Abstract
When transcatheter aortic valve implantation (TAVI) was first introduced in 2002, we could not have foreseen the central position it would come to occupy in the decision algorithm for aortic stenosis1. Since that time, we have learned a great deal from our collective experience with TAVI – from which patients are most appropriate, to mastering and improving each step of the procedure. The core philosophy of the strategy revolves around anticipating challenges and needs. Through the literature, meetings, live cases, and companioning, we understand better how to anticipate technical challenges to prevent complications and optimise procedural results. The evolution in technology and our understanding now allow us to tackle more challenging clinical scenarios and anatomy, such as TAVI for bicuspid aortic valves or for failed surgical bioprostheses23. The latter indication, namely valve-in-valve (ViV), carries with it a risk of coronary obstruction that is greater than for TAVI in native aortic valves. Coronary obstruction in ViV carries a very high mortality rate. Various techniques have been proposed to prevent or bail out coronary occlusion while performing ViV, including intentional leaflet laceration (BASILICA) or chimney stenting of the coronary ostia45. In order to determine the individual risk of coronary obstruction, it is necessary to integrate the height and location of coronary arteries, the width of the sinuses of Valsalva, the length and bulkiness of the coronary leaflets, particularly the location of the calcium, and the diameter of the sinotubular junction. Rather than using strict cut-off threshold measurements, it is recommended to integrate the device shape and diameter into the patient anatomy. Commissural alignment has recently been introduced as another factor influencing coronary obstruction. The ease of coronary cannulation also needs to be considered in anticipation of possible percutaneous coronary intervention post TAVI. This concern was always critical for the index procedure and will be more so for patients undergoing redo TAVI procedures (TAV-in-TAV). As the contemporary trend towards treating patients with a lower surgical risk profile and longer life expectancy continues to gain acceptance, coronary access will become a topic of frequent discussion for TAV-in-TAV cases. Therefore, there is a fundamental need to develop tools and provide guidance for systematic estimation of the risk of coronary obstruction for these patients.
In this issue of the journal, Tarantini et al6 seek to standardise the assessment of the difficulty of coronary cannulation post TAVI by defining the risk plane as the level under which the passage of a coronary catheter will be impossible after a second TAVI device is implanted.
They depict different scenarios depending on the location of the coronary ostia in relation to this risk plane, the type of prosthesis implanted during the index procedure, and the prosthesis options to maintain coronary access. They present an algorithm to predict the risk of acute coronary occlusion during the index TAVI procedure and the feasibility of future coronary catheterisation after TAV-in-TAV. They must be commended for this effort that will undoubtedly inform discussions with the current patients surviving their TAVI device and requiring a second procedure. Heart Teams will only see a growth in this cohort of patients as post-TAVI life expectancy continues to improve. This issue, that is fundamental to the future of TAVI, is addressed very well by the authors of the paper. Their hypotheses have to be validated in a prospective study that is ideally multicentric and includes most, if not all, of the available TAVI devices. In a recent study exploring TAVI in low-risk patients, Rogers et al found that TAV-in-TAV was probably not feasible in approximately 13% of their cohort, due to anticipated sinus sequestration7. These findings highlight the need for an established strategy to identify the patients at high risk of non-accessible coronary arteries post TAV-in-TAV. Apart from the issue of prosthesis durability, the issue of coronary access is central to our daily discussions for young and healthy TAVI candidates.
Chimney stenting for ViV seems be an effective strategy to prevent coronary obstruction. Encouraging short-term and midterm outcomes were observed in a collaborative registry. The intention to perform chimney stenting should ideally be decided upon prior to prosthesis deployment. Indeed, chimney stenting for impending or definitive coronary artery obstruction appears to be associated with poorer outcomes5. Could it be a realistic option for TAV-in-TAV? It is difficult to imagine stent patency being maintained between two layers of metallic prostheses. Benchtop testing would be required before application in humans for TAV-in-TAV. BASILICA is another technique for the prevention of coronary artery obstruction. The technique, though promising, is challenging to perform and is still considered an investigative technique. Its promising early results for ViV need to be explored in a large cohort of patients before validation for this indication4. Intuitively, even if we remain open-minded and imaginative, BASILICA seems hazardous for TAV-in-TAV.
Debate continues about what is the cut-off age after which TAVI can be considered the first-line option in younger patients. Consensus seems to exist for the 70-75-year age group if transfemoral TAVI is feasible with simple and favourable aortic root and peripheral vasculature anatomy. If TAVI ever emerges as an option for patients of 60-65 years (time will tell), the question of treatment sequence will remain central in the discussion: should we start with TAVI? Should we then schedule surgery at the time of prosthesis failure? Should we then perform ViV last in order to cover the lifespan of the patient and avoid TAV-in-TAV? This could be an option in patients at high risk for coronary occlusion post TAV-in-TAV. Imaginably, the highest risk setting for coronary occlusion would be TAV-in-ViV (Figure 1). A novel element in the discussion regarding treatment sequence will be the technical challenges inherent to transcatheter prosthesis explant after several years. Fukuhara and colleagues recently provided meaningful insights from a series of 15 explanted prostheses. They highlighted the technical difficulties of withdrawing the transcatheter valve, with a non-negligible proportion of patients requiring aortic root reconstructions8. In light of these warnings, it would be most prudent to wait for data from larger cohorts of patients with explanted devices before lowering the cut-off age for TAVI.
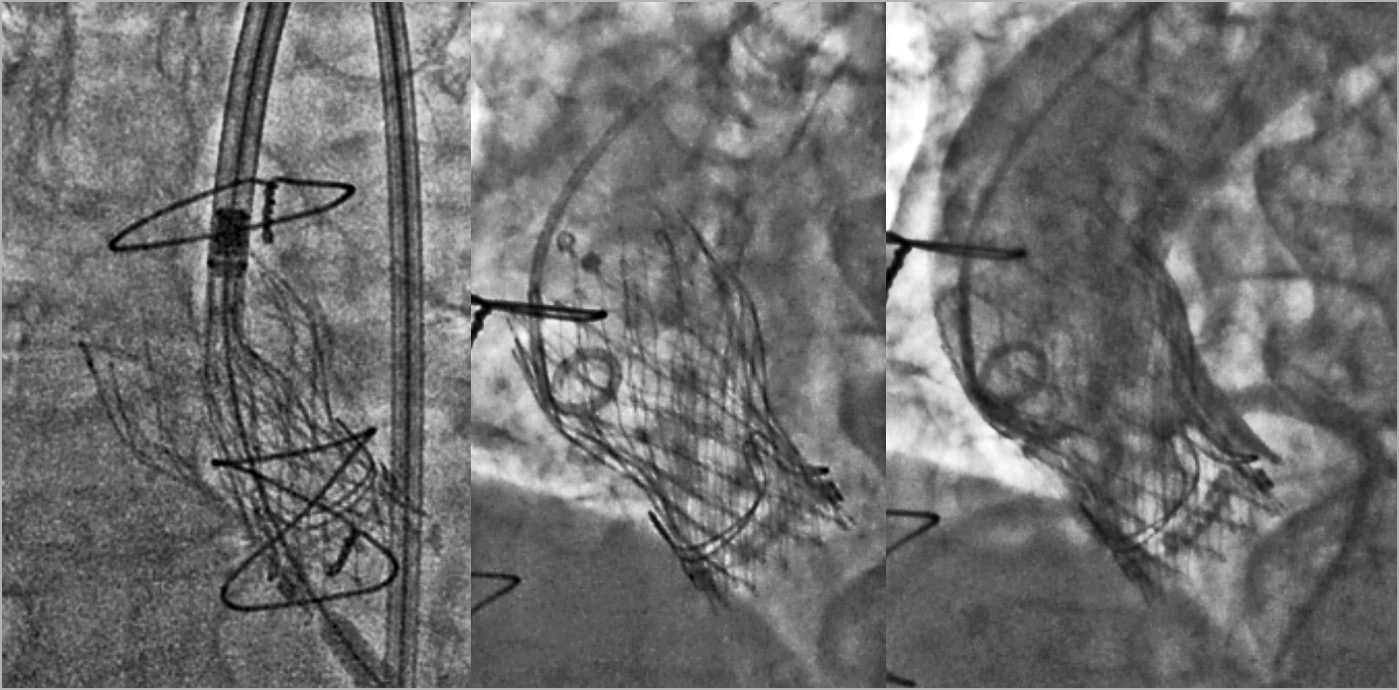
Figure 1. TAV-in-TAV for failed ViV, four years after the index procedure
Since the very first TAVI, we have observed constant refinement of prostheses and delivery systems which has translated into ever-improving outcomes for our patients. As a field, we will continue to forge this path to the future, with emerging devices facilitating TAV-in-TAV and reducing coronary occlusion risk. Promising technologies include shorter stent frames, thinner struts with open-cell design, failed-leaflet grasping technology, and smaller valves with larger effective orifice areas9.
In conclusion, there is, without a doubt, a bright future for TAVI as part of the central strategy for each aortic stenosis patient. Heart Teams will have to integrate the challenges of TAV-in-TAV when addressing younger patients. Algorithms to identify the individuals at higher coronary risk are needed. Tarantini and colleagues have paved the way for us with their excellent work.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.