of thrombectomy in addition to best medical therapy. This included the use of intravenous thrombolysis if appropriate. The use of any second-generation neurothrombectomy device (retrievable stent or aspiration catheter) was permitted. We excluded trials in which only a minority (<50%) of the thrombectomy group received thrombectomy with retrievable stents, aspiration catheters or a combination of the two (for example, trials which permitted wire manipulation in isolation as the thrombectomy technique).
ENDPOINTS
The primary efficacy endpoint for this meta-analysis was disability as assessed by the 90-day modified Rankin scale (mRS). The mRS is a validated 7-point scale of disability and dependence in activities of daily living for patients following stroke11. Higher grades indicate greater degrees of disability, where a score of 0 is equivalent to no symptoms at all, and 6 is equivalent to death. We additionally reported a dichotomised outcome from the mRS, which categorised an independent functional outcome (mRS ≤2) or a dependent outcome (mRS >2). The secondary efficacy endpoint was all-cause mortality at 90-day follow-up. The primary safety endpoint was the occurrence of symptomatic intracranial haemorrhage.
DATA ABSTRACTION AND ANALYSIS
Two authors (C.A. Rajkumar and S. Ganesananthan) independently abstracted the data from eligible studies and these data were verified by the senior author (M. Shun-Shin). For each trial, the number of patients in each mRS category at 90-day follow-up was abstracted from the intervention and control arms using the reported intention-to-treat analysis. This allowed us to construct, for each trial, a table with individual patient mRS scores that could be used to recreate the original analysis, rather than relying on a single summary effect size (such as a single odds ratio [OR] or mean difference) for each trial. We did not have access to the patient baseline covariates (e.g., time to reperfusion) that would allow the assessment of the impact of these on the effect size.
For the mRS endpoint, a Bayesian ordinal regression model was constructed for the individual patient’s mRS score. For the death and symptomatic intracranial haemorrhage endpoints, a Bayesian logistic regression model was constructed. Bayesian methods have multiple advantages over frequentist approaches. In addition to allowing external information or beliefs to be captured and made clear using prior distributions, they also allow direct probability statements to be made about parameters or their combinations12.
All models included a randomisation arm as a fixed effect and the trial as a random intercept, without random slope. The model family was binomial with the logit link function – four chains with 5,000 burn-in iterations and 5,000 post burn-in iterations. Effect sizes, 95% credible intervals, and probabilities that the effect was greater than 0 were calculated. Package default priors (normal distributions with a standard deviation of 100 on coefficients, and exponential distribution with a mean of 1 on the random effects) were used. For familiarity we present the probability that the control arm had a better outcome than the intervention. Forest plots were generated for the individual trials and summary effect.
For reader familiarity, we present an I2 equivalent statistic as a measure of heterogeneity. This was calculated from the effect sizes and standard errors from a Bayesian ordinal analysis of the individual trials and our model effect size.
Whilst the “number needed to treat” (NNT) has statistical and conceptual limitations13, we present the NNT for disability and mortality as the inverse of the absolute rate reduction of the raw data to allow comparison with other reports.
A sensitivity analysis was generated to assess the impact of the prior on the primary endpoint (Supplementary Table 1, Supplementary Table 2) and the secondary endpoint of all-cause mortality (Supplementary Table 3, Supplementary Table 4).
Publication bias for the primary endpoint was assessed with the construction of a funnel plot and asymmetry was assessed with Egger’s test14.
All analysis was performed on the statistical programming environment R15 using the “rms” package (with the “blrm” function) for modelling and the “tidyverse” set of packages.
Individual RCTs were critically appraised using the Cochrane risk of bias tool16 by two authors (C.A. Rajkumar and S. Ganesananthan), and results are reported in line with PRISMA guidance17.
Results
SEARCH RESULTS
The results of the search strategy are shown in Figure 1.
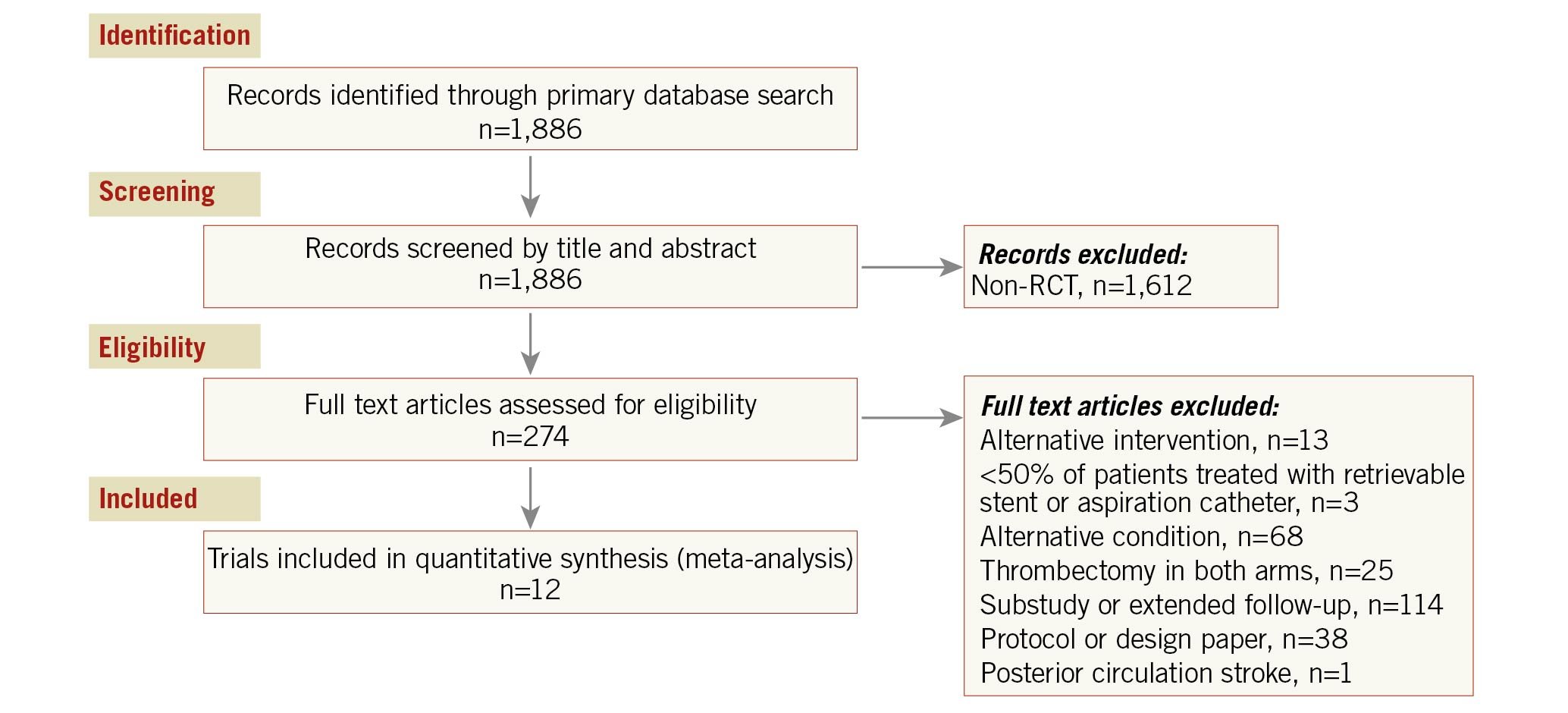
Figure 1. Consort diagram of search strategy. RCT: randomised controlled trial
Characteristics of eligible studies are summarised in Table 1.
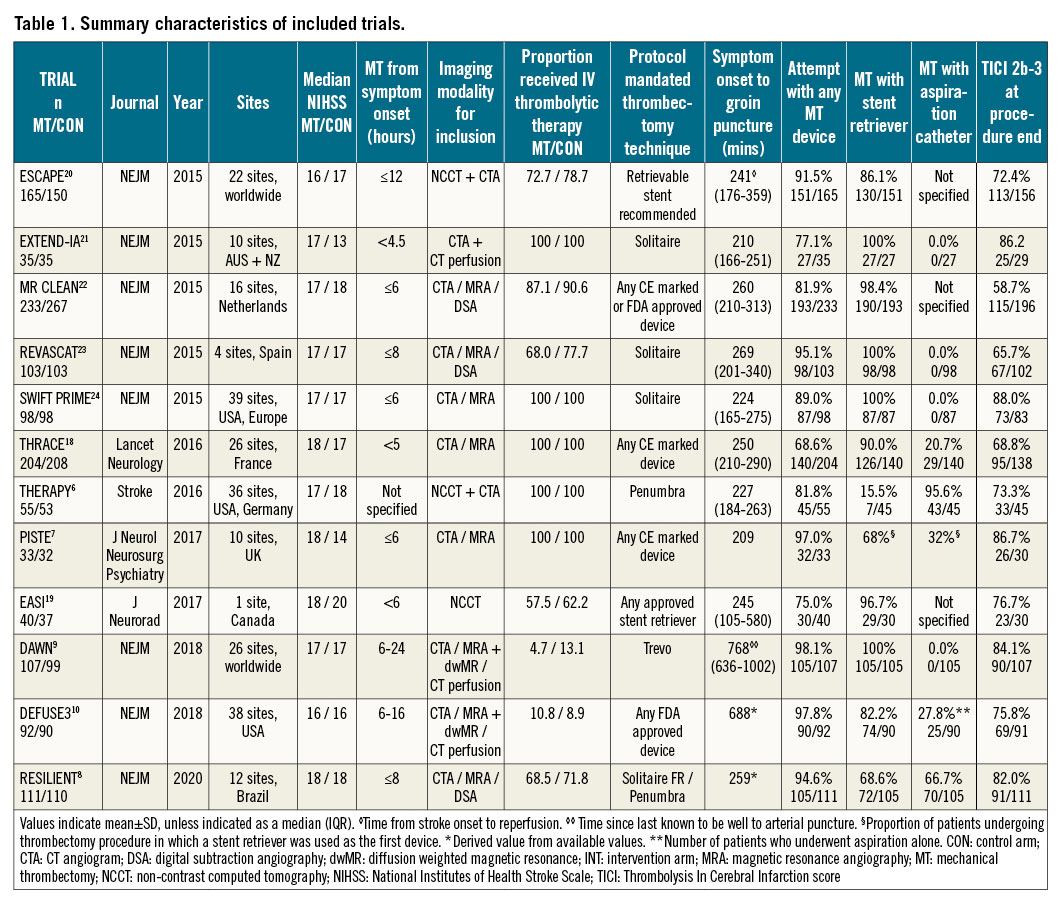
Twelve trials67891018192021222324 were eligible, comprising 2,558 patients. A total of 1,276 patients were randomised to thrombectomy and 1,282 to control. Patients in both the thrombectomy and control arms were also allowed to receive thrombolysis if indicated. The majority of trials aimed to recruit patients with a time from symptom onset to delivery of thrombectomy of less than eight hours. Two trials recruited patients with delayed presentation (up to 1610 and 249 hours) from the time they were last known to be well; the majority of these patients were ineligible for IV thrombolysis. Excluding these trials, the median duration from symptom onset to groin puncture was 245 (224-259) minutes.
Median National Institutes of Health Stroke Scale (NIHSS) scores ranged from 16 to 18 in the thrombectomy arm and 14 to 20 in the control arm. The number of patients randomised to thrombectomy who received an attempt at thrombectomy with a dedicated device was 86.4% (1,103/1,276), in whom a retrievable stent (alone or in combination with another device) was used in 87.7% (967/1,103).
Three trials did not meet eligibility criteria for our main analysis, MR-RESCUE25, IMS III26 and SYNTHESIS Expansion27. In each case only a minority of patients were treated with a retrievable stent or aspiration catheter. We additionally performed a sensitivity analysis of the totality of the available data, in which these three trials were added (Supplementary Appendix 2).
RISK OF BIAS OF INCLUDED STUDIES
In all trials, patients were aware of treatment allocation. Two trials, THRACE18 and EASI19, did not blind the outcome assessor to treatment allocation. No other significant issues were identified. The risks of bias of the included studies are summarised in Supplementary Table 5.
PRIMARY EFFICACY ENDPOINT: MODIFIED RANKIN SCALE AT 90 DAYS
The distribution of mRS scores at 90-day follow-up is displayed in Figure 2. Thrombectomy reduced the level of disability at 90 days compared with medical therapy alone (OR 0.52, 95% credible interval [CrI] 0.46 to 0.61, p<0.0001, I2=48%) (Figure 3A). The median mRS at follow-up was 3 in the thrombectomy group and 4 in the control group (mean 2.8 vs 3.5).
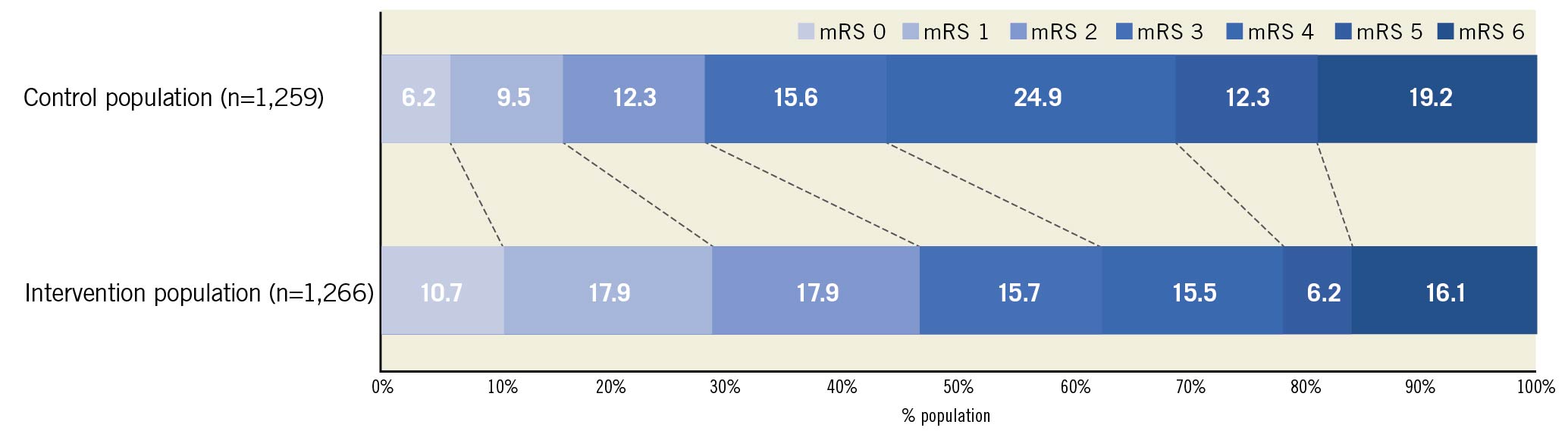
Figure 2. Distribution of modified Rankin Scale scores at 90-day follow-up. Higher scores indicate greater disability. mRS: modified Rankin Scale
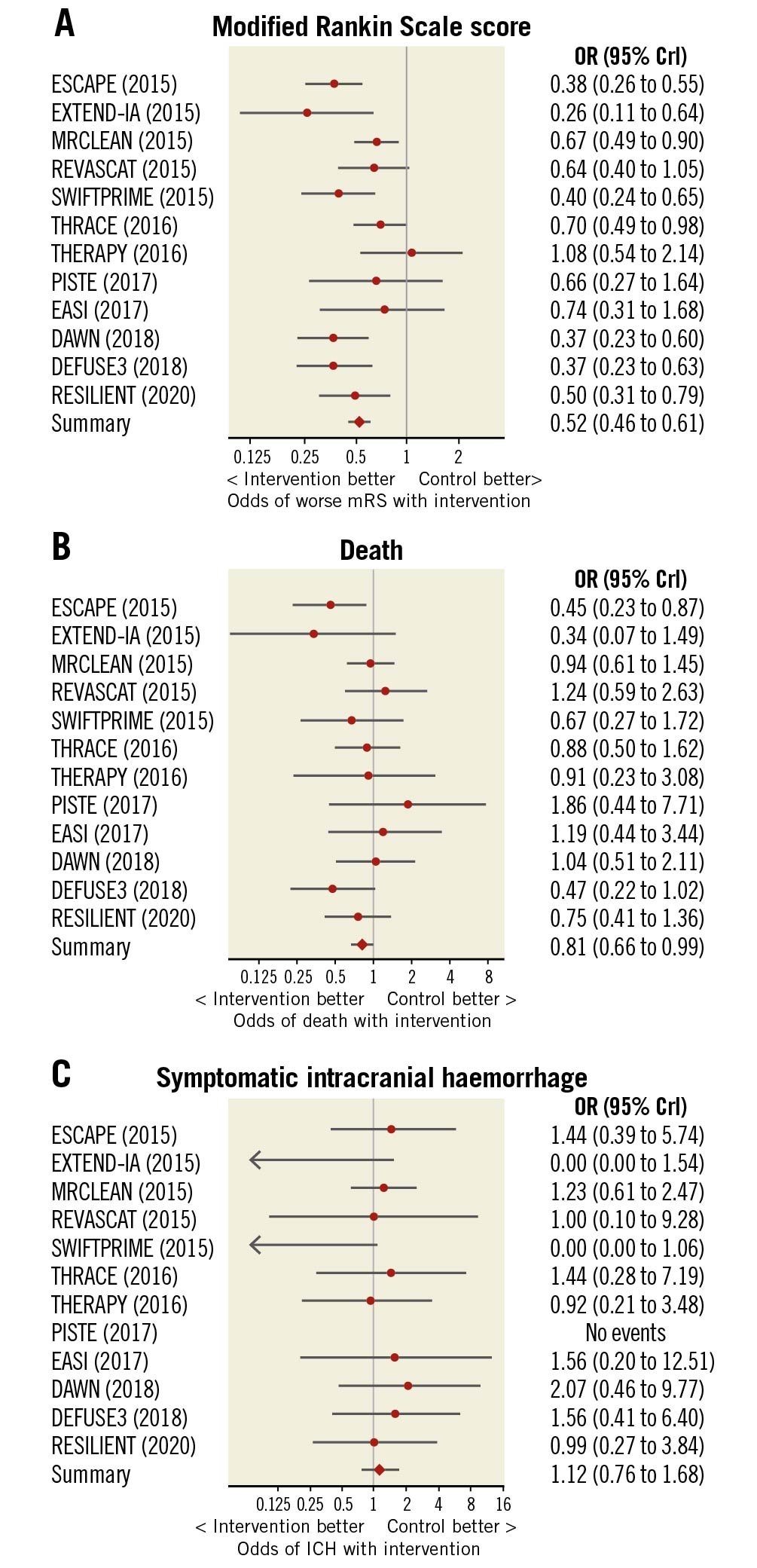
Figure 3. Forest plots of outcome measures. Forest plots indicating the effect of mechanical thrombectomy versus control for the treatment of acute ischaemic stroke on 90-day outcomes of (A) modified Rankin Scale score, (B) all-cause mortality, and (C) symptomatic intracranial haemorrhage. CrI: credible interval; ICH: intracranial haemorrhage; mRS: modified Rankin Scale score; OR: odds ratio
Thrombectomy reduced the odds of patients being functionally dependent (mRS >2) at 90 days (OR 0.44, CrI 0.37 to 0.52, p<0.0001). For every 5.4 patients treated with thrombectomy, one fewer patient will be dependent at 90 days (Central illustration).
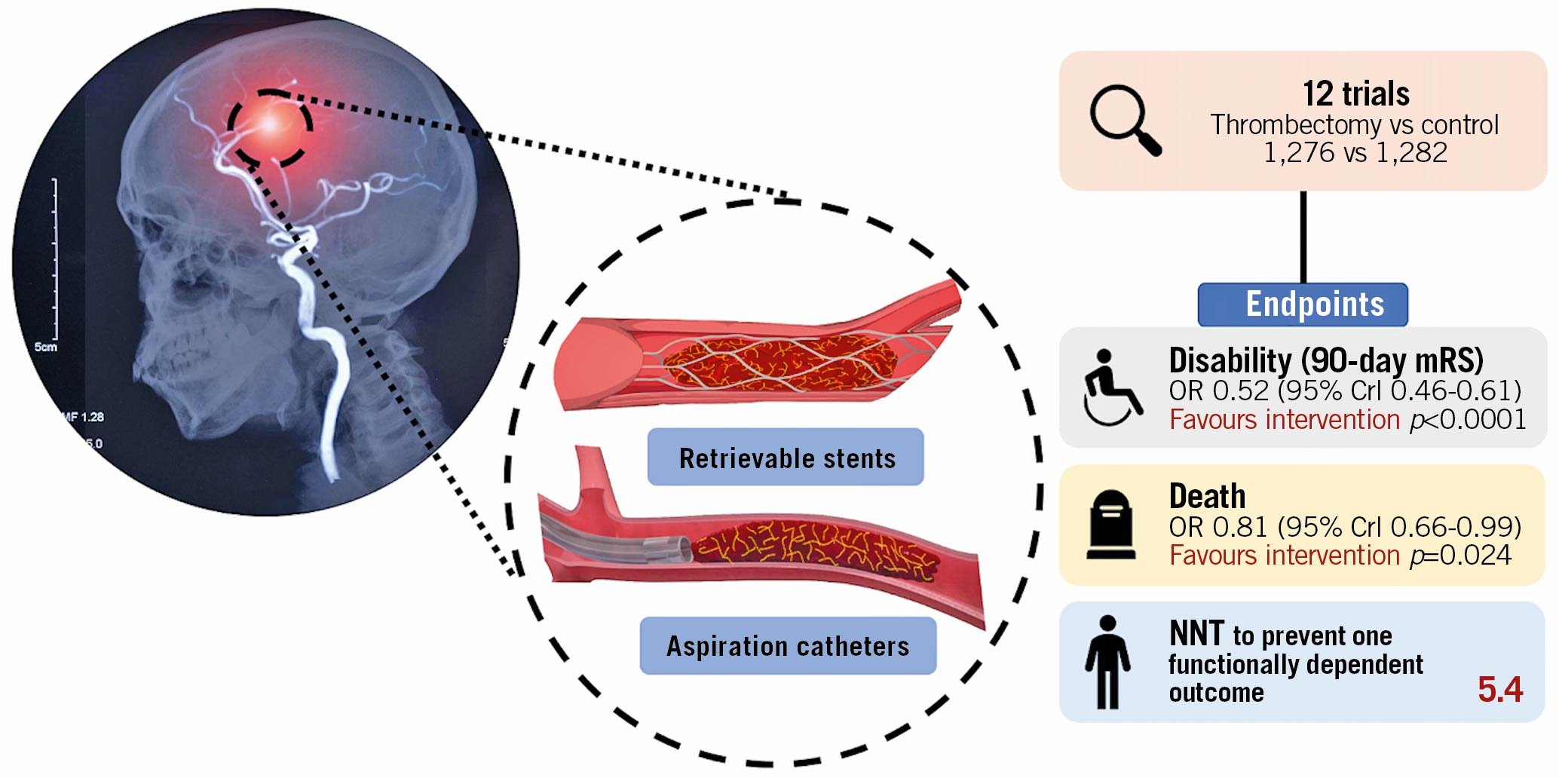
Central illustration. Mechanical thrombectomy with retrievable stents and aspiration catheters for acute ischaemic stroke: a meta-analysis of randomised controlled trials. Crl: credible interval; mRS: modified Rankin scale; NNT: number needed to treat
SECONDARY EFFICACY ENDPOINT: ALL-CAUSE MORTALITY
At 90 days, death occurred in 16.1% (204/1,266) of patients randomised to thrombectomy and 19.2% (242/1,259) randomised to control. Thrombectomy reduced all-cause mortality (OR 0.81, 95% CrI 0.66 to 0.99, p=0.024, I2=0%) (Figure 3B). The NNT to prevent one death at 90 days was 32.
PRIMARY SAFETY ENDPOINT: SYMPTOMATIC INTRACRANIAL HAEMORRHAGE
Symptomatic intracranial haemorrhage occurred in a small proportion of patients randomised to thrombectomy (4.2%, 54/1,276) and control (4.0%, 51/1,282). The odds of symptomatic intracranial haemorrhage were similar between the arms (OR 1.12, 95% CrI 0.76 to 1.68, p=0.72, I2=0%) (Figure 3C); however, the small number of events limits certainty.
PUBLICATION BIAS
There was no strong evidence of publication bias in the trials included in this meta-analysis (funnel plot, Supplementary Figure 1, Egger’s test p=0.2).
SENSITIVITY ANALYSIS
Our sensitivity analysis extended the scope of eligible trials to those that did not routinely use retrievable stents or aspiration devices (Supplementary Table 6) but instead used wire manipulation, first-generation devices (such as the Merci retriever) or even attempted intra-arterial catheter-directed ultrasound. The results of this analysis are reported in Supplementary Figure 2.
SAMPLE DIAGNOSTIC PLOTS
Sample diagnostic plots (trace, density and autocorrelation) for each endpoint are shown in Supplementary Figure 3-Supplementary Figure 5.
Discussion
The RCTs of modern thrombectomy for acute ischaemic stroke (covering a diverse range of trial protocols, encompassing delays to treatment onset, differential use of thrombolytics, a variety of second-generation devices, and pragmatic treatment settings) show that thrombectomy (i) significantly reduces disability at 90-day follow-up, (ii) significantly reduces all-cause mortality at 90 days, and (iii) is not associated with an increase in the rate of symptomatic intracranial haemorrhage, although the small number of events limits certainty.
DISABILITY REDUCTION WITH THROMBECTOMY
A 1-grade better outcome in those randomised to thrombectomy is a substantial reduction in disability. It is the difference between being bedridden and not (mRS 5 vs 4). Alternatively, it is the difference between only being able to walk when someone is available to help and being able to walk whenever one wants to (mRS 4 vs 3).
The strength of our analysis is that it was sensitive across the full 7-point mRS scale, rather than draining statistical power by dichotomising at a particular threshold. However, some dichotomies are clinically important. For example, by dichotomising the results into independent (mRS ≤2) and dependent (mRS >2) categorisations, we can calculate that, for every 5.4 patients treated with the addition of thrombectomy to medical care, one fewer patient is dependent at 90 days. Put into context, the equivalent figure for functional independence with the addition of thrombolysis to medical therapy for stroke is 1828.
MORTALITY REDUCTION WITH THROMBECTOMY
This is the first complete meta-analysis to demonstrate a significant reduction in all-cause mortality following mechanical thrombectomy. Thrombectomy reduced mortality from 19.2% to 16.1%. The NNT to prevent one death at 90 days was 32. Not only has mortality reduction not been found with thrombolysis for stroke28, but this effect size of three absolute percentage points is similar to that of primary percutaneous coronary intervention (PCI) for ST-elevation myocardial infarction (STEMI) (which has been estimated at 2%)29.
IMPLICATIONS FOR SERVICE PROVISION
Timely intervention, to obtain the best clinical outcome, requires services that are available locally in many hospitals around a given country rather than isolated in small numbers of super-specialised centres to which the patient has to be transported. The lesson from primary PCI is that it was feasible and effective to have dozens of hospitals providing 24/7 emergency intervention, to which patients presenting anywhere in the country could be transported within tens of minutes.
In acute ischaemic stroke, as in acute myocardial infarction, early intervention is beneficial. Each 15-minute reduction in the time from stroke onset to tPA is associated with a 4% increase in the odds of walking independently at discharge30. Despite this, it is notable that the selected populations enrolled in the delayed presentation DEFUSE 310 and DAWN9 trials did not have the smallest effect sizes of trials of thrombectomy in this meta-analysis. Similarly, the EXTEND31 trial for thrombolysis for stroke found benefit up to nine hours. Whilst it must be stressed that the delayed presentation trials randomised a highly selected patient cohort in comparison to trials restricted to a six-hour time window, the RCT evidence for thrombectomy for stroke for delayed presentation exceeds that for primary PCI for STEMI910.
Services implemented for acute ischaemic stroke have mirrored those for acute myocardial infarction. First, there is thrombolysis made available locally. Then comes procedural intervention offered only in a small number of super-specialised centres. Finally, with recognition of mortality benefit, the health service moves to ensure universal access to prompt procedural intervention3233.
For stroke intervention, the sites providing it need interdisciplinary teams with complementary expertise. Routine, 24/7 access to CT imaging, high dependency care and rehabilitation services are required. They also need 24/7 teams of proceduralists, catheter laboratory staff, and anaesthetists on-call for this intervention. Minimum practice standards for acute stroke care have been defined previously34. It is recommended that mechanical thrombectomy is available in all level 1 and level 2 stroke centres. However, routine access to thrombectomy remains limited in most European countries35.
No more RCTs are required on the general question of whether modern thrombectomy for acute ischaemic stroke is better than medical therapy alone for large artery acute ischaemic stroke. Although questions remain over the risk-benefit ratio of mechanical thrombectomy in certain subgroups, such as occlusions of the M2 segment of the middle cerebral artery, the overall benefit is seen across numerous trials with increasingly pragmatic protocols, performed in increasingly diverse healthcare systems. We can therefore be confident that the benefits of thrombectomy are both large and generalisable.
A mechanical thrombectomy service is a multidisciplinary effort. The next step for the healthcare system is rapid expansion of the pool of specialists able to perform the technique and an increase in the provision of 24/7 CT vascular imaging and interpretation, and advanced stroke care. For the provision of imaging, cost efficiency may be improved through artificial intelligence to screen large numbers of images for eligibility36.
Limitations
This meta-analysis addressed retrievable stent and aspiration catheter therapies. There have been previous technologies. The Merci device from 2004 used a retrievable coil, rather than a stent. It achieved Thrombolysis In Cerebral Infarction (TICI) 2b-3 recanalisation in only 25% of cases in the MRRESCUE trial25. There have been other trials in which the only mechanical intervention in most patients in the active arm was simple disruption of the thrombus with a guidewire. These trials also generally had lower standards of prior imaging confirmation of vascular occlusion amenable to thrombectomy. Those trials were not eligible for our analysis252627. However, we have performed a sensitivity analysis in which they are added and found that the primary endpoint continues to show significant benefit of the intervention.
Furthermore, among the trials that did meet our inclusion criteria, there was substantial between-trial and within-trial heterogeneity in the specific devices used for thrombectomy. However, direct head-to-head RCTs comparing a strategy of direct aspiration versus retrievable stents as the first-line technique have been performed, with little evidence of difference between the two3738.
There was significant variation in the inclusion criteria between trials. For example, the DAWN9 and DEFUSE 310 trials are distinct in design by their inclusion of patients presenting late after stroke onset. This is an important source of heterogeneity. However, whilst an attenuated benefit of thrombectomy might have been predicted in this setting, the effect sizes observed in these “late-presenter” trials were entirely consistent with trials restricted to patients with earlier presentation. The consistent effect seen across patient populations therefore gives confidence that the findings are generalisable. The HERMES collaboration have previously published predictors of response to thrombectomy based on individual patient data from a more limited number of trials3940. Access to equivalent covariate data would be required for similar analyses to be performed for the expanded RCT data presented here.
Trials included in this meta-analysis typically recruited patients in centres with experienced interventional neuroradiologists in North America, Western Europe and Australasia. It could be argued that comparable results may not be achieved in less specialist centres. However, on account of the infancy of this therapy, the majority of operators in these trials would not have vast experience in thrombectomy. Furthermore, the purpose of the PISTE7 and RESILIENT8 trials was to assess whether the benefits of thrombectomy were reproducible in more pragmatic settings and public health systems. Reassuringly, they were found to be so.
Our conclusions are limited to patients presenting with acute large-vessel anterior circulation strokes as this is what was studied in the included trials. Vertebrobasilar occlusions are typically associated with more devastating neurological consequences, and intravenous therapy is limited by the fact that many patients present late with ill-defined symptoms or are delayed by diagnostic uncertainty41. Randomised trials of thrombectomy for vertebrobasilar occlusions have therefore been hampered by poor recruitment rates, and a high frequency of crossover from control to thrombectomy arms has been observed42. In addition, limited evidence suggests that mechanical thrombectomy in the posterior circulation may be more prone to complications than in the anterior circulation43.
Our primary endpoint, disability as assessed by the mRS, is subject to a number of limitations. First, there is substantial interobserver variability in scores awarded using the mRS, even by experienced researchers44. Second, its reporting is subject to bias in the absence of assessor blinding. Two trials1819 included in this meta-analysis did not blind the assessor to treatment allocation; their results are therefore subject to this potential limitation.
Recruitment was halted prior to the planned randomisation target in 10/12 trials included in this meta-analysis. For seven trials671920212324 this was because of evidence of efficacy from an external trial. Three trials were halted due to achievement of an internal efficacy margin on a pre-specified interim review8910. A different result may have been obtained if these trials had run to completion.
Conclusions
Mechanical thrombectomy with retrievable stents and aspiration catheters significantly reduces disability at 90 days in anterior circulation ischaemic stroke. The available evidence now demonstrates that these benefits extend to a reduction in all-cause mortality. There is no significant increase in symptomatic intracranial haemorrhage. The absolute mortality effect is similar to primary PCI which has long been rolled out universally. Innovative action by healthcare policy makers could transform the disability and mortality outcomes for patients with acute ischaemic stroke, with limited ongoing cost if efficiently integrated with existing services.
Impact on daily practice
Contemporary trials of mechanical thrombectomy confirm a reduction in disability with a large effect size. For every 5.4 patients treated, one fewer patient is functionally dependent at 90 days. The available evidence now supports a significant reduction in all-cause mortality, a 3% absolute risk reduction at 90-day follow-up. The benefits of mechanical thrombectomy for acute ischaemic stroke are both large and generalisable. Urgent action is required to expand access to this life-saving therapy.
Funding
C. Rajkumar is a PhD Training Fellow at the Medical Research Council [Grant Number MR/S021108/1]. M. Foley is a PhD Training Fellow at the Medical Research Council [Grant Number MR/V001620/1]. J.P. Howard is a PhD Training Fellow at the Wellcome Trust [Grant number 212183/Z/18/Z]. A. Nowbar is supported by the NIHR Imperial Biomedical Research Centre (BRC).
Conflict of interest statement
I. Grunwald is a co-founder and a shareholder of Brainomix. R. Al-Lamee reports speakers’ honoraria from Philips Volcano and Menarini Pharmaceuticals. H. Seligman declares research funding from Amgen. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.