Abstract
Aims: We report our single-centre experience with the Solitaire AB self-expanding retrievable stent system in patients with acute ischaemic stroke.
Methods and results: Demographic, clinical, and angiographic findings of thirty-eight consecutive patients with acute ischaemic stroke who underwent mechanical thrombectomy were evaluated retrospectively. The mean initial National Institutes of Health Stroke Scale (NIHSS) score was 17.8±4.6. Nearly half of the patients had a middle cerebral artery (MCA) occlusion (45%). Both internal carotid artery and MCA occlusions were detected in five patients. Successful revascularisation (Thrombolysis in Cerebral Infarction [TICI] 2b and 3) was achieved in 34 of 38 (89%) patients; a TICI 3 state was observed in 24 (63%) patients. Almost three quarters of the patients (74.3%) improved by >5 points on the NIHSS at discharge, and 57.9% showed a modified Rankin Scale (mRS) score of ≤2 at 90 days.
Conclusions: This single-centre experience with mechanical thrombectomy devices demonstrated that the procedure could be performed safely with high success rates by experienced interventional cardiologists in suitably equipped cathlabs.
Introduction
Stroke is the third most common cause of death and the leading cause of severe disability worldwide1,2. Of all strokes, 85% are ischaemic and intracranial artery occlusion accounts for 80% of these ischaemic strokes3. Current treatment options for acute ischaemic stroke include intravenous (IV) fibrinolytic therapy and endovascular management with intra-arterial (IA) fibrinolytics or mechanical thrombectomy using aspiration devices and retrievable stents. Although IV fibrinolysis is the preferred treatment strategy in daily practice, the narrow therapeutic time window (<4.5 hours), numerous absolute contraindications, and relatively low efficacy have restricted its use. Results of previous studies suggested that the revascularisation rate of IV tissue plasminogen activator (tPA) ranges from 35 to 52%, depending on the degree and location of the culprit arterial occlusion; however, it could be associated with a reocclusion rate of up to 17%4-7. Although IA administration of thrombolytics provides relatively higher recanalisation rates and extension of the therapeutic window up to six hours compared to IV use but poor recanalisation rates particularly in proximal large vessel occlusion with high thrombus burden, such as the internal carotid artery (ICA) or middle cerebral artery (MCA) Ml segment, the expected benefits have not been achieved8,9.
Endovascular therapy for acute ischaemic stroke was a new modality aiming at resolution of clots in occluded cerebral arteries. This therapy includes lasers, ultrasonography, microcatheter or microwire clot maceration, aspiration or suction devices, and clot-retrieval or microsnare devices10,11. Several randomised controlled trials of mechanical thrombectomy for acute ischaemic stroke have been conducted and have shown promising results. These trials led to the Food and Drug Administration (FDA) approval of the first thrombectomy device, the Merci® Retriever (Concentric Medical, Mountain View, CA, USA), in 2004 and the second device, the Penumbra (Penumbra, Inc., Alameda, CA, USA), in 2008. These improvements in endovascular technology have led to a move towards acute stroke intervention. Compared to fibrinolytics, retrievable stent thrombectomy devices have widened the therapeutic window to eight hours with high recanalisation rates (80-90%)12,13.
Further refinement in mechanical thrombectomy became possible with the development of the Solitaire Flow Restoration (FR) device (ev3/Covidien, Irvine, CA, USA). It is a self-expanding, fully retrievable stent which obtained FDA approval in March 2012 based on the results of the SOLITAIRE™ FR With the Intention For Thrombectomy (SWIFT) Study. This study found higher recanalisation rates and better neurologic outcomes with the Solitaire FR device compared to the Merci device14. The aim of the present study was to test the efficacy of this device for cerebral vessel revascularisation in acute stroke in our local set-up.
Materials and methods
PATIENT ASSESSMENT AND IMAGING
A total of thirty-eight consecutive patients admitted to Bezmialem Foundation Hospital emergency department (ED) with acute ischaemic stroke between January 2012 and December 2013 were evaluated retrospectively. All the patients had a large intracranial artery occlusion and underwent mechanical thrombectomy using the Solitaire AB retrievable stent. A computed tomography (CT) brain scan was performed in order to rule out haemorrhagic stroke on admission. A magnetic resonance angiogram (MRA) or CT angiogram with diffusion-weighted imaging (DWI) was performed for assessment of occluded vessels. Patients with: 1) National Institutes of Health Stroke Scale (NIHSS) score >8, 2) Thrombolysis in Cerebral Infarction (TICI) score of 0 to 1 in an accessible vessel, 3) no detection of intracerebral haemorrhage (ICH) were included. After the interventional procedure, a CT brain scan was performed routinely in order to rule out ICH. We evaluated the patients who underwent direct catheter-based thrombectomy: none of these patients received thrombolytics mostly due to contraindications to thrombolytics. Patients with acute ischaemic stroke who underwent a rescue thrombectomy procedure due to the failure of thrombolysis and persisting large penumbra after lytics were not analysed. As a result, a subgroup analysis comparing the results of different patient subsets could not be performed.
PROCEDURE
Patients admitted to the ED with a diagnosis of acute stroke initially assessed by the stroke neurologist and eligible patients for endovascular treatment were transfered to the catheter laboratory according to our hospital’s stroke protocol (Figure 1)1. The mechanical thrombectomy procedure was performed (under slight sedation and local anaesthesia) by a stroke team composed of a cardiologist, a neurologist, and an anaesthesiologist. For evaluation of the degree of leptomeningeal collaterals, an angiogram of the non-infarct-related artery was performed first.
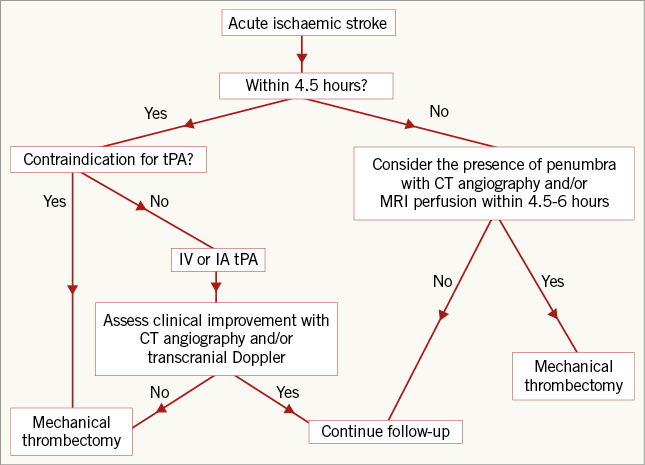
Figure 1. Treatment algorithm for the patients with acute ischaemic stroke.
The occlusion status and TICI scale of the occluded vessel were confirmed by angiography after locating the 8 Fr guiding catheter (Launcher; Medtronic Inc., Minneapolis, MN, USA) in the left internal carotid artery. To prevent the occurrence of a new thromboembolic event during the procedure, a weight-adjusted dose (40 IU/kg, max. 5,000 IU) of unfractionated heparin was administered through the guiding catheter (Table 1). In patients with tandem occlusions, a proximal protection device (MO.MA; Invatec, Roncadelle, Italy) was used. Next, a Rebar 18 microcatheter (ev3/Covidien) under the guidance of a hi-torque Whisper LS guidewire (Abbott Laboratories, Abbott Park, IL, USA) was introduced into the target vessel and located at the distal portion of the occlusion site after passing the thrombus segment. A Solitaire AB stent (ev3/Covidien) was deployed over the whole length of the thrombus. By compressing the thrombus, the retrievable stent’s radial force was able to create a channel immediately and partially restore blood flow to the distal territory. The device was left in place for five minutes to allow engagement of the thrombus within the stent struts. Partial recanalisation was observed immediately after stent deployment. The microcatheter and stent were gently pulled back under continous aspiration using a 50 cc syringe through the guiding catheter to prevent development of a new embolism by lost clots. Patency of the carotid artery was maintained with a stent after successful recanalisation of the distal occlusion in patients with tandem lesions. To assess the patency of the artery, a control angiography was performed immediately after the interventional procedure (Figure 2). When the subsequent angiogram showed a TICI score <2, the procedure was repeated until a TICI score of >2 or 3 was achieved. TICI scoring is summarised in Table 2 13. The NIHSS score was calculated for each patient on admission, after the procedure and at the time of discharge. The modified Rankin Scale (mRS) was recorded at the third month. An mRS <2 was defined as a good neurological outcome. The study was approved by the local ethics committee.
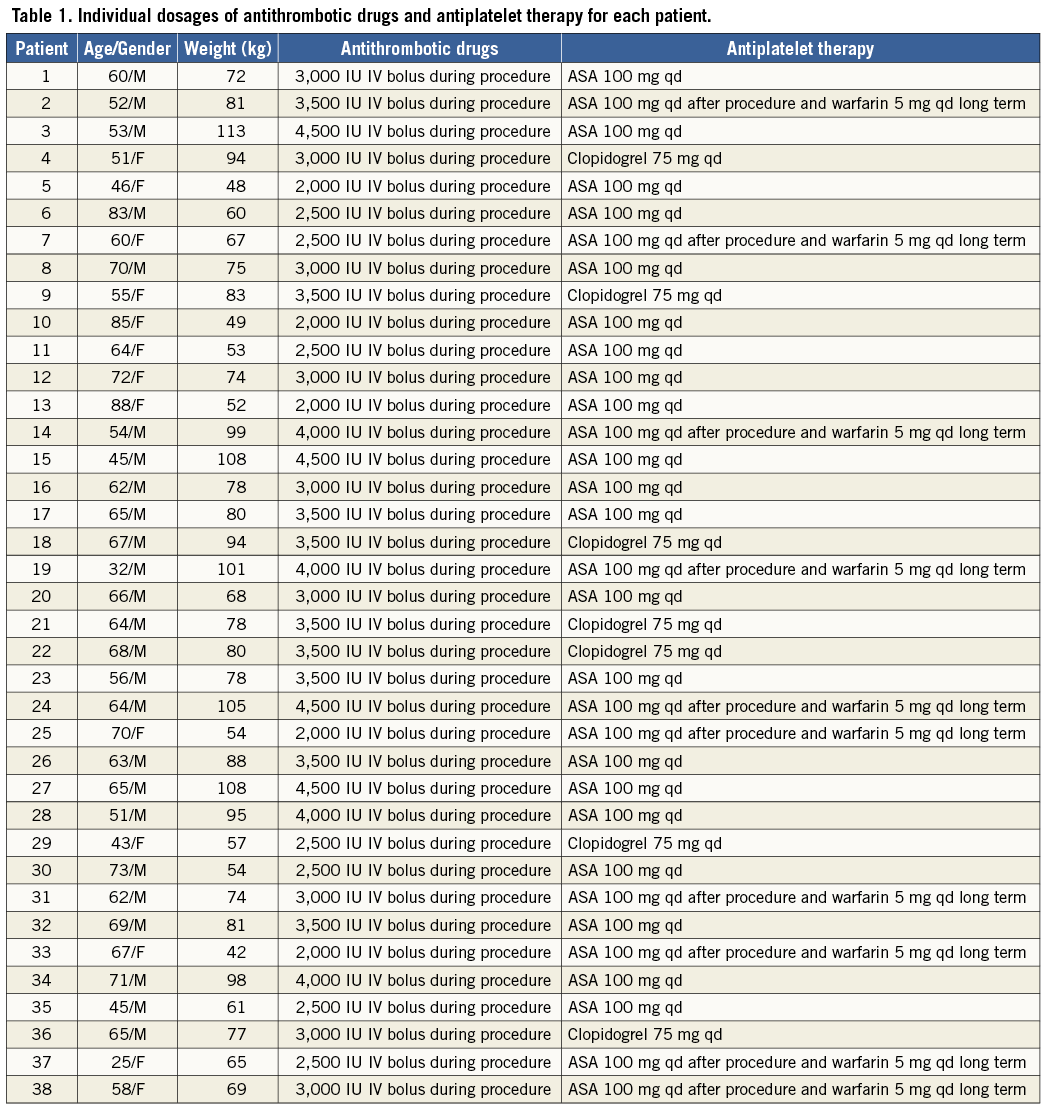

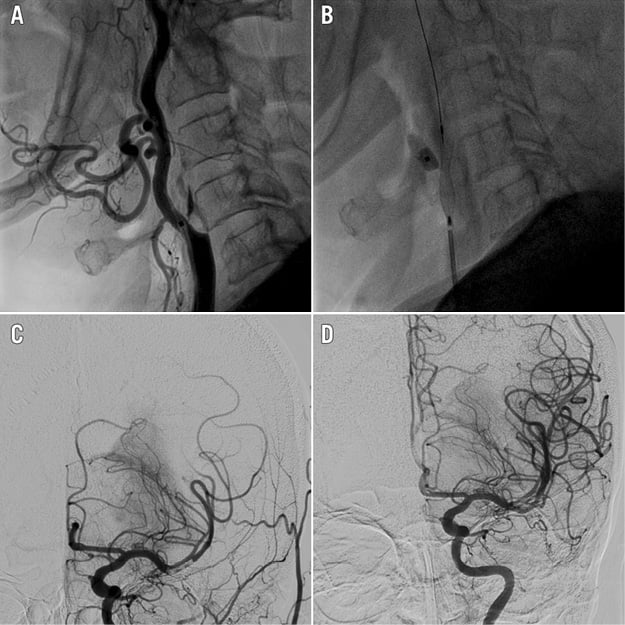
Figure 2. Initial and post-treatment angiograms. A) Initial angiogram (lateral views) demonstrating the occlusion of the internal carotid artery. B) Internal carotid artery stenting accompanied by the MO.MA protection system (Invatec). C) Immediate post-treatment angiogram showing thrombus migration to M2 segment of middle cerebral artery (MCA). D) Complete revascularisation of left MCA.
Results
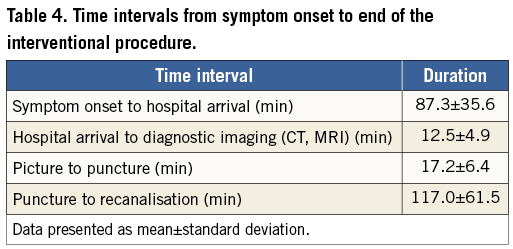
The clinical and imaging characteristics of the thirty-eight consecutive patients (mean age 60.5±13.4 years; 14 females and 25 males) are shown in Table 3. The patients were admitted to our centre between 60 minutes and 480 minutes after the onset of symptoms, with a mean time of 218 minutes. Time intervals from symptom onset to first medical contact, hospital arrival, diagnostic CT, sheath insertion and clot retrieval (thrombectomy) are shown in Table 4. Most of our patients presented with dense right hemiparesis. In addition, patients had neglect, dysphasia, and difficulty in swallowing. The presence of a thrombus was confirmed by CT angiogram in all patients. The clinical and post-procedural angiographic characteristics are shown in Table 5. Reperfusion time was defined as the time from onset of symptoms to complete recanalisation of the occluded artery and was between 160 minutes and 600 minutes, with a mean value of 246 minutes. The duration of the revascularisation procedure was between 45 minutes and 180 minutes, with a mean value of 78 minutes.
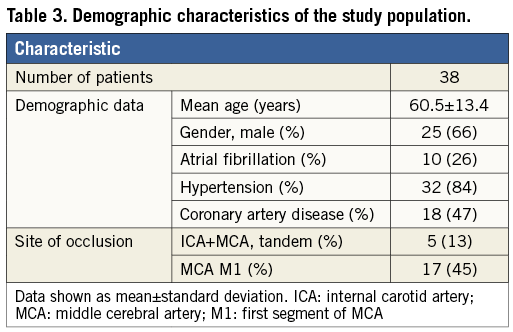
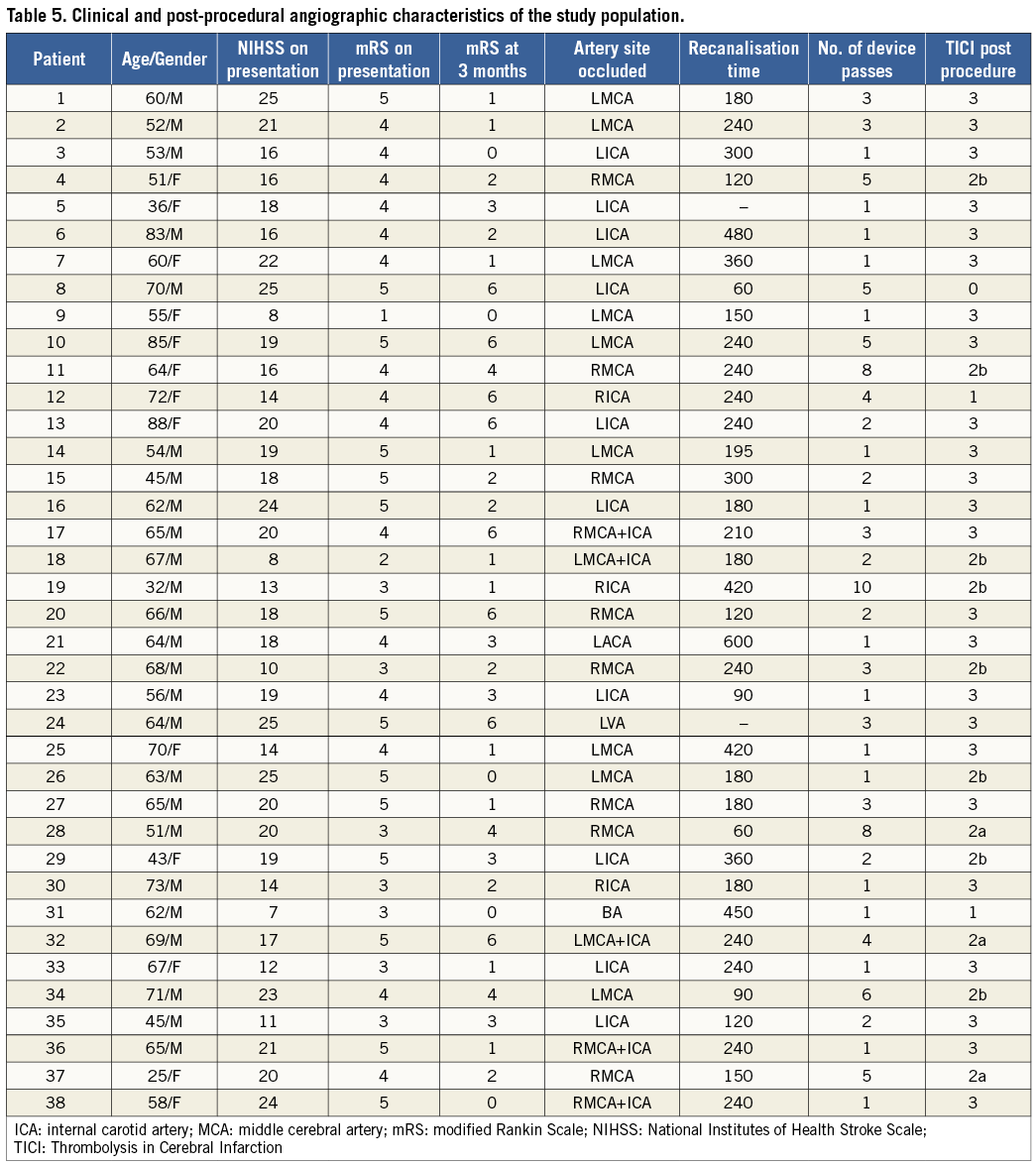
Almost half of the patients had a middle cerebral artery (MCA) occlusion (45%). Both internal carotid artery and MCA occlusions were detected in five patients. Successful revascularisation (TICI 2b and 3) was achieved in 34 of 38 (89%) patients; a TICI 3 state was observed in 24 (63%) patients. Balloon angioplasty after thrombectomy was performed in one patient with infective endocarditis who underwent cardiac open surgery for aortic valve replacement. NIHSS on admission was 17.8±4.6 and almost three quarters of the patients (74.3%) improved by >5 points on the NIHSS at discharge, and 57.9% showed an mRS of <2 at 90 days. New occlusion by migrated emboli was observed in five cases (13.2%). Two patients experienced post-procedural symptomatic intracerebral haemorrhage. Five patients died due to nosocomial infection and symptomatic post-procedural intracerebral haemorrhage in hospital, and one patient died in the second month after discharge.
Discussion
In the present single-centre study, we identified 38 patients with acute ischaemic stroke undergoing mechanical thrombectomy by interventional cardiologists with the Solitaire AB self-expanding retrievable stent. A successful recanalisation rate and good outcome were found in 89% and 57.9%, respectively. In addition, a significant proportion of patients completely recovered with a slight or no long-term disability. Also, six patients died during three months of follow-up.
Ischaemic stroke is the leading cause of acquired disability and the third most common cause of death in the world1,2. Despite the improving modalities in stroke management, there is still a challenge. In the current era, IV recombinant tissue plasminogen activator (rtPA) is the most used and standard therapy. However, its efficacy is limited in proximal intracranial arterial occlusion, and there are many absolute and relative contraindications. In the NINDS study, rtPA was administered IV within three hours of acute ischaemic stroke6. The recovery rate by three months was 40%. Another treatment modality, IA thrombolytic administration, was evaluated in the PROACT II study8. IA pro-urokinase plus heparin was compared with heparin alone during the first six hours of symptoms. Of the patients in the IA route arm, favourable outcome at three months was 40% and the recanalisation rate was 66.1%. The combined IV and IA fibrinolytic therapy was evaluated in the IMS II study15. It was shown that good outcome at three months was 46%. The recanalisation rate was 60%. As can be seen, although IA thrombolysis extends the time of administration up to six hours, the results are not rewarding. It could be used in patients with a small thrombus burden and very tortuous neck arteries.
Thrombectomy (the Merci Retriever) and thromboaspiration (the Penumbra system) devices were approved in 2004 and 2007, respectively. Then, in 2008, stent retrievers were approved. The Merci Retriever was used in the MERCI study during the eight hours following the start of symptoms16. One hundred and fifty-one patients who were not suitable for thrombolytic treatment with a high NIHSS score (median 20) were assessed. The arterial recanalisation rate was 48.2%. The Multi MERCI study evaluated 164 patients (median NIHSS of 19)17. Recanalisation was achieved in 57.3% of cases with the device alone and in 69.5% of cases with a combination of device and medical treatment (IV or IA). Good clinical outcome was seen in 36% of patients. In the Penumbra Stroke Trial (median NIHSS of 18), recanalisation was obtained in 81.6% of the cases18. A favourable outcome was seen in 25% of all the patients.
The efficacy of older devices such as Merci and Penumbra was not satisfactory, so newer-generation devices such as retrievable stents (Solitaire FR, AB) were developed. These devices are self-expanding stents fixed to the system allowing insertion of a temporary stent and removal of the clot. SWIFT (Solitaire FR), a randomised study, compared the Solitaire and Merci retrievers in 113 stroke patients within eight hours of stroke onset19. Better outcomes (58.2% versus 33%) were observed in the Solitaire group compared with the Merci group. In addition, mortality was lower (17.2% versus 38%) in the Solitaire group at three months.
Comparing the results of our study with six large trials assessing IA mechanical treatment for acute stroke, higher recanalisation rates and lower three-month mortality rates were observed in our study than in the PROACT II, MERCI, IMS II, Multi MERCI, and Penumbra Stroke Trials14-19. Mortality (17.2% versus 15.8%), recanalisation (88.9% versus 89%) and good outcome rates (58.2% versus 60%) were similar between SWIFT and our study. Good outcome rates were also similar to IMS II but better than the others. The higher success rates with new stent retrievers could be related to device design, and rapid and simple applicability. Although the studies evaluating retrievable stents have shown good angiographic and clinical results, ongoing large studies will provide conclusive data in the future. A study by Abilleira et al20 including 536 consecutive patients with acute ischaemic stroke treated with endovascular therapy demonstrated that age greater than 80 years and hypertension predicted increased risk, while anterior circulation strokes and pre-stroke mRS <2 reduced risk. Whether or not patients had prior IV tPA had no effect on functional outcome or mortality. Wisco et al selected patients for endovascular treatment based on CT/CT angiography and magnetic resonance imaging (MRI)21. The MRI approach before treatment decreased the number of endovascular stroke interventions by half. The results of these two studies highlighted the possibility that endovascular trials are contaminated by ineligible patients, and this might explain why there were very high rates of recanalisation but still only a 50%-60% rate of good outcome. So, patient selection is very important. This condition necessitates an experienced neurologist and radiologist in your stroke team. The 2013 AHA/ASA guidelines suggested that the Solitaire thrombectomy devices could be useful in achieving recanalisation alone or in combination with fibrinolytics in selected patients (Class IIa, Level of Evidence B)1.
In our hospital, we designed a stroke team including trained interventional cardiologists, neurologists and radiologists. Our catheter laboratory provides 24/7 care (24 hours per day, 7 days per week). Our results are comparable with other large trials. We hope that the present study might encourage the Ministry of Health to support this stroke management strategy in our country because cerebrovascular diseases account for 15% of all deaths in Turkey.
The lack of a control group and small sample size were the main limitations of our study. However, the use of the Solitaire AB device afforded good clinical and angiographic results.
Conclusion
Mechanical thrombectomy by trained interventional cardiologists appears to be a safe, effective and feasible technique with high recanalisation rates and favourable clinical outcomes in patients with acute ischaemic stroke.
| Impact on daily practice Mechanical thrombectomy can be performed safely and decisively by trained interventional cardiologists with suitable and effective organisation of cardiology, neurology, and radiology departments, and a catheterisation laboratory with 24/7 on-site staffing. Our results emphasise the importance of a stroke team and strict selection criteria for intervention. |
Acknowledgements
The authors would like to thank staff at the angiography unit for their kind contribution and support while conducting the study. There was no financial sponsorship, grant or funding.
Conflict of interest statement
The authors have no conflicts of interest to declare.