Transcatheter aortic valve implantation (TAVI) was introduced as a less invasive alternative to surgical aortic valve replacement (SAVR) in patients with severe symptomatic aortic stenosis. After initially addressing patients at extreme or high surgical risk, TAVI has been shown to be non-inferior to SAVR with regard to mortality and disabling stroke in patients at intermediate surgical risk. These encouraging findings have led to trials comparing TAVI and SAVR in low-risk patients (NCT02675114, NCT02701283) and younger patients (NCT02825134). However, expanding TAVI to these patients is related with a number of potential issues, e.g., the higher prevalence of bicuspid aortic valves in younger patients, the long-term impact of permanent pacemaker and mild paravalvular leakage on ventricular function, as well as the durability of the bioprosthetic valves. In particular, durability is a major concern for TAVI in patients with longer life expectancy than the initially treated patients, who were often elderly with high comorbidity. It is well known that bioprosthetic aortic valves have limited durability. This is of particular concern in younger patients. Furthermore, a transcatheter heart valve (THV) prosthesis in a bicuspid aortic valve will be elliptical rather than circular, and this configuration may affect the durability of the bioprosthetic valve. The solution to THV deterioration may be to implant a new THV inside the failed one (TAVI-in-TAVI). However, as discussed below, this may add to the complex relationship between the bioprosthetic aortic valve and the coronary arteries in TAVI.
The coronary arteries may impact on the procedural outcome of TAVI both in native aortic valves and in failed surgical bioprosthetic aortic valves (TAVI-in-SAVR). In addition, subsequent access to the coronary arteries may become an issue after TAVI, and even impossible after TAVI-in-TAVI.
For TAVI in native aortic valves, the stent frame of the THV may cause occlusion of the ostia of the coronary arteries. This has mainly been described for balloon-expandable techniques, but is currently rare due to preprocedural risk stratification and procedural precautions. A preprocedural computed tomography scan is typically used to assess the length of the native aortic cusps, the width of the sinus of Valsalva, as well as the height from the aortic annulus to the take-off of the coronary arteries – all important morphological measures for the risk of coronary occlusion. Furthermore, a safety guidewire and non-expanded stent may be placed in the coronary artery in case of a TAVI procedure with predicted high risk of occlusion. Similar strategies have been applied for TAVI-in-SAVR, where not only stentless valves but also stented bioprostheses with leaflets sutured on the outside of the stents imply a higher risk of coronary occlusion.
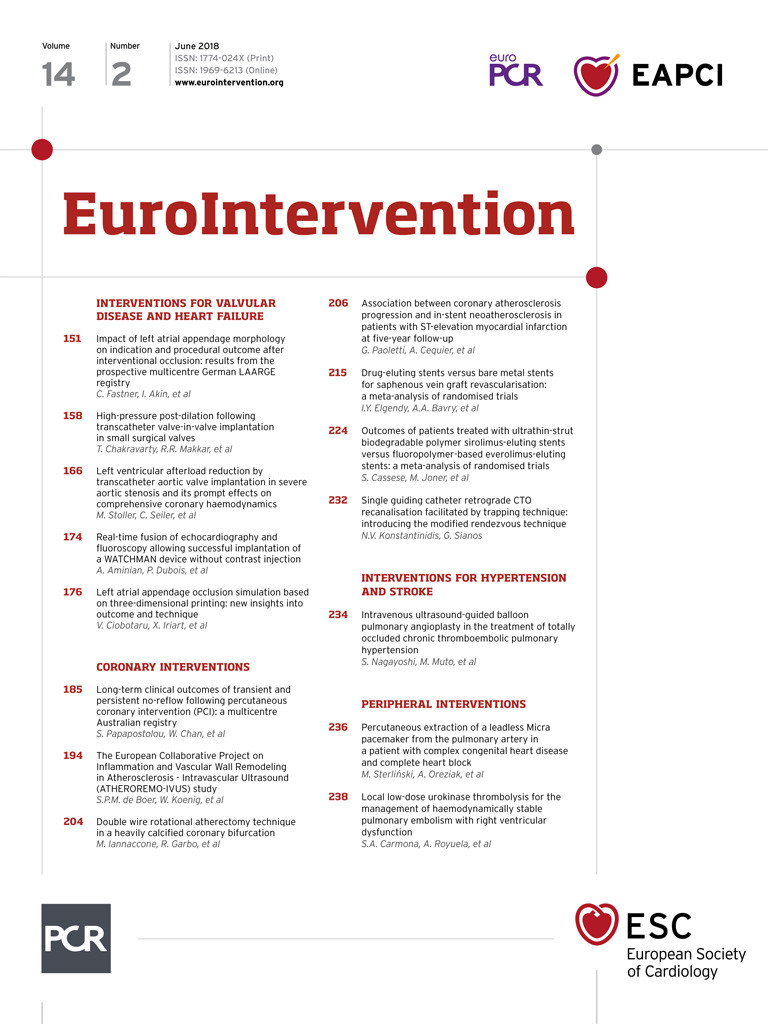
In patients with suspected ischaemic heart disease after TAVI, coronary angiography and percutaneous revascularisation may be challenging. If a low-frame THV with intra-annular leaflet position has been implanted, it is often possible to enter the sinus of Valsalva and coronary ostia with a catheter downstream from the stent frame (Figure 1A). This may be more challenging for high-frame THVs, since the catheter has to pass through the struts of the stent frame (Figure 1B, Figure 1C). However, access to the coronary arteries also depends on the alignment between the native aortic valve commissures and the THV commissures. In contrast to surgical bioprosthetic aortic valves, which are implanted aligned with the native commissures (Figure 2A), THV are orientated randomly. This means that, although a coronary catheter can be passed through the stent struts, the stent posts or leaflet suspensions of the THV may be orientated in front of the coronary ostia, thereby compromising the coronary access (Figure 2B).
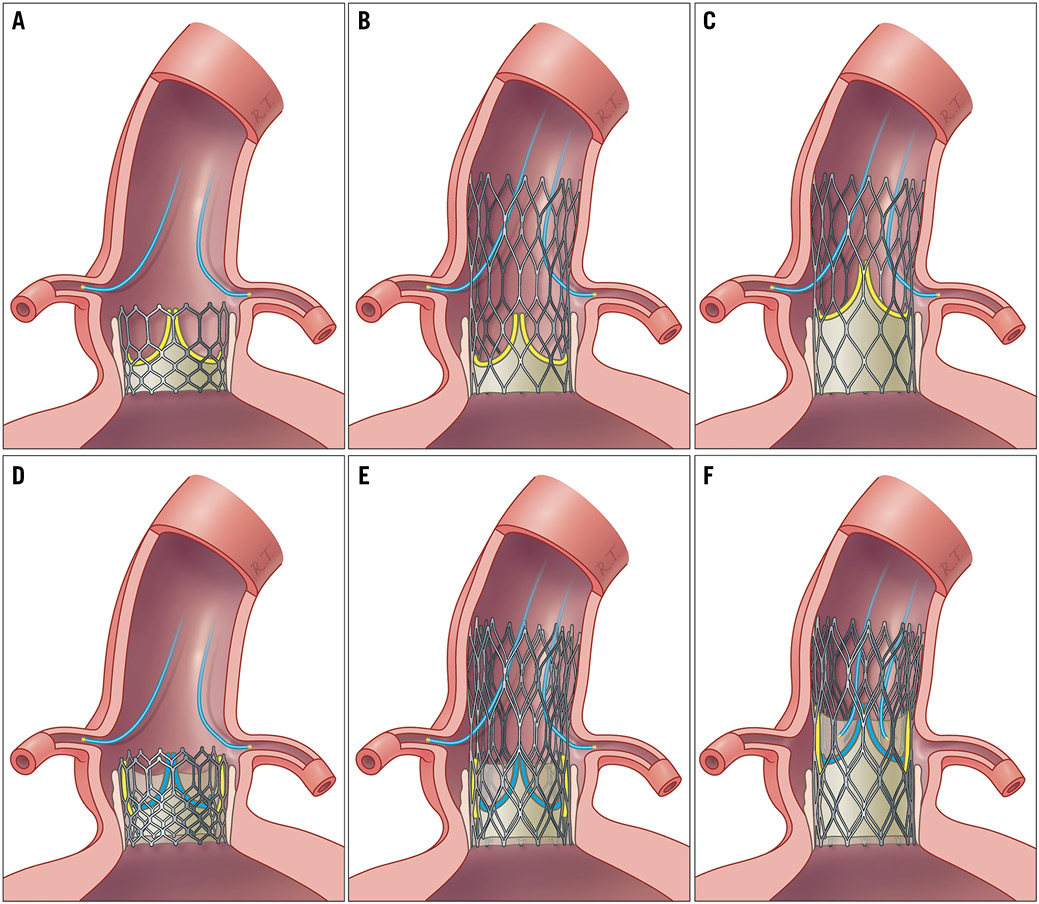
Figure 1. Access to the coronary arteries after TAVI and after TAVI-in-TAVI. Access to the coronary arteries after first transcatheter aortic valve implantation (TAVI) using a bioprosthetic valve with low-frame and intra-annular leaflet position (A), high-frame and intra-annular leaflet position (B), and high-frame and supra-annular leaflet position (C). After TAVI-in-TAVI, access to the coronary arteries may be possible in case of low-frame and intra-annular leaflet position (D) and high-frame and intra-annular leaflet position (E), whereas high-frame and supra-annular leaflet position (F) may compromise this. Yellow leaflets: leaflets in first implanted transcatheter heart valve. Blue leaflets: leaflets in second implanted transcatheter heart valve. Yellow/grey colour: tissue tunnel.
Figure 2. Commissural alignment and access to the coronary arteries. Commissural alignment between native and bioprosthetic aortic valve (A), and commissural misalignment (B).
Surgical bioprosthetic aortic valves are increasingly used in younger patients with severe aortic stenosis – often driven by a patient preference for avoiding anticoagulation therapy1. Based on the ongoing TAVI vs. SAVR trials, it is expected that TAVI will expand to these patients. In contrast to the initial patient cohort treated with TAVI, the life expectancy of younger and low-risk patients will exceed the durability of the THV. As an example, a 60-year-old low-risk patient who undergoes TAVI may have a life expectancy of approximately 25 years, whereas the THV may fail after 10 years. If this is solved by performing TAVI-in-TAVI, the patient will still have 15 years of life remaining. However, for some THV designs combined with patient anatomy, TAVI-in-TAVI may exclude future access to the coronary arteries for diagnostic and interventional purposes.
In case of implantation of a second stent frame inside the initial THV (TAVI-in-TAVI), the leaflets of the first bioprosthetic valve will be pushed up against the frame, thereby forming a tunnel of tissue. For low-frame THV with an intra-annular leaflet position, it may still be possible to access the sinus of Valsalva and coronary arteries downstream from the prosthesis (Figure 1D). For high-frame THV with an intra-annular leaflet position, the tissue tunnel created by the degenerated leaflets pushed up against the frame may not prohibit access to the coronary arteries through the struts (Figure 1E), although the overlay of the two frames may cause difficulties in case of small strut sizes. The scenario may be different for high-frame THV with a supra-annular leaflet position, where the tissue tunnel after TAVI-in-TAVI may extend from the aortic annulus through the sinus of Valsalva to even beyond the sinotubular junction. This implies that it may not be possible to access the coronary arteries in this TAVI-in-TAVI scenario (Figure 1F), which may be a major problem in case of acute coronary syndrome or unstable angina.
These issues need to be kept in mind when patients with long life expectancy undergo TAVI. The manufacturers, who are also seeking to target this market, must be dedicated to developing THVs or other solutions which address access to the coronary arteries in case of TAVI-in-TAVI. Based on laceration of the anterior mitral leaflet to prevent left ventricular outflow tract obstruction in mitral valve replacement2, lacerating the degenerated surgical bioprosthetic leaflets before TAVI-in-SAVR has been suggested in order to maintain access to the coronary arteries. However, for TAVI-in-TAVI, the success of this technique depends on the alignment of the native and bioprosthetic commissures (Figure 2). Currently, none of the THV systems is designed to secure this alignment routinely.
The interventionalist also has an obligation in terms of the choice of THV in order to optimise the chance of successful access to the coronary arteries a decade or two later in patients with long life expectancy. Currently, particularly a high-frame THV with a supra-annular leaflet position may complicate this. This is even the case if TAVI-in-TAVI is performed at a later stage with a low-frame inside a high-frame THV with a supra-annular leaflet position – the degenerated THV leaflets will still need to be pushed aside, thereby creating a long tissue tunnel.
During the last decade, TAVI has been a life-saving success story and is rightly predicted to play an even more important role in treating patients with aortic stenosis. However, new indications also call for new considerations.
Conflict of interest statement
The authors have no conflicts of interest to declare in relation to the editorial.