Abstract
The T and small protrusion (TAP) technique is a modification of provisional T-stenting aimed at optimising “bail-out” SB stent implantation in bifurcated coronary lesions treated using the “provisional” approach. The main strengths of the TAP stenting technique are: compatibility with 6 Fr guiding catheters, full coverage of the side branch ostium, and facilitation of final kissing balloon inflation. The main drawback of TAP is related to the creation of a single layer stent strut neocarina of variable length. In this paper, we review the technical aspects which should be considered in order to achieve TAP stenting successfully in the case of “bail-out” need for side branch stenting. Furthermore, we report the technical details which may help in the practice of TAP stenting in complex bifurcated lesions with the anticipated high probability of requiring double stenting. Although no large trial has investigated this technique, the clinical results reported so far look promising.
Introduction
The single stenting technique in unselected coronary bifurcated lesions (CBL) has proven clinical efficacy. However, some patients undergoing percutaneous coronary interventions (PCIs) require the implantation of drug-eluting stents (DESs) in both the main vessel (MV) and side branch (SB). A series of techniques has been developed to implant two DES in CBL. The “T And small Protrusion” (TAP) technique is one of the more recently reported1 and has been inserted into the A family of the “MADS” (Main, Across, Distal, Side) classification for CBL stenting techniques2.
Historically, two independent groups (from Italy and the Republic of Korea) developed the TAP stenting technique in the early years of the DES era. A full description of the technique and the first clinical experience was reported at the beginning of 20071.
“Provisional” TAP technique step by step
The TAP stenting technique is a modification of the T-stenting technique aimed at optimising “bail-out” SB stent implantation in CBL treated by the “provisional” approach. Thus, according to the standard practice of TAP stenting, it is applied after the MV stent has been implanted and kissing balloon inflation has been performed. In particular, TAP stenting was developed to ensure full ostium coverage by DES struts while requiring the performance of final kissing inflation. To achieve this, the SB stent is delivered with intentional minimal protrusion inside the MV with an uninflated balloon positioned in the MV across the SB take-off (Figure 1). After SB stent deployment, kissing balloon inflation is immediately performed with the stent’s balloon and the balloon which was previously positioned in the MV (Figure 1, Moving image 1). Further kissing balloon inflations with non-compliant balloons may be advisable in the case of suboptimal stent expansion. Since most recent-generation DES and balloons fit together in large lumen 6 Fr guiding catheters, the TAP technique may be practised without large guiding catheters.
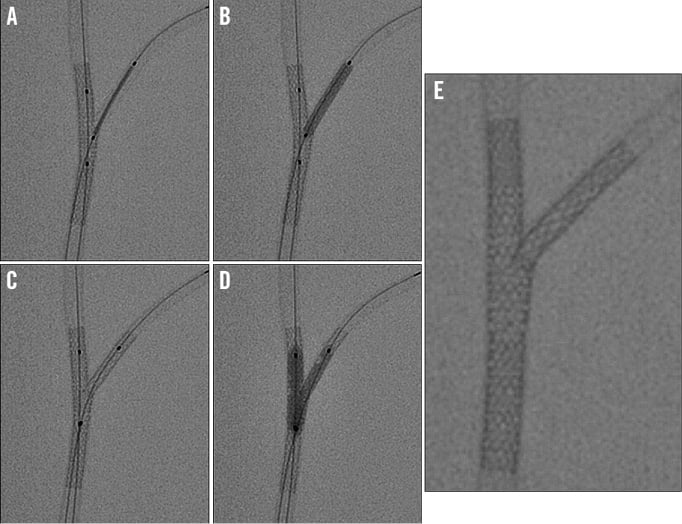
Figure 1. “Provisional” TAP technique step by step in a bench model. A) The stent for the side branch (SB) is placed with minimal protrusion in the MV and an uninflated balloon is prepared for final kissing in the MV. B) The SB stent is deployed with the main vessel (MV) balloon uninflated (Moving image 1). C) The balloon of the SB stent is pulled back to achieve perfect alignment with the MV balloon (Moving image 1). D) Kissing balloon inflation is performed with the SB stent’s balloon and the MV balloon (Moving image 1). E) Final result with TAP stenting (Moving image 1).
An anticipated pitfall of this technique is that a single layer “neocarina” is created by the SB stent struts protruding inside the MV at the level of the coronary bifurcation flow divider. Conversely, in the rest of the bifurcation area, TAP allows full stent coverage. A recent bench testing study comparing TAP with crush and culotte techniques showed that stent strut malapposition in the proximal vessel and the maximal wall-malapposed strut distance are significantly reduced by the TAP technique3.
During the practice of TAP stenting, the operator should pay attention to and try to limit as much as possible the protrusion inside the MV which influences the length of the neocarina. Nevertheless, two main determinants of neocarina length should be recognised: the SB take-off angle and the “quality” of pre-TAP kissing inflation.
The impact of the SB take-off angle is quite intuitive: when the SB has a “T” shape take-off, small or absent SB stent protrusion inside the MV is needed to cover the SB ostium successfully. On the other hand, acute SB angles (Y-shapes) are associated with longer, oval-shaped SB ostia. Such an anatomic configuration implies the need for wider protrusion of the SB stent inside the MV, resulting in a longer neocarina.
The “quality” of pre-TAP kissing balloon inflation is probably less recognised but may theoretically have similar relevance. Indeed, the site of the MV stent’s side cells recrossing with the guidewire is known to influence the SB ostium scaffolding after kissing4,5. In particular, wider MV stent strut scaffolding at the SB ostium site is obtained when kissing ballooning follows distal rewiring5. As a consequence, when implanting an SB stent according to TAP (especially in acute angled bifurcations), a limited need of protrusion inside the MV is achieved with distal rewiring followed by kissing balloon inflation (Figure 2).
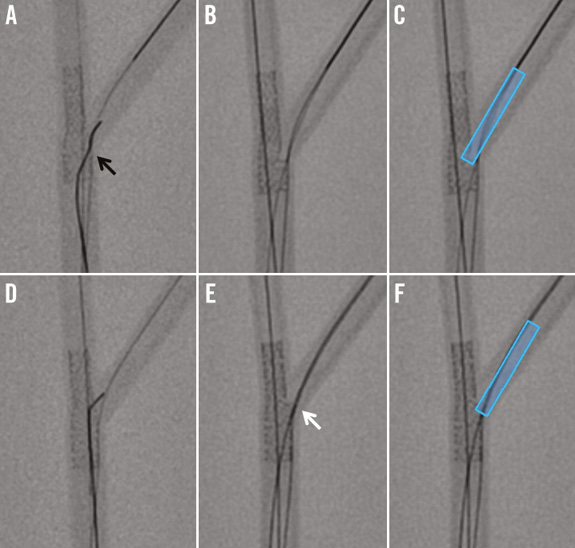
Figure 2. Impact of pre-TAP kissing balloon “quality” on neocarina length. Two situations (in a bench test) for TAP stenting in acute angled bifurcations: side branch proximal rewiring and kissing (A,B,C) versus side branch distal rewiring and kissing (D,E,F). A) Side branch (SB) rewiring is achieved through the most proximal stent struts (black arrow). B) After kissing, no side branch scaffolding has been achieved and stent struts are still in front (of the distal part) of the SB ostium. C) In such a situation, to achieve full ostium coverage, the tubular stent for TAP should be implanted deeply protruding inside the main vessel, thus generating a long neocarina. D) Side branch (SB) rewiring is achieved through the most distal stent struts using a pullback rewiring technique. E) After kissing, wide side branch scaffolding has been achieved (white arrow). F) In such a situation, to achieve full ostium coverage, the tubular stent for TAP can be implanted with minimal protrusion inside the main vessel thus generating a short neocarina despite the acute bifurcation angle.
Finally, it should be emphasised that a TAP-associated neocarina is highly mobile and often not easy to appreciate by angiography. Thus, if dilation of the proximal MV segment is needed after TAP (both immediately and/or in the case of repeat procedures), the balloon should not reach the bifurcation area in order to avoid unintended neocarina distortions. Moreover, when further MV and/or SB ballooning at the bifurcation site is needed, all dilations should be performed with balloons for final kissing already in place, since final kissing is recommended to ensure the “central” seating of the neocarina at procedure end.
Planning TAP in bifurcations with a high probability of double stenting requirement
In contrast to other techniques, such as crush or kissing stenting, the TAP technique has been designed to optimise SB stenting in the setting of provisional procedures. However, due to its effectiveness, TAP stenting has also started to be considered by some operators as a valuable technique to treat CBL, with the anticipated high probability of requiring double stenting. When planning a TAP stenting procedure in such high-risk anatomies (extensive disease, large SBs), the operator should aim to optimise the procedure course by carefully selecting the “operative” MV axis. As, by definition, it is necessary first to implant a stent across a major branch, it is mandatory to consider carefully the risk of “parent” branch closure after crossover stenting and to anticipate the easiness of “jailed” branch rewiring, dilation and stenting. In other words, TAP and so-called “inverted TAP”2 are selected on a case by case basis. As a consequence, the first stent is usually implanted from the proximal MV towards the vessel which is more diseased, larger and/or more difficult to wire, regardless of its nomenclature (either distal MV or SB). Figure 3 shows the procedure sequence to treat a patient with a complex distal left main lesion by “inverted TAP” successfully.
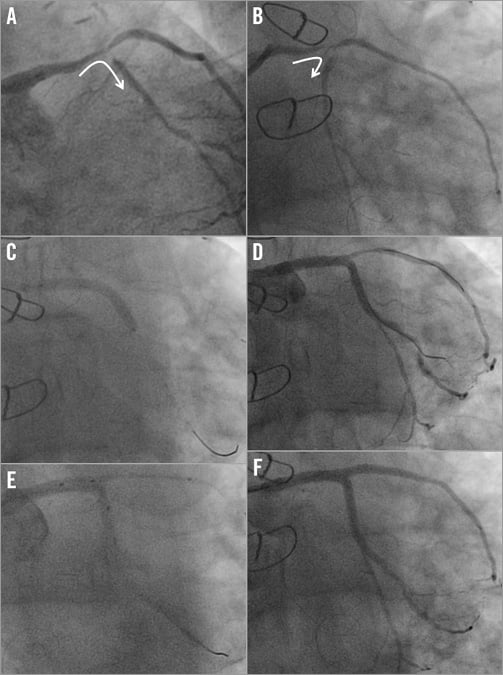
Figure 3. “Inverted” TAP to treat a complex bifurcation with high probability of double stenting being needed. A) & B) A patient with a complex lesion on the protected left main-left circumflex-ramus intermedius. Due to difficult access and more extensive disease, the left circumflex is selected as the “operative” main branch (white arrow). C) After predilation of both branches, the stent is implanted towards the left circumflex. D) After stenting, the relevant side branch (ramus) is patent and exhibits an easy-to-rewire configuration. E) After proximal optimisation technique (POT) followed by kissing inflation, TAP stenting is performed. F) Result after TAP stenting with final kissing inflation.
How to manage an eventual incorrect side branch stent positioning during TAP
A safe practice for any technique comprises the planning of strategies to overcome possible failures. The main difficulty of a “perfect” TAP stenting procedure is the selection of an appropriate site for SB stenting. An intravascular ultrasound study clearly documented the variability of neocarina length obtained in clinical practice with a mean length of 2.7±1.4 mm6.
In the case of a stent deployment site being unintentionally too distal, the failure to cover the ostium may be noticed. In such a circumstance, the operator may either accept the result or consider attempting another stent implantation according to TAP (Figure 4).
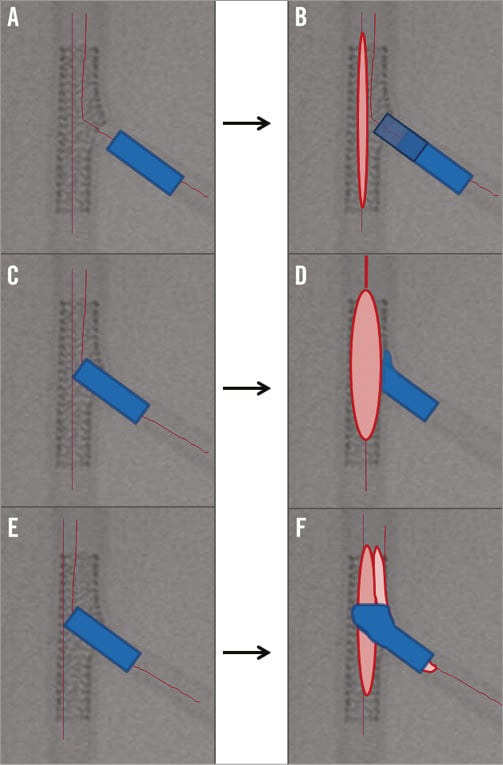
Figure 4. How to remedy incorrect stent placement in the course of TAP stenting. A) Too distal stent deployment site with failure to cover the ostium. B) Another stent implantation on the SB ostium may be performed according to TAP. C) Accidentally too long protrusion inside the MV. D) A balloon is advanced into the MV over the main vessel wire and dilated so that the protruding SB stent struts are crushed achieving the configuration of an “internal” crush. After crushing, SB rewiring and kissing balloon inflation should be performed to complete the procedure. E) Accidentally extremely long protrusion inside the MV with SB stent reaching the proximal MV stent segment. F) Failed TAP may be converted into a culotte technique by post-dilating the proximal MV and rewiring the distal MV in order to finish with a kissing balloon inflation.
The other main pitfall which may be encountered during TAP stenting is a protrusion inside the MV being accidentally too long. Once the SB stent has been implanted too far inside the MV so that the neocarina length is considered unacceptably long by the operator, two options may be considered. As shown in Figure 4, the protruding SB stent struts may be crushed by a balloon inflated into the MV achieving the configuration of an “internal” crush (Figure 4). After crushing, SB rewiring and kissing balloon inflation should be performed to complete the procedure. Finally, if the SB stent protrusion is extremely long so that the proximal SB stent is seated well inside the proximal MV stent segment, failed TAP may be converted into a culotte technique (Figure 4). To do this, the proximal part of the SB stent protruding inside the proximal MV should be ballooned with an appropriately sized balloon (to try to adapt it to the proximal MV size). Then, the distal MV should be rewired in order to finish with a kissing balloon inflation.
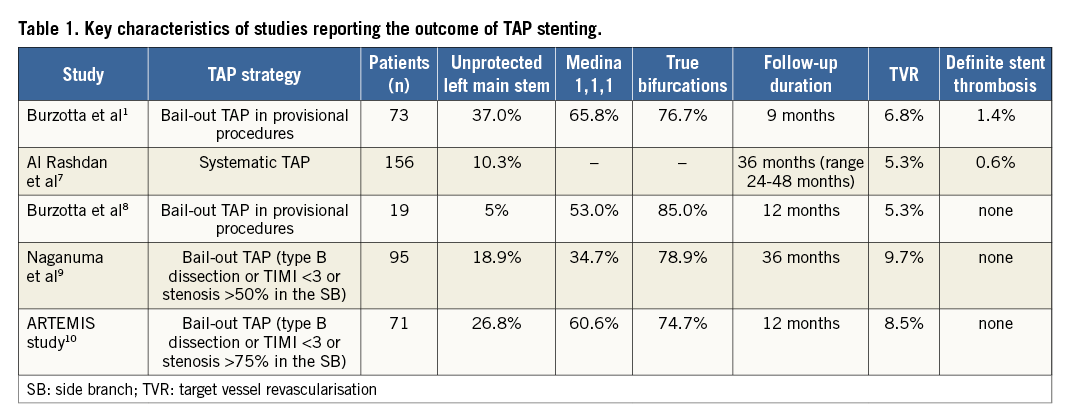
Updates on the clinical results of the TAP technique
Being relatively young, TAP stenting has not been selected as a technique to be investigated in any study design in the large prospective trials on CBL which have been conducted in recent years. However, some data regarding the outcome of patients treated by TAP have been published recently by independent groups1,7-10. The main characteristics and the clinical results reported so far are summarised in Table 1. Despite the overall high-risk pattern of the study populations enrolled, the reported clinical results look very promising11. Of note, intravascular ultrasound data showed that an optimal SB ostium dilation constitutes a critical issue with the TAP technique, since the SB ostium is the most frequent site of both post-procedural minimal stent area and largest neointimal formation6.
Recently, a strategy of systematic TAP stenting has been compared with simple stenting in a small single-centre prospective randomised trial conducted in China enrolling CBL patients with large SBs12. One-year clinical outcomes were similar and, at eight-month follow-up coronary angiography, the side branch binary restenosis rate was significantly lower with TAP (3.8% vs. 17.1% in simple stenting, p<0.05).
What about TAP with bioresorbable scaffolds?
The feasibility of T-stenting or TAP stenting with the first clinically available bioresorbable scaffold (BVS), Absorb (Abbott Vascular, Santa Clara, CA, USA), has been demonstrated in bench tests13. Of note, when adapting an Absorb BVS to the treatment of different bifurcation anatomies, its limited potential for stretching should be considered. A series of rules for the different steps (main vessel post-dilation, kissing balloon inflation) of bifurcation interventions has been reported14,15. The first experiences of TAP stenting with the Absorb have recently started to be reported. Seth et al successfully deployed a BVS through BVS side struts16 finishing with a full BVS TAP. Due to the huge Absorb strut thickness, the use of metallic DES for bail-out TAP has been advocated as an alternative strategy to deal with diseased SBs in the setting of provisional procedures with Absorb. Such an approach has recently been reported by Miyazaki et al, resulting in a “hybrid” coverage of the bifurcated lesion in which the neocarina is metallic17. New BVS devices with better expansion characteristics and lower profiles are expected to facilitate the performance of TAP in the future.
Conclusions
TAP stenting represents a valuable technique both for “bail-out” SB stenting during the “provisional” approach to CBL and for PCI in CBL with a high probability of requiring double stenting. This technique allows a complete coverage of the SB ostium and warrants final kissing inflation performance. Since TAP is associated with a single-layer stent strut neocarina of variable length, meticulous attention should be paid in order to optimise SB stent positioning.
Conflict of interest statement
F. Burzotta has been involved in advisory board meetings for Medtronic and has received speaker’s honoraria from Medtronic and Abiomed. M. Ferenc has received speaker’s honoraria from Biotronik, Eli Lilly, Abbott Vascular, Boston Scientific, Medtronic, and Biosensors. C. Trani has received speaker’s honoraria from Abiomed. The other authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. “Provisional” TAP technique step by step in a bench model.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Provisional TAP technique step by step in a bench model.

