A 92-year-old female with prior transcatheter aortic valve implantation (TAVI) with a 26 mm CoreValve bioprosthesis (Medtronic) was admitted for worsening dyspÂnoea, home oxygen requirement, and a mean gradient of 39 mmHg, six years after the TAVI procedure. Transoesophageal echocardiography and computed tomography (CT) imaging showed no leaflet thrombosis but a severely calcified and degenerated transcatheter aortic valve (TAV).
Given her age and comorbidities, the patient was deemed to be at prohibitive risk for surgery. CT scans showed a high risk for sinus sequestration during TAV-in-TAV due to a low and narrow sinotubular junction (Figure 1A). Commissural misalignment of the initial TAV prohibited leaflet modification treatments. A Heart Team decision was made for chimney stenting (also called snorkel stenting) in both coronaries to preserve coronary patency. TAV-in-TAV was performed using a 23 mm SAPIEN 3 (S3) valve (Edwards Lifesciences) with the S3 outflow at CoreValve node 4 (Moving image 1). Chimney stenting successfully maintained coronary patency (Figure 1B, Moving image 2).
A clinical discussion of optimal cell access and concern for chimney stent deformation if stents were placed between the two TAV frames led us to retrospectively evaluate the clinical case on the bench. A heart valve pulse duplicator system (Heartroid [JMC Corporation]) and a 3D-printed patient-specific anatomy model were used (Figure 1C). A 26 mm Evolut R valve (Medtronic) was initially deployed, followed by the placement of 3.5x30 mm and 4.5x15 mm stents in the right and left coronaries, respectively. Coronary stents were wired through nodes 3-5 of the Evolut R valve, which placed them between the two TAV frames (Figure 1D). A 23 mm S3 valve was implanted with the S3 outflow aimed at Evolut R node 4; the final position was closer to node 5 (Moving image 3). After chimney stent deployment, the two TAV frames appeared to be crushing the left stent (Moving image 4). Post-dilation failed to fully resolve the left stent distortion. Fluoroscopic (Figure 1E) and micro-CT imaging (Figure 1F, Moving image 5) confirmed successful chimney technique of the right stent with external compression of the left stent.
The authors believe this work demonstrates the following: 1) coronary wires should be directed through the most superior index TAV cell feasible, 2) coronary stent cell-crossing height and second TAV placement are crucial for the procedural success of chimney stenting, and 3) preprocedural CT planning and in vitro models may help determine the optimal pathway for chimney stent placement during TAV-in-TAV.
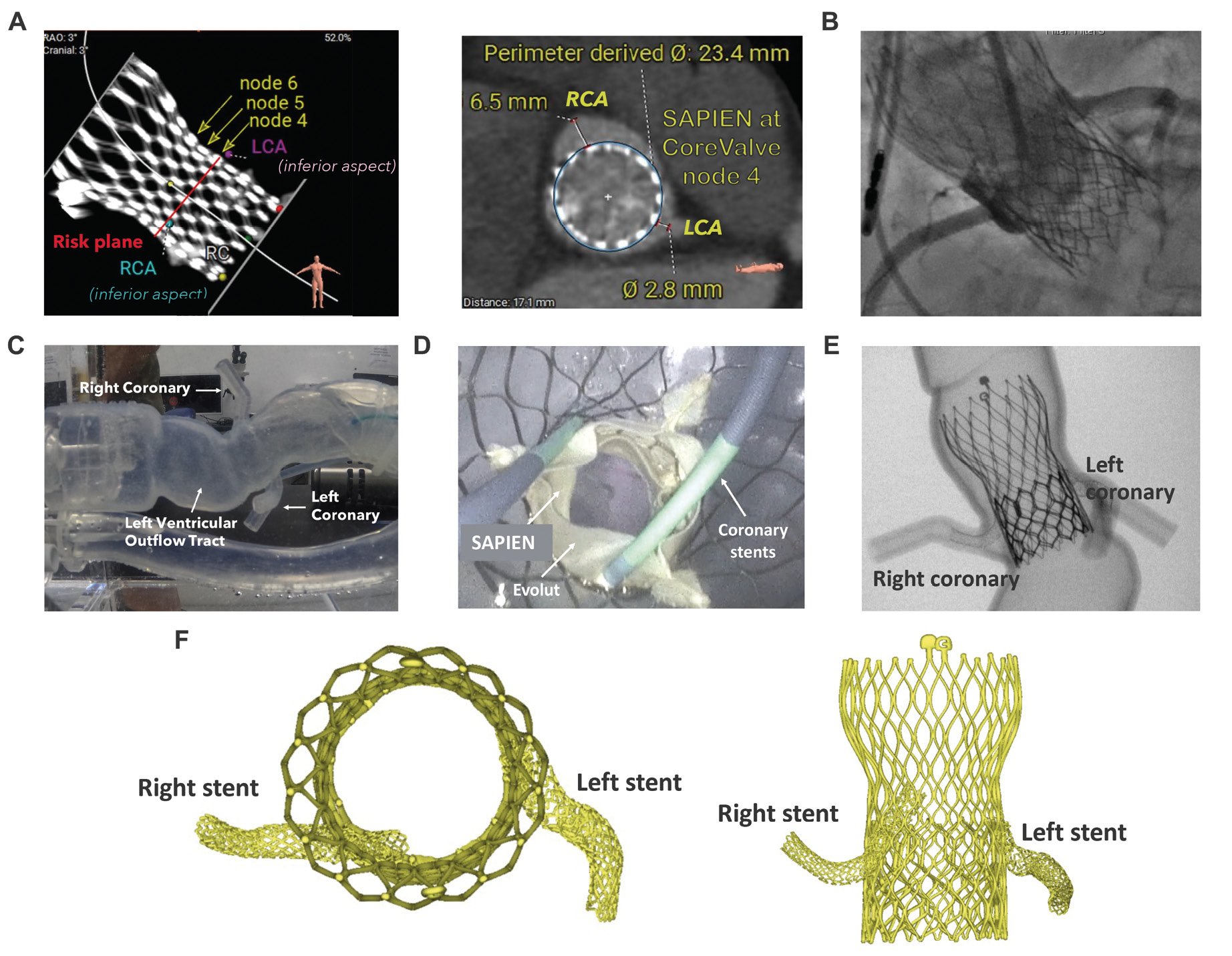
Figure 1. Chimney/snorkel stenting during TAV-in-TAV. A) CT case planning of TAV-in-TAV; B) Angiogram confirming coronary patency after chimney stenting during TAV-in-TAV; C) Patient-specific benchtop model; D) Coronary protection setup with guiding catheter, wire and undeployed coronary stents; E) Bench fluoroscopic image; and F) Micro-CT reconstruction. CT: computed tomography; LCA: left coronary artery; RCA: right coronary artery; TAV: transcatheter aortic valve
Acknowledgements
We gratefully acknowledge the technical contributions from Akankshya Shradhanjali, PhD, Jorge Zhingre Sanchez, PhD, and John Horrigan, PhD (all employees of Medtronic). Andres Caballero, PhD, and Sruti Bheri, PhD, (both employees of Medtronic) provided editorial support under the direction of the lead author.
Conflict of interest statement
C.L. Brown serves as a consultant to Medtronic. J. White serves as a consultant to Medtronic. C.T. Stinis is a speaker and proctor for Edwards Lifesciences. P.S. Teirstein receives speaking and consulting fees from Medtronic and Boston Scientific.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Deployment of a 23 mm SAPIEN 3 inside a 26 mm CoreValve. SAPIEN 3 deployment at CoreValve node 4. SAPIEN 3 rides up the left ventricular outflow tract despite forward force during deployment.
Moving image 2. Perfusion of right and left coronary arteries following TAV-in-TAV. Flow detected through both left and right coronaries after deployment of both chimney stents.
Moving image 3. In vitro deployment of a 23 mm SAPIEN 3 within a 26 mm Evolut R. SAPIEN 3 deployed between Evolut R nodes 4 and 5 after both left and right coronary stents were in position.
Moving image 4. TAV-in-TAV before and after coronary stent deployment. Top view of the SAPIEN 3 functioning within the index Evolut R and deployed left and right coronary stents.
Moving image 5. Micro-CT imaging of a 23 mm SAPIEN 3 within a 26 mm Evolut R after chimney stenting technique.