Introduction
Transcatheter aortic valve implantation (TAVI) is a therapeutic standard for patients with symptomatic severe aortic stenosis (AS) regardless of surgical risk. Although research on the long-term durability of transcatheter heart valves (THV) is still ongoing, the increasing number of TAVI performed in the last decade will inevitably lead to an important need to re-valve THV. The concept of lifetime management for younger patients undergoing TAVI has also become an essential tenet of contemporary clinical practice, in particular since transcatheter aortic valve (TAV)-in-TAV procedures have been associated with an increased risk of coronary obstruction12. In this research correspondence, we report on a state-of-the-art planning and execution of a TAV-in-TAV procedure to treat a degenerated ACURATE neo bioprosthesis (Boston Scientific).
Methods
A 74-year-old male who underwent TAVI with an ACURATE neo (size L) in 2017 presented with severe central aortic regurgitation and concomitant moderate AS. The self-expanding ACURATE neo platform features a supra-annular leaflet design with a “short stent” segment at the valve inflow and 3 stabilisation arches at the outflow. A meticulous multislice computed tomography (MSCT) analysis was performed to determine the position of the coronary ostia in relation to the ACURATE neo THV and to model the functional neoskirt – and, hence, determine the risk plane – in case of different implant depths of the second THV.
Results
Based on extensive bench test work (currently still in progress) and using computational modelling, it is thought that a balloon-expandable THV is likely to provide the optimal TAV-in-TAV result for a degenerated ACURATE neo. Both coronary arteries had ostia above the valve's upper crown (Figure 1A, Moving image 1). The outflow of the balloon-expandable THV should be positioned either at the top of the ACURATE neo upper crown (“low implant”) or at the base of the ACURATE neo commissural posts (“high implant”). We determined the optimal treatment strategy to be a balloon-expandable THV implantation in the low implant position (Figure 1B). Although more leaflet overhang can be expected, a lower neoskirt and maintained coronary access was anticipated. Key procedural aspects when performing a SAPIEN-in-ACURATE implantation are shown in Figure 1C and Moving image 2. First, we crossed the ACURATE neo valve with a pigtail catheter, thereby positioning the catheter within the stabilisation arches. To ensure intraluminal wiring of the ACURATE neo THV, a “swing test” should be performed in a fluoroscopic view in which 2 of the ACURATE neo commissural posts are overlapping. In this manoeuvre, the pigtail catheter needs to cross the 2 overlapping commissural posts at the left- and right-hand sides by manipulating the pigtail catheter. Next, a SAPIEN 3 (26 mm; Edwards Lifesciences) THV was positioned with the outflow part aligned with the upper crown of the ACURATE neo – this was verified using a right/left cusp overlap view, as this eliminated the parallax from both THV. Finally, the SAPIEN 3 valve was implanted under rapid pacing, resulting in good valve haemodynamics (no paravalvular or central regurgitation; mean gradient <10 mmHg) and preserved coronary access, as demonstrated by a selective left coronary artery ostium cannulation within 10 seconds using a Judkins left (JL) 4 catheter.
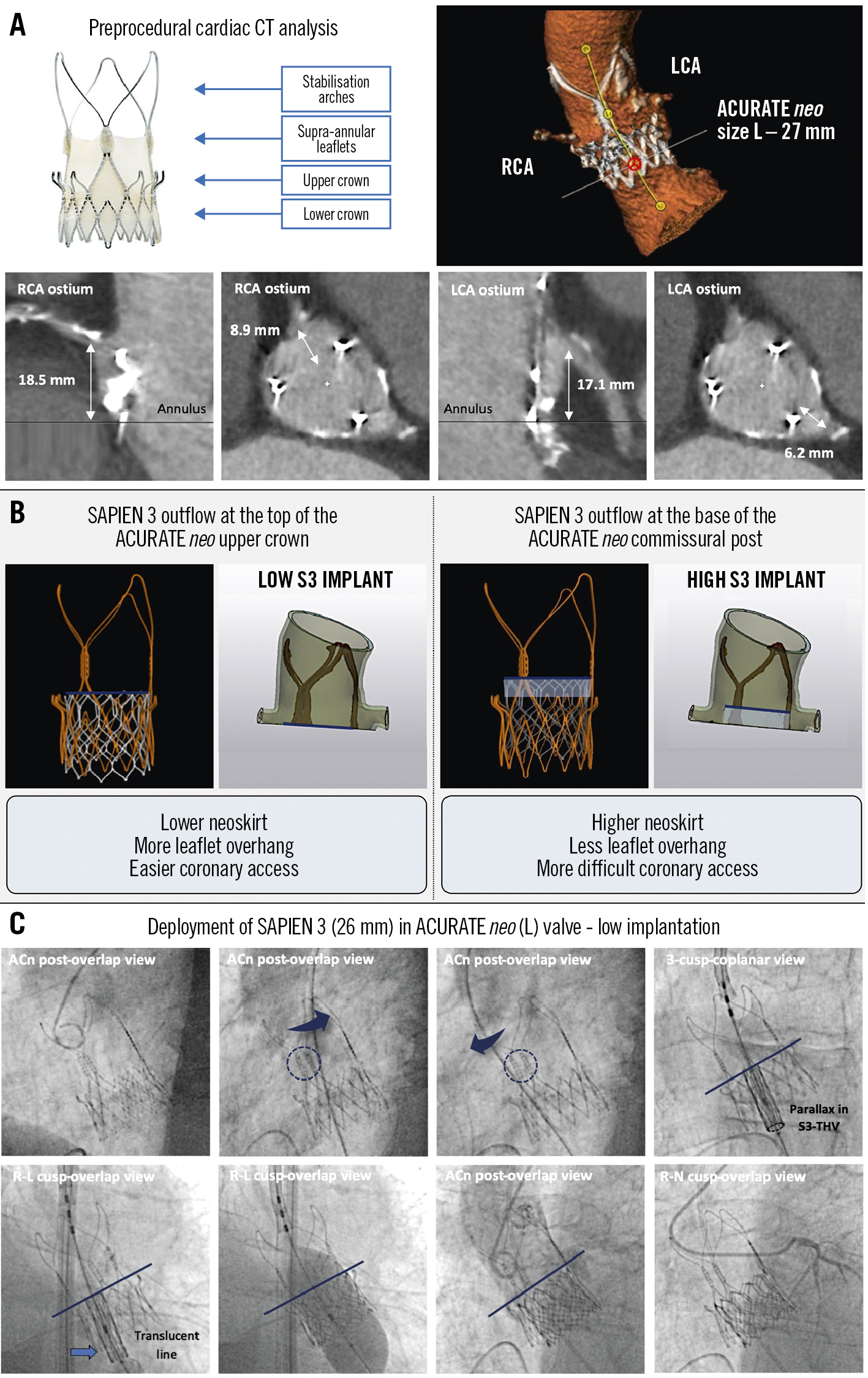
Figure 1. Planning and procedural aspects of TAV-in-TAV to treat a degenerated ACURATE neo valve with a balloon-expandable THV. A) Preprocedural cardiac CT analysis to determine the relation of the coronary artery ostia to the ACURATE neo THV. B) Patient-specific computational modelling showing coronary access in the case of a low and high SAPIEN implant. The risk plane, to which the neoskirt extends, is shown in dark blue. C) Crossing of the ACURATE neo THV using a pigtail and “swing test” and deployment of the SAPIEN 3 valve at a low implant position. ACn: ACURATE neo; CT: computed tomography; LCA: left coronary artery; RCA: right coronary artery; S3: SAPIEN 3; TAV: transcatheter aortic valve; THV: transcatheter heart valve
Discussion
TAV-in-TAV to treat a degenerated ACURATE neo using a balloon-expandable THV was safe and effective. Preprocedural MSCT analysis facilitates identification of the optimal second THV implant position, which – based on bench tests and computational models – is recommended to be between the upper crown and bottom of the commissural posts of the ACURATE neo.
Therefore, it is important to understand that the unique design of the ACURATE neo results in a neoskirt that is not deflected all the way to the outer dimensions of the THV. Most THV have a complete frame, and the leaflet is deflected all the way to the frame, forming the neoskirt. When implanting a SAPIEN 3 in an ACURATE neo, the neoskirt does not extend all the way to the end of the upper crown, and, hence, this gap helps to mitigate the risk of coronary obstruction and facilitates future coronary access. Another important aspect of the ACURATE neo is that it will not “overexpand” when performing TAV-in-TAV (including in the case of a SAPIEN-in-ACURATE), as shown in bench test work (in progress). Hence, sinus sequestration should only be a concern in the event that the stabilisation arches are seen touching either the aortic wall or sinotubular junction (STJ) on cardiac computed tomography (CT; in this case, the valve-to-STJ distance was more than 5 mm). Overall, these features in combination with the open stabilisation arches should facilitate coronary access, even in a scenario of commissural misalignment. Although the current TAV-in-TAV case was extensively modelled and tested preprocedurally and the clinical outcomes confirmed both bench tests and computational models, more real-world SAPIEN-in-ACURATE cases are needed to confirm these encouraging findings.
Conclusions
A state-of-the-art planning and execution of a TAV-in-TAV procedure to treat a degenerated ACURATE neo bioprosthesis relies on a meticulous preprocedural MSCT analysis.
Guest editor
This paper was guest edited by Franz-Josef Neumann, MD; Department of Cardiology and Angiology II, University Heart Center Freiburg - Bad Krozingen, Bad Krozingen, Germany.
Conflict of interest statement
The authors have no conflicts of interest to declare regarding this manuscript. The Guest Editor reports lecture fees paid to his institution from Amgen, Bayer, Biotronik, Boehringer Ingelheim, Boston Scientific, Daiichi Sankyo, Edwards Lifesciences, Ferrer, Pfizer, and Novartis; consultancy fees paid to his institution from Boehringer Ingelheim; and grant support from Bayer, Boston Scientific, Biotronik, Edwards Lifesciences, GlaxoSmithKline, Medtronic, and Pfizer.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Preprocedural CT tomography planning, showing moderate-to-severe coronary misalignment between the ACURATE neo and native aortic valve commissures.
Moving image 2. Angiography showing procedural aspects of implanting a SAPIEN 3 26 mm THV in an ACURATE neo (L) valve and the final result with easy coronary access.