Stroke, a growing global healthcare burden, remains one of the leading culprits of disability and death in the Western world1. Ischaemic stroke accounts for the majority of all strokes, in which rapid restoration of blood flow to salvageable tissue at risk of infarction reduces the final area of infarct and provides better outcomes. For several years, fibrinolytic treatment with tissue plasminogen activator (tPA), within four and a half hours of the onset of symptoms, has been the primary reperfusion strategy in the treatment of acute ischaemic stroke. Nonetheless, limitations of tPA therapy, including the low rates of recanalisation in large vessel ischaemic strokes, have led to the development of endovascular approaches2,3. However, robust data to support endovascular therapy for stroke were previously lacking because of the futility in randomised trials. Despite these results, researchers have remained attentive to this approach and investigated endovascular stroke treatment in a number of trials, considering some prior limitations. Subsequently, data from MR CLEAN4, EXTEND-IA5, ESCAPE6, REVASCAT7, and SWIFT PRIME8 (and expected data from other forthcoming studies) have shown improved outcomes with endovascular therapy in patients with an acute ischaemic stroke due to an arterial occlusion of the anterior circulation. Careful selection of the candidates, identification of a major vessel occlusion prior to intervention with imaging studies and effective recanalisation (TICI 2b-3) that was achieved with stent retrievers in the majority of patients contributed to good clinical outcome in the trials. Moreover, these trials achieved highly efficient workflow metrics and a relatively short time to intervention. This is particularly important, because time plays an essential role in predicting the clinical outcome and efficacy of treatment in cerebral ischaemia, as demonstrated by the analysis of these recent trials9,10.
Overall, the results were impressive and treatment remained effective across a wide range of ages and initial stroke severity as well as for both patients eligible and ineligible for intravenous tPA11. Moreover, for every 100 patients treated, 38 would have a less disabling sequel, when compared to best medical management alone, with an extra 20 achieving functional independence with endovascular treatment11. Consequently, these compelling results led to updates of the acute stroke guidelines, strongly recommending endovascular therapy after IV tPA in the treatment of acute ischaemic stroke in well-defined settings.
The favourable outcomes attained in these trials clearly mandate the establishment and reorganisation of the management of stroke services. Initial challenges likely to be faced include ensuring a timely transfer of candidates for endovascular therapy to adequate centres. This process includes many factors: increasing public awareness, improving response times of medical services, the initiation of prehospital stroke treatment, effective triage of the patients, and, finally, establishing faster in-hospital action plans12. Another significant challenge is the dispersion of well-equipped centres, capable of performing endovascular stroke interventions.
At present, many countries, including ours (Turkey), lack a sufficient number of centres which can provide a round-the-clock service for endovascular stroke treatment. Furthermore, considering the number of patients requiring endovascular treatment, insufficient procedural volume not supporting a 24/7 available team represents a major logistical challenge, particularly in areas with scattered populations13. These challenges may limit the widespread application of such a promising therapy.
Nonetheless, cardiologists have achieved a similar organisation in the context of acute myocardial infarction (AMI) over recent decades. Moreover, due to the number of procedures they perform, they have become increasingly skilled at catheter-based interventions. This highlights the potential of incorporating present organisations and workforce, in an effort to extend the services of acute stroke management. On the other hand, there are still doubts over this approach, mainly due to the concerns about the lack of a formal training. However, as supporters of this approach, we are aware of the differences in the pathophysiology of AMI and ischaemic stroke, as well as in the course of the disease and the vasculature. Therefore, the involvement of interventional cardiologists, which is of the upmost importance, does not and should not divert training (although it can be shorter), nor replace stroke teams, as this is the best way to manage stroke patients. Indeed, a previous study by our group can serve as an example of this approach: we demonstrated the possibility of attaining similar outcomes in stroke interventions performed by cardiologists working in a stroke team, to those achieved by neurointerventional centres (Figure 1)14. These results were in accordance with the results of studies by other groups15,16.
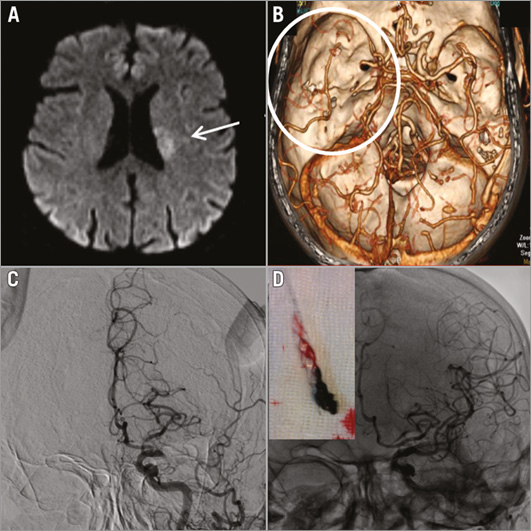
Figure 1. Case example. A 58-year-old male was admitted to hospital with right-sided weakness which had begun two hours before. Neurologic examination revealed right-sided hemiplegia, aphasia with a National Institutes of Health Stroke Scale (NIHSS) score of 20. Computed tomography with angiography showed total occlusion of the left internal carotid artery and left middle cerebral artery (A & B). This was confirmed on cerebral angiography (C). After treatment with a retrievable stent, good angiographic results were achieved (D). NIHSS score was 4 at the first hour and 2 at discharge.
In conclusion, we are clearly entering into a new era of acute ischaemic stroke treatment, as recent trials and their meta-analysis, including the one by Ferrante et al in this current issue of EuroIntervention, strengthen the role of endovascular treatments. However, there are many questions yet to be answered, including whether we will be able to translate the results of these well-organised and efficient trial settings to the real world. Nonetheless, the revolution of stroke management will require a large multidisciplinary workforce, in which we believe that the involvement of interventional cardiologists would be of benefit.
Conflict of interest statement
The authors have no conflicts of interest to declare.